Childbirth and Bipolar Disorder

In an abstract for virtual presentation at the 2020 meeting of the International Society for Bipolar Disorders, researcher Ian Jones presented evidence that childbirth may trigger onset of bipolar disorder.
Jones found that 15% of women who experience postpartum mood disorders shortly after childbirth will go on to develop bipolar disorder over time. A previous diagnosis of bipolar affective disorder is the biggest predictor that a woman will be readmitted for treatment of postpartum mental illness.
In addition, one of the biggest risk factors for postpartum mental disorders is a family history of bipolar disorder in first-degree relatives. The risk of postpartum mental disorders also increases when first-degree relatives have a psychiatric illness of any kind.
Editor’s Note: These data are consistent with research on sensitization/kindling, the idea that while early mood episodes may be triggered by psychosocial stress and other endocrine factors, later episodes may emerge more spontaneously. In this case, the stress associated with childbirth can lead to a subsequent bipolar diagnosis (with or without a precipitating stressor) in the future.
The psychosocial stress of childbirth and subsequent sleep deprivation can be severe, and those with a history of a mood disorder should seek additional support during such a time.
Environment Can Leave “Molecular Scars” Via Epigenetic Processes
A 2020 review article by researchers Julia Richetto and Urs Meyer in the journal Biological Psychiatry provides a good overview of the role epigenetic modifications play in schizophrenia and related disorders.
The article provides a powerful understanding of how the environment can induce long-lasting changes in the structure of DNA (not only in schizophrenia, but also in bipolar disorder). This process, known as epigenetics, can have life-long influences on brain chemistry and behavior, and remarkably, some of these epigenetic changes can even be transmitted to the next generation.
While the sequence of DNA that one inherits from one’s parents does not change over the course of one’s life, what can change is how loosely or tightly the DNA is wound around proteins called histones, making it easier or harder to transcribe the genetic material held there. The addition of a methyl group to DNA usually inhibits transcription, while the addition of an acetyl group to histones usually facilitates transcription. These alterations in the shape of the DNA that result from environmental exposures or behavior can be passed on through generations.
Richetto and Meyer describe these chemical changes to DNA as “molecular scars,” which are left when environmental stress occurs during sensitive developmental periods. For example, patients with schizophrenia who experienced stressors in early life have higher levels of the enzyme histone deacetylase than patients who had stress or trauma later in life. Histone deacetylase would remove the acetyl groups on histones, which would inhibit gene transcription.
Other factors that have been implicated in epigenetic modifications in schizophrenia, such as DNA methylation of key developmental pathways, include pre- or post-natal stress, a challenge to a mother’s immune system during pregnancy, pre- and post-natal nutrition, exposure to drugs or toxic substances, and cannabis use in adolescence.
Richetto and Meyer suggest that epigenetics may explain why schizophrenia (and we would add bipolar disorder) can differ so much across individuals, and may help researchers and clinicians determine how best to treat different individuals.
Editor’s Note: This editor has written about how epigenetic changes can mediate sensitization to the recurrence of life stressors, episodes of mood disorder, and bouts of substance abuse, each of which can drive illness exacerbation and progression in bipolar disorder (see the 2016 article by Robert M. Post in the journal Bipolar Disorders, “Epigenetic basis of sensitization to stress, affective episodes, and stimulants: implications for illness progression and prevention”).
The chemical changes to our DNA, histones, and microRNA emphasize how important it is to begin long-term preventative treatment starting after a first episode of mania. This not only helps limit episode recurrence and the accumulation of stressors and bouts of substance use that can cause illness deterioration, but also limit the placement of these “molecular scars” on our DNA. The key to treating bipolar disorder is: prevent episodes, protect the person and the brain.
Predicting Onset of Bipolar Disorder in Children at High Risk: Part I
 At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported.
At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported.
Symptom Progression
In offspring of parents with bipolar disorder, researcher Anne Cecilia Duffy found that symptoms in the children tended to progress in a typical sequence. Childhood sleep and anxiety disorders were first to appear, then depressive symptoms, then bipolar disorder.
Different Types of Illness May Respond Best to Different Medications
Duffy’s research also suggested links between illness features and a good response to specific medications. Those offspring who developed a psychotic spectrum disorder responded best to atypical antipsychotic medication. Those with classical episodic bipolar I disorder responded well to lithium, especially if there was a family history of lithium responsiveness. Those offspring with bipolar II (and anxiety and substance abuse) responded well to anticonvulsant medications.
If parents with bipolar disorder had experienced early onset of their illness, their children were more likely to receive a diagnosis of bipolar disorder.
The offspring of lithium-responsive parents tended to be gifted students, while those from lithium non-responders tended to be poorer students.
Comparing Risk Factors for Bipolar Disorder and Unipolar Depression
Researcher Martin Preisig and colleagues also showed that parental early onset of bipolar disorder (before age 21) was a risk factor for the offspring receiving a diagnosis of bipolar disorder. Parental oppositional defiant disorder (ODD) was also a risk factor for bipolar disorder in the offspring. The emergence of depression, conduct disorder, drug use, and sub-syndromal hypomanic symptoms also predicted the onset of mania during childhood.
Conversely, sexual abuse and witnessing violence were strong risk factors associated with a diagnosis of major (unipolar) depressive disorder. Being female and experiencing separation anxiety were also factors that predicted unipolar depression.
Predicting Conversion to Mania
Researcher Danella M. Hafeman reported that mood swings (referred to in the literature as “affective lability”), depression/anxiety, and having a parent who had an early onset of bipolar disorder were linked to later diagnoses of mania. Immediate risk factors that predicted an imminent onset of mania included affective lability, substance abuse, and the presence of sub-threshold manic symptoms.
Family Focused Therapy Effective in Youth at Risk for Bipolar Disorder Who Have Early Symptoms
 Researcher David Miklowitz developed Family Focused Therapy (FFT), in which families of young people at risk for bipolar disorder take part in therapy, learning about the illness and practicing strategies for communication and coping.
Researcher David Miklowitz developed Family Focused Therapy (FFT), in which families of young people at risk for bipolar disorder take part in therapy, learning about the illness and practicing strategies for communication and coping.
At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, Miklowitz reported findings from recent studies of youth who were at high risk for bipolar disorder because of a family history of the illness and the presence of early symptoms such as depression or cyclothymia or bipolar not otherwise specified (BP-NOS). Family focused therapy reduced symptoms. It also slowed onset of a first episode of mania and slowed the conversion to a diagnosis of bipolar I or bipolar II. These results converge with a total of 10 other positive studies of family focused therapy in different populations in children and adults. FFT or its equivalent should be made available to all symptomatic children who are at risk for bipolar disorder because of a family history of the disorder.
Potential Problems when Youth at Risk for Bipolar Disorder Take SSRIs
 At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Manpreet Singh reported that in youth at high risk for bipolar disorder, 53% had an adverse event while taking a selective serotonin reuptake inhibitor antidepressant (SSRI), and 26% had a new onset of suicidality while taking an SSRI. These adverse events were associated with reduced size and increased activation of the amygdala, the brain region responsible for emotion processing. Singh concluded that dysfunction in the prefrontal-limbic network may predict adverse events in children at risk for bipolar disorder when they are given SSRI antidepressants. She urged caution in the use of antidepressants in this population. Researcher Joseph Biederman echoed this caution later in the meeting.
At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Manpreet Singh reported that in youth at high risk for bipolar disorder, 53% had an adverse event while taking a selective serotonin reuptake inhibitor antidepressant (SSRI), and 26% had a new onset of suicidality while taking an SSRI. These adverse events were associated with reduced size and increased activation of the amygdala, the brain region responsible for emotion processing. Singh concluded that dysfunction in the prefrontal-limbic network may predict adverse events in children at risk for bipolar disorder when they are given SSRI antidepressants. She urged caution in the use of antidepressants in this population. Researcher Joseph Biederman echoed this caution later in the meeting.
Cannabis May Produce More Brain Changes in Teens with Bipolar Disorder than in Healthy Teens
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Benjamin Goldstein of Sunnybrook Research Institute in Toronto reported that adolescents with bipolar disorder who smoked marijuana had greater deficits in certain brain areas than did adolescents who did not have bipolar disorder. The areas affected included the dorsal lateral and rostral middle frontal cortex, and middle cortex. Goldstein concluded, “Adolescents with [bipolar disorder] may be particularly sensitive to the neurostructural effects of cannabis.”
Marijuana in general causes adverse changes in brain structure and cognition and vulnerability to paranoia and psychosis. Heavy use in adolescence is associated with an increased incidence of the onset of bipolar disorder and schizophrenia. The Goldstein data suggest several possible causal mechanisms. Those with bipolar disorder may already have brain abnormalities that are exacerbated by marijuana use. Alternatively, marijuana and bipolar disorder together may impact brain structure more than either factor alone would.
Psychiatric Risks in Offspring of Parents with Bipolar/Unipolar Disorders
 At the 2019 meeting of the International Society for Bipolar Disorders, researcher Martin Preisig and colleagues from Lausanne, Switzerland reported on a longitudinal study of mood disorders in offspring of parents with bipolar disorder, unipolar depression, or no history of psychiatric illness. The study included 446 children (with an average age of 10.1 years at the beginning of the study), who participated for an average of 11.9 years.
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Martin Preisig and colleagues from Lausanne, Switzerland reported on a longitudinal study of mood disorders in offspring of parents with bipolar disorder, unipolar depression, or no history of psychiatric illness. The study included 446 children (with an average age of 10.1 years at the beginning of the study), who participated for an average of 11.9 years.
Preisig and colleagues determined symptoms and other factors that preceded psychiatric illness. They found that bipolar disorder in the offspring was preceded by sub-threshold hypomania, major depression, and conduct disorder. Bipolar disorder in the offspring was also predicted by parental early-onset bipolar disorder.
Major depression was preceded by separation anxiety disorder, and witnessing violence or being a victim of sexual abuse.
Preisig and colleagues concluded that not only did bipolar disorder and major depressive disorder have different familial origins, they also had different antecedents and risk factors.
Comorbid Psychiatric Disorders Impair Response to Psychosocial Treatment in Adolescents with Bipolar Disorder
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Marc J. Weintraub and colleagues followed 145 adolescents with bipolar disorder over a period of two years. The adolescents with comorbid disorders (compared to those with bipolar disorder alone) fared more poorly in response to psychosocial treatment.
Weintraub and colleagues found that the adolescents who had anxiety disorders in addition to their bipolar disorder spent more weeks depressed, had more severe symptoms of (hypo)mania, and had more family conflict over the course of the study than those adolescents who had bipolar disorder alone.
Participants who had attention deficit hyperactivity disorder (ADHD) in addition to their bipolar disorder had more weeks with (hypo)manic symptoms, had more severe (hypo)manic symptoms, and greater family conflict than those with bipolar disorder alone.
Those participants with comorbid oppositional defiant disorder (ODD) or conflict disorder in addition to their bipolar disorder had more depressive symptoms and family conflict throughout the study.
Editor’s Note: How to better approach treatment in these diagnostically complex young people is an urgent unmet need, as most research excludes participants with more than one psychiatric disorder. Clinicians treating young people with bipolar disorder and comorbidities such as anxiety disorder, ADHD, and ODD must generally rely on inferences from children with these illnesses, using their own intuition about best treatment approaches rather than having evidence from systematic studies about how best to treat these children. It appears that both psychosocial and pharmacological treatments must be tailored to these more complicated presentations.
Lithium Reverses Thinning of the Cortex That Occurs in Bipolar Disorder
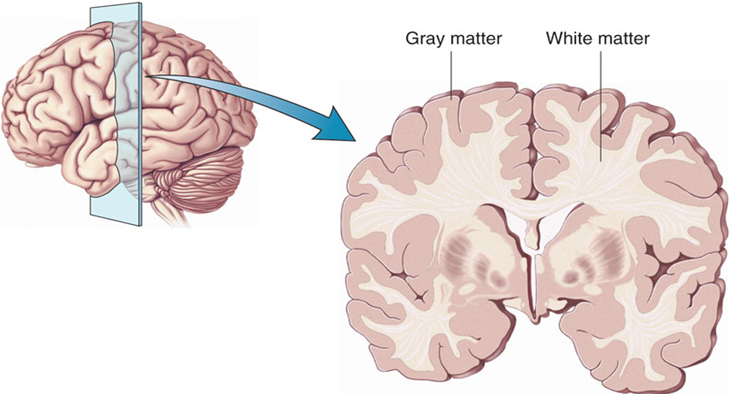
In a 2018 article in the journal Molecular Psychiatry, researcher Derrek P. Hibar reported findings from the largest study to date of cortical gray matter thickness. Researchers in the ENIGMA Bipolar Disorder Working Group, which comprises 28 international research groups, contributed brain magnetic resonance imaging (MRI) from 1837 adults with bipolar disorder and 2582 healthy control participants.
Hibar and colleagues in the working group found that in adults with bipolar disorder, cortical gray matter was thinner in the frontal, temporal, and parietal regions of both brain hemispheres. They also found that bipolar disorder had the strongest effect on three regions in the left hemisphere: the pars opercularis, the fusiform gyrus, and the rostral middle frontal cortex.
Those who had had bipolar disorder longer (after accounting for age at the time of the MRI) had less cortical thickness in the frontal, medial parietal, and occipital regions.
A history of psychosis was associated with reduced surface area.
The researchers reported the effects of various drug treatment types on cortical thickness and surface area. In adults and adolescents, lithium was associated with improvements in cortical thickness, and the researchers hypothesized that lithium’s protective effect on gray matter was responsible for this finding. Antipsychotics were associated with decreased cortical thickness.
In people taking anticonvulsant treatments, the thinnest parts of the cortex were the areas responsibly for visual processing. Visual deficits are sometimes reported in people taking anticonvulsive treatments.
Mounting Evidence of Mitochondrial Dysfunction in Bipolar Disorder
At the 2019 meeting of the International Society for Bipolar Disorders, researchers Ana Andreazza, Olivia Dean and colleagues reviewed substantial data that implicate mitochondrial dysfunction in the mood and energy fluctuations that make up bipolar disorder. Most of the neurobiological alterations known to occur in bipolar disorder have a relationship to mitochondria, which produce energy within cells. These alterations include abnormalities in glutamate, gene expression, apoptosis (cell death), oxidative stress, low ATP (a molecule that stores energy), altered ion pumps, increased intracellular calcium, and insufficient glutathionine (an antioxidant made up of three amino acids).
Coenzyme Q10 is a mitochrondrial enhancer of Complex I, an enzyme that is key to the first step in mitochondrial energy production. A 2018 controlled study by Maryam Mehrpooya and colleagues published in the Journal of Clinical Psychopharmacology found that 200mg/day of CoQ10 was more effective than placebo at reducing symptoms of bipolar depression when added to patients’ stable treatment regimens that included mood stabilizers and antidepressants. The effect size was large (0.87), and it took eight weeks for the benefit over placebo to appear. Response rate to CoQ10 was 72% compared to 12% to placebo.
Editor’s Note: Some formulations of CoQ10 do not cross the blood-brain barrier easily, so only a very small percentage of the CoQ10 gets into the brain. Thus, consumers should be careful about the type of product they purchase. The one made by Takeda Pharmaceutical Company is likely to be effective.