Certain Types of Inflammation and BMI Predict Depression
At the 2016 meeting of the Society of Biological Psychiatry, researcher Femke Lamers and colleagues presented findings from the Netherlands Study of Depression and Anxiety. The inflammatory markers interleukin-6 and CRP were elevated in people with current major depression. These measures were correlated with BMI, a measure of body weight. High levels of interleukin-6 at the beginning of the study predicted who would have a chronic course of illness.
Editor’s Note: Previous studies have found that elevated levels of CRP predicted a future mood episode in people at high risk for bipolar disorder due to a family history of the illness.
These studies suggest that it might be useful to assess levels of these inflammatory markers (CRP, interleukin-1, interleukin-6, and TNF-alpha) in young people who are at high risk for bipolar disorder. Factors that put someone at high risk include a family history of depression or bipolar disorder, a history of adversity in childhood (abuse, neglect, loss of a parent, etc.), and preliminary symptoms.
Several interventions are available that may reduce the likelihood that someone at risk for bipolar disorder will go on to develop the illness. Family interventions such as the Family Focused Therapy developed by researcher David Miklowitz are helpful. In a 2013 study in the Journal of the American Academy of Child and Adolescent Psychiatry, Miklowitz reported that Family Focused Therapy outperformed treatment as usual for youth at risk for bipolar disorder.
Measures of inflammation might provide additional rationale for beginning interventions in youth at high risk for mood disorders. In addition to family interventions, omega-3 fatty acid supplementation is a low-risk option that is supported by some positive data. Since BMI was implicated in the study by Lamers and colleagues, keeping weight under control might also have some benefit.
For adults with depression who want to keep their weight under control, the combination of the antidepressant bupropion XR (150–300mg/day) and naltrexone (50mg/day), an opiate antagonist medication normally used to fight addictions, has been effective.
Emotional Abuse Increases Inflammation
Trauma in childhood is a risk factor for depression, and both childhood trauma and depression have been linked to increased inflammation. In a study presented at the 2016 meeting of the Society of Biological Psychiatry, Sarah R. Horn and colleagues found that emotional abuse in childhood predicted high levels of inflammation measured in the blood in adulthood.
Horn and colleagues took blood samples from 35 people with treatment-resistant depression and 28 healthy control subjects. The researchers measured inflammatory markers in the blood and also interviewed the participants about any physical, sexual, or emotional abuse they experienced in childhood. Among all the participants, emotional abuse was linked to elevated levels of several inflammatory markers, including interleukin-6, interleukin-10, interleukin-1a, interleukin-15, and fractalkine.
The researchers suggest that more research is needed to clarify the link between early trauma, depression, and inflammation. How elevated inflammation in people with a history of abuse may influence the effectiveness of different psychotherapies and medications for depression remains to be determined.
Inflammation Linked to Non-Response to Antidepressants
In a symposium on inflammation’s role in psychiatric disorders at the 2016 meeting of the Society of Biological Psychiatry, researcher Carmine Pariante reviewed the considerable literature indicating that major depression is often associated with measures of inflammation. Depression has been linked to elevated blood levels of the inflammatory proteins interleukin-1, interleukin-6, TNF alpha, and c-reactive protein, with about one-third of depressed patients having an elevated level of at least one of these proteins. People with elevated inflammatory markers are also less likely to respond to traditional antidepressants such as selective serotonin reuptake inhibitors (SSRIs).
Pariante reported that in depressed people, interleukin-6 is also elevated in cerebrospinal fluid in addition to blood, suggesting that inflammation in depression extends to the central nervous system. Increased secretion of interleukin-6 has been linked to depressive behaviors in mice exposed to stress.
There is some hope that anti-inflammatory treatments can help patients who do not respond to traditional antidepressant treatment. Some anti-inflammatory medications that may eventually be used to treat depression with inflammation include the COX-1 inhibitor aspirin, the COX-2 inhibitor celecoxib (Celebrex), or the antibiotic minocycline. Each of these approaches gained some support in preliminary clinical trials, but it has not yet been established that these anti-inflammatory treatments produce a better response in people with elevated inflammatory markers.
Methylene Blue May Help Bipolar Depression
 We have previously reported on the research by Martin Alda and colleagues that the chemical compound methylene blue had positive effects in patients with bipolar depression. The research was published in the British Journal of Psychiatry in 2016.
We have previously reported on the research by Martin Alda and colleagues that the chemical compound methylene blue had positive effects in patients with bipolar depression. The research was published in the British Journal of Psychiatry in 2016.
Now a new article by Ashley M. Feen and colleagues in the Journal of Neurotrauma reports that methylene blue has an antidepressant-like effect in mice with traumatic brain injury (TBI). Methylene blue reduced inflammation and microglia activation in the animals. Methylene blue reduced levels of the pro-inflammatory cytokine Il-1b and increased levels of the anti-inflammatory cytokine Il-10.
These findings are of particular interest as many patients with classical depression (and no brain injury) have abnormal levels of these inflammatory markers. It remains to be seen whether methylene blue is more helpful in those patients with elevated inflammatory markers and if levels of the markers can predict treatment response or not.
Methylene blue causes urine to turn blue, so low doses of the compound are used as a placebo. Alda and colleagues reported that the active dose 195mg reduced depression and anxiety significantly more than the placebo dose (15mg) in a 13-week crossover study. In that study, methylene blue was added to lamotrigine which had not had a complete enough effect.
In a 1986 study by G.J. Naylor and colleagues in the journal Biological Psychiatry, patients were treated with either 15mg/day or 300mg/day of methylene blue for one year and crossed over to the other dose in the second year. Participants had significantly less depression during the year of taking the active 300mg/day dose.
The FDA has issued a warning about the danger of a serotonin syndrome if methylene blue is combined with serotonin active agents (presumably because it inhibits MAO-A). Symptoms of the serotonin syndrome can include lethargy, confusion, delirium, agitation, aggression, decreased alertness, and coma. Neurological symptoms, such as jerky muscle contractions, loss of speech, muscle tension, and seizures; or autonomic symptoms, such as fever and elevated blood pressure, are also common. Patients should call their doctor if they are taking a serotonergic psychiatric medication and develop any of the above symptoms.
Combination of SSRIs and Statins Better than SSRIs Alone
A large study in Denmark suggests that taking selective serotonin reuptake inhibitor (SSRI) antidepressants alongside cholesterol-lowering statin drugs improved depression more than SSRIs alone. The findings, by Ole Köhler and colleagues were reported in the American Journal of Psychiatry in 2016.
The study included 872,216 people in Denmark’s national health care database who took SSRIs between 1997 and 2012. The most common SSRIs were citalopram, sertraline, and escitalopram. Of these people taking SSRIs, 13.0% also took a statin drug, typically simvastatin. Those patients who were taking both an SSRI and a statin were less likely than those taking an SSRI alone to be hospitalized for any psychiatric problem, or for depression specifically.
Depression is known to be correlated with inflammation throughout the body. Statins reduce this inflammation as well as lowering cholesterol. A 2013 study by Ahmad Ghanizadeh and Arvin Hedayati in the journal Depression and Anxiety showed that the SSRI fluoxetine and the statin lovastatin reduced depression severity compared to fluoxetine alone.
The combination of SSRIs and statins did not seem to reduce deaths or suicidal behavior compared to SSRIs alone. Statins have some side effects, but combining them with antidepressants did not increase the risks associated with their use.
Inflammation Linked to Post-Stroke Depression
A 2016 study in the journal Psychoneuroendocrinology confirms that high levels of inflammatory cytokines in the blood are linked to higher risk of depression following a stroke.
The study, by Hee-Ju Kang and colleagues, followed 222 stroke sufferers for one year. Two weeks following the stroke, their levels of inflammatory cytokines IL-6 and IL-18 were measured. They were also assessed for depression both at the two-week point and one year later. The researchers also observed whether or not the participants were treated with statins, which are often prescribed to lower stroke risk and also have anti-inflammatory effects.
Those participants who had depression following their strokes (either at two weeks or at one year) tended to be older, to have a history of depression or stroke, to have a more severe stroke, and to have a stroke location toward the front of the brain.
Having any depression following the stroke was associated with higher levels of IL-6 and IL-18. This was particularly true of those participants who were not taking a statin. Among those taking statins, the statins may have interfered with the link between inflammatory cytokines and post-stroke depression. In the statin group, the only significant finding was a link between levels of IL-6 and depression at the two-week mark.
Lithium Treatment Reduces Inflammation, Mania-Like Behavior in Rats
Patients with bipolar disorder often show increases in signs of inflammation, including levels of the proteins IL-2, IL-4, Il-6, IL-10 and tumor necrosis factor in their blood. Lithium is the most effective treatment for bipolar disorder, but it is not yet clear how it works. A recent study by researcher Joao de Quevado and colleagues determined that lithium can reduce the same inflammatory markers in rats.
Rats were treated with amphetamine to induce mania-like behavior, which was accompanied by increases in some of the same inflammatory markers in the blood and brain that are increased in people with bipolar disorder. Lithium treatment reduced both the manic behavior and levels of these inflammatory proteins in the rats.
The researchers concluded that lithium may treat mania by reducing inflammation.
Diabetes Drug Pioglitazone May Improve Depression
 Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
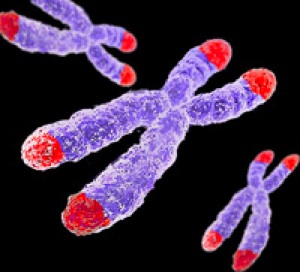
The study also touched on the role of telomere length in mental and metabolic disorders. Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect them during cell replication. Telomeres get shorter with aging and with psychiatric illnesses. In the study, telomere length was used to predict whether patients’ depression would improve.
Rasgon and colleagues found that in those patients taking both pioglitazone and antidepressant treatments (compared to those who received a placebo in addition to their antidepressants), longer telomeres predicted better antidepressant response. This suggests that telomere length could be used as a biomarker—that is, measuring a patient’s telomere length could reveal whether that patient’s depression is likely to respond to an anti-inflammatory treatment such as pioglitazone. The research was presented at a 2015 scientific meeting.
Yoga Therapy Improves Depression and Inflammation
Drug treatment for major depression can produce remission in 35–50% or patients. The others may need additional interventions, and some mind-body techniques have been successful. A recent randomized study by Anup Sharma and colleagues found that Sudarshan Kriya Yoga (SKY) decreased depression at one and two months when added to participants’ regular treatments. Participants who received the yoga treatment also showed reductions in inflammation in the blood, including lower levels of the inflammatory proteins TNF-alpha, IL-10, and CRP.
Anti-Inflammatory Treatments Look Promising for Bipolar Depression
Inflammation has been linked to both unipolar and bipolar depression. New research shows that anti-inflammatory treatments may reduce bipolar depression, for which few treatments exist.
Researchers led by Jonathan Savitz divided people with bipolar depression into four groups. One group received two placebos, another received minocycline (a drug with neuroprotective and immune-modulating properties) plus a placebo, the third received aspirin plus a placebo, and the final group received both minocycline and aspirin. Of the 64 participants, those who took both minocycline and aspirin were most likely to respond to treatment and to enter remission. In people with body mass indexes (BMIs) above the median of 30, a sign of greater inflammation, 100% of those who received both anti-inflammatory drugs responded to treatment, compared to 36% of those who received aspirin alone, 33% of those who received minocycline alone, and 25% of those who received two placebos.
Dosages of the drugs were 100mg twice a day for minocycline and 81mg twice a day for aspirin. Savitz and colleagues believe that aspirin and minocycline must work particularly well together, and are modifying their study to more directly compare use of the two anti-inflammatory drugs together to the absence of anti-inflammatory treatments.









