Lithium is a Lifesaver in Bipolar Disorder
Batya Swift Yasgur MA, LSW reported in Medscape Medical News on November 28, 2022 that “Mood stabilizers protect against suicide and all-cause mortality in patients with bipolar disorder (BD), including natural mortality, with lithium emerging as the most protective agent, new research suggests.
Investigators led by Pao-Huan Chen, MD, of the Department of Psychiatry, Taipei Medical University Hospital, Taiwan, evaluated the association between the use of mood stabilizers and the risks for all-cause mortality, suicide, and natural mortality in over 25,000 patients with BD and found that those with BD had higher mortality.
However, they also found that patients with BD had a significantly decreased adjusted 5-year risk of dying from any cause, suicide, and natural causes. Lithium was associated with the largest risk reduction compared with the other mood stabilizers.“
PREVENT EPISODES, PROTECT YOUR BRAIN, BODY, AND SELF
Kessing and Andersen 2017 wrote:”Overall, increasing number of affective episodes seemsto be associated with:(i) increasing risk of recurrence, (ii) increasing duration of episodes, (iii) increasing symptomatic severity of episodes,(iv) decreasing threshold for developing episodes, and (v) increasing risk of developing dementia.
Conclusion: Although the course of illness is heterogeneous, there is evidence for clinical progression of unipolar and bipolar disorder.”
These adverse outcomes emphasize the importance of early and sustained treatment to prevent the occurrence and accumulation of episodes.
Surface Area of Cortex Is Reduced After Multiple Manic Episodes
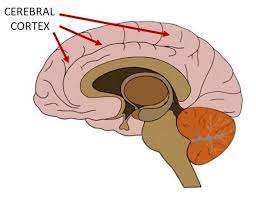
In a 2020 article in the journal Psychiatric Research: Neuroimaging, researcher Rashmin Achalia and colleagues described a study of structural magnetic resonance imaging (MRI) that compared 30 people with bipolar I disorder who had had one or several episodes of mania to healthy volunteers. Compared to the healthy volunteers, people with bipolar disorder had “significantly lower surface area in bilateral cuneus, right postcentral gyrus, and rostral middle frontal gyri; and lower cortical volume in the left middle temporal gyrus, right postcentral gyrus, and right cuneus.”
The surface area of the cortex in patients with bipolar I disorder who had had a single episode of mania resembled that of the healthy volunteers, while those who had had multiple manic episodes had less cortical surface area.
The data suggest that compared to healthy volunteers, people with bipolar disorder have major losses in brain surface area after multiple episodes that are not seen in first episode patients. In addition, the researchers found that both the number of episodes and the duration of illness was correlated with the degree of deficit in the thickness in the left superior frontal gyrus. These decreases in brain measures occurred after an average of only 5.6 years of illness.
Editor’s Note: These data once again emphasize the importance of preventing illness recurrence from the outset, meaning after the first episode. Preventing episodes may prevent the loss of brain surface and thickness.
Clinical data has also shown that multiple episodes are associated with personal pain and distress, dysfunction, social and economic losses, cognitive deficits, treatment resistance, and multiple medical and psychiatric comorbidities. These and other data indicate that treatment after a first episode must be more intensive, multimodal, and continuous and include expert psychopharmacological and psychosocial support, as well as family education and support. Intensive treatment like this can be life-saving. The current study also supports the mantra we have espoused: prevent episodes, protect the brain and the person.
Predicting Onset of Bipolar Disorder in Children at High Risk: Part I
 At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported.
At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported.
Symptom Progression
In offspring of parents with bipolar disorder, researcher Anne Cecilia Duffy found that symptoms in the children tended to progress in a typical sequence. Childhood sleep and anxiety disorders were first to appear, then depressive symptoms, then bipolar disorder.
Different Types of Illness May Respond Best to Different Medications
Duffy’s research also suggested links between illness features and a good response to specific medications. Those offspring who developed a psychotic spectrum disorder responded best to atypical antipsychotic medication. Those with classical episodic bipolar I disorder responded well to lithium, especially if there was a family history of lithium responsiveness. Those offspring with bipolar II (and anxiety and substance abuse) responded well to anticonvulsant medications.
If parents with bipolar disorder had experienced early onset of their illness, their children were more likely to receive a diagnosis of bipolar disorder.
The offspring of lithium-responsive parents tended to be gifted students, while those from lithium non-responders tended to be poorer students.
Comparing Risk Factors for Bipolar Disorder and Unipolar Depression
Researcher Martin Preisig and colleagues also showed that parental early onset of bipolar disorder (before age 21) was a risk factor for the offspring receiving a diagnosis of bipolar disorder. Parental oppositional defiant disorder (ODD) was also a risk factor for bipolar disorder in the offspring. The emergence of depression, conduct disorder, drug use, and sub-syndromal hypomanic symptoms also predicted the onset of mania during childhood.
Conversely, sexual abuse and witnessing violence were strong risk factors associated with a diagnosis of major (unipolar) depressive disorder. Being female and experiencing separation anxiety were also factors that predicted unipolar depression.
Predicting Conversion to Mania
Researcher Danella M. Hafeman reported that mood swings (referred to in the literature as “affective lability”), depression/anxiety, and having a parent who had an early onset of bipolar disorder were linked to later diagnoses of mania. Immediate risk factors that predicted an imminent onset of mania included affective lability, substance abuse, and the presence of sub-threshold manic symptoms.
Family Focused Therapy Effective in Youth at Risk for Bipolar Disorder Who Have Early Symptoms
 Researcher David Miklowitz developed Family Focused Therapy (FFT), in which families of young people at risk for bipolar disorder take part in therapy, learning about the illness and practicing strategies for communication and coping.
Researcher David Miklowitz developed Family Focused Therapy (FFT), in which families of young people at risk for bipolar disorder take part in therapy, learning about the illness and practicing strategies for communication and coping.
At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, Miklowitz reported findings from recent studies of youth who were at high risk for bipolar disorder because of a family history of the illness and the presence of early symptoms such as depression or cyclothymia or bipolar not otherwise specified (BP-NOS). Family focused therapy reduced symptoms. It also slowed onset of a first episode of mania and slowed the conversion to a diagnosis of bipolar I or bipolar II. These results converge with a total of 10 other positive studies of family focused therapy in different populations in children and adults. FFT or its equivalent should be made available to all symptomatic children who are at risk for bipolar disorder because of a family history of the disorder.
Quetiapine Reduced Childhood Mania, Especially in Those with Thicker Frontal Temporal Regions
 In a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Melissa P. Delbello reported that six weeks of treatment with either lithium or quetiapine was effective in childhood mania, but quetiapine had a higher response rate of 71% versus 46% for lithium. Delbello found two types of structural changes on functional magnetic resonance imaging (fMRI). Some children had thicker frontal temporal regions, while others had thinning in these areas. The first group of patients had a 100% response to quetiapine, but only 53% of the second group responded to quetiapine.
In a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Melissa P. Delbello reported that six weeks of treatment with either lithium or quetiapine was effective in childhood mania, but quetiapine had a higher response rate of 71% versus 46% for lithium. Delbello found two types of structural changes on functional magnetic resonance imaging (fMRI). Some children had thicker frontal temporal regions, while others had thinning in these areas. The first group of patients had a 100% response to quetiapine, but only 53% of the second group responded to quetiapine.
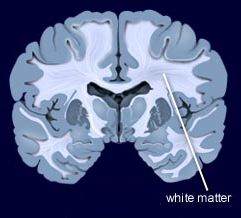
In contrast, other researchers have found lithium superior to quetiapine. Vivian Kafantaris showed that patients who respond well to lithium show improvements in white matter abnormalities. Michael Berk and colleagues found that a year on lithium was superior to quetiapine on all measures including cognition and brain imaging in patients having their first episode of mania.
In Mice, Knockout of Circadian CLOCK Genes Resembles Mania
Colleen McClung reviewed and extended previous findings of hers that knocking out a gene known as CLOCK in mice could reproduce most aspects of bipolar mania, including symptoms such as hyperactivity; decreased sleep; less depression; more impulsivity, risk taking, and novelty seeking; and increased reward-seeking including substances such as cocaine, alcohol, and sucrose. This syndrome in mice can be reversed by giving the mice lithium and valproate.
Knocking out the CLOCK gene produced an increased firing rate and burst firing of dopamine neurons in the ventral tegmental area (VTA). Localized knockout of the CLOCK gene in the VTA alone also reproduced the increase in dopamine cell firing.
When McClung and colleagues knocked out CLOCK in the medial prefrontal cortex, the normal development of a type of neurons called GABAergic parvalbumin interneurons did not occur in adolescent mice, and in adulthood, certain neural nets did not mature, leading to increases in oxidative stress, mitochondrial and cellular dysfunction, and the behavioral abnormalities that resembled mania. This animal model thus gives insight into how a genetic deficit in circadian rhythm genes in humans could influence the timing of behavioral abnormalities starting in adolescence and lasting through adulthood.
Links Between Mixed Depression, Insulin Resistance, Inflammation, and Cognitive Deficits
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Roger McIntyre discussed links between obesity, diabetes, and cardiovascular problems; increased inflammation; and decreased functioning of the neural networks involved in cognition.
He and his colleagues analyzed 121 studies that included empirical research and meta-analyses. McIntyre and colleagues found that patients with higher levels of inflammatory markers have more insulin resistance and cognitive dysfunction. A meta-analysis revealed that the inflammatory markers IL-6, TNF alpha, and CRP were significantly elevated in people with bipolar disorder compared to normal controls, while IL-1B was not.
People with depression who had a few manic traits (mixed depression) were particularly likely to have insulin resistance and elevated levels of pro-inflammatory markers.
People with mixed depression have increases in inflammation and increased incidence of cardiovascular disorder. People experiencing a first episode of mixed depression who are overweight show increased signs of brain aging.
In studies McIntyre and colleagues analyzed, diabetes or pre-diabetes occurred in 50% of depressed patients, and these patients had the greatest amount of cognitive dysfunction.
Treatment
McIntyre noted that taking the antipsychotic drug lurasidone for bipolar depression worked best in both adults and children who had elevated levels of CRP at baseline. The fast-acting antidepressant ketamine also works well in those who show baseline inflammation .
The anti-diabetes drug liraglutide (Victoza, Saxenda) improves mixed depression symptoms and cognition in obesity, diabetes, and mixed depression. Liraglutide belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists or incretin mimetics. They work by increasing insulin release from the pancreas and decreasing excessive glucagon release.
McIntyre now routinely uses liraglutide for cognitive deficits in patients with obesity or diabetes, including patients with mixed depression. It is injected under the skin at 0.6 mg daily, then the dosage is increased to 1.2 mg and then 1.8 mg. Victoza reduces major cardiovascular events in those with type 2 diabetes. The higher-dose Saxenda (3mg) can be used for weight control.
Another anti-diabetes drug, pioglitazine, has also been reported to be helpful in bipolar depression.
McIntyre found that the antibody infliximab, which can be used as an intravenous treatment for chronic inflammation and works by blocking the effects of TNF-alpha, did not improve depression, but did improve cognition.
McIntyre also supports the use of acetyl-L-carnitine, a potential adjunctive treatment that can reverse the insulin resistance that often occurs with obesity and thus could theoretically improve cognition.
McIntyre described preliminary literature suggesting the effectiveness of drugs such as statins, calcium channel blockers, and biguanides such as the diabetes treatment metformin in reducing inflammation.
Bariatric surgery to reduce the size of the stomach was another option discussed by McIntyre. He said the intervention is safe for patients with bipolar disorder and can help them recover cognitive function.
McIntyre noted that offspring of a mother with obesity have decreased response to sensory cues, reward preference, cognitive control, and motor control. Obesity and the inflammation that goes along with it apparently affect offspring via epigenetic mechanisms, meaning obesity may change the structure of inherited DNA (without changing its sequence).
Lithium FDA-Approved for Bipolar Disorder in Children 7–17
 In April 2019, the US Food and Drug Administration approved lithium for both the acute treatment of mania and for ongoing maintenance treatment of bipolar disorder in children and adolescents aged 7 to 17. Combined analysis of several studies indicates that lithium is effective and well-tolerated in both children and adolescents with bipolar disorder, both for acute treatment and to prevent bipolar episodes.
In April 2019, the US Food and Drug Administration approved lithium for both the acute treatment of mania and for ongoing maintenance treatment of bipolar disorder in children and adolescents aged 7 to 17. Combined analysis of several studies indicates that lithium is effective and well-tolerated in both children and adolescents with bipolar disorder, both for acute treatment and to prevent bipolar episodes.
Eating Beef Jerky and Other Nitrate-Cured Meats Linked to Increased Mania Risk
 In a 2018 article in the journal Molecular Psychiatry, researcher Seva G. Khambadkone and colleagues reported that a history of eating nitrated dry cured meat, such as beef jerky, was associated with a more than threefold increase in the risk of current mania. Eating other types of meat and fish products was not linked to mania.
In a 2018 article in the journal Molecular Psychiatry, researcher Seva G. Khambadkone and colleagues reported that a history of eating nitrated dry cured meat, such as beef jerky, was associated with a more than threefold increase in the risk of current mania. Eating other types of meat and fish products was not linked to mania.
The study included 217 people with mania, 91 with bipolar depression, 79 with unipolar depression, and 371 with schizophrenia, plus 343 control participants without a psychiatric disorder. Each participant responded to a questionnaire assessing whether they had ever eaten certain foods. The researchers had the idea that eating foods such as undercooked meat or fish, which might carry infectious agents, could be connected with mania, since inflammation seems to be linked to psychiatric illness. To the researchers’ surprise, their analysis found an independent link between eating nitrated dry cured meat (such as beef jerky, turkey jerky, or meat sticks) and being admitted to a hospital with acute mania.
Having eaten other cured meats such as salami or prosciutto was not linked to mania, nor was having eaten any other food.
Following these findings, Khambadkone and colleagues designed a study in which rats were given meat with added nitrate. The rats showed hyperactivity that resembled human mania, alterations in brain pathways that have been linked to bipolar disorder, and changes to gut microbes.



