Antipsychotics That Worked for A First Episode May Not Work As Well a Second Time
 In new research by Ofer Agid and colleagues, patients in their first schizophrenic episode who reached remission in response to one of two antipsychotic medications (risperidone or olanzapine) and relapsed due to medication non-adherence were re-treated with the same medication regimen that had brought about remission. Reinitiating the same treatment was not as successful in bringing about remission of the patients’ second psychotic episodes.
In new research by Ofer Agid and colleagues, patients in their first schizophrenic episode who reached remission in response to one of two antipsychotic medications (risperidone or olanzapine) and relapsed due to medication non-adherence were re-treated with the same medication regimen that had brought about remission. Reinitiating the same treatment was not as successful in bringing about remission of the patients’ second psychotic episodes.
Patients showed different types of trajectories in their first remission, from immediate to gradual improvement, and these predicted parallel trajectories of their treatment response during the second episode, though the muted response to antipsychotics existed across the board. Dopamine is the main target of antipsychotic treatments, but its role in schizophrenia is not straightforward, and Agid and colleagues stress that response and relapse are multidimensional processes.
Editor’s Note: These data are consistent with the research of J.A. Lieberman and colleagues fifteen years ago, which showed that response to antipsychotic treatment is poorer in successive episodes of psychosis. The findings are also consistent with the idea of episode sensitization in mood disorders, developed by this author (Robert Post). Episode sensitization refers to the case in which greater numbers of prior depressions or manias are associated with faster relapse and a greater degree of treatment resistance.
The data raise major doubts about the common practice of quitting medications to see if remission can be maintained without them. There are dozens of studies in patients with schizophrenia showing that continuous treatment is more effective than intermittent treatment.
Anti-Coagulants May Treat Psychosis
Schizophrenia is generally associated with a reduction in volume of the hippocampus. It is thought that the illness results from a predisposition that is triggered by an event such as a trauma or drug use that causes the release of chemicals that damage neurons. Recently, following the finding that five patients with schizophrenia and recurrent deep vein thrombosis (a blood clotting disorder) achieved remission of their psychosis after being treated with the anticoagulant warfarin (Coumadin) and have been able to go years with antipsychotic treatment, researchers Silvia Hoirisch-Clapauch and Antonio Egidio Nardi searched the existing literature for any connection between blood clotting and hippocampal neurogenesis, hoping to find a protein that could encourage neuronal growth in the hippocampus.
They found tissue-plasminogen activator (tPA), which facilitates the conversion of plasminogen to plasmin (the major enzyme responsible for breaking down blood clots) and plays a role in the repair of hippocampal neurons after stress. Low tPA activity is associated with clotting disorders and psychotic events. The drug warfarin reduces blood clotting, and also increases tPA activity, which may explain its effectiveness in treating the five patients who had both schizophrenia and deep vein thrombosis.
Abnormalities in schizophrenia that could be related to low tPA include deficient dopamine transmission at D1 receptors in the prefrontal cortex, impaired cleavage of the precursor to brain-derived neurotrophic factor (pro-BDNF, which can kill cells) to mature BDNF (which helps cells survive), abnormal NMDA receptor-mediated signaling, reduced Akt phosphorylation, and abnormal activation of reelin. The researchers found that all five patients had more than one tPA-related vulnerability to deep vein thrombosis, including high fasting blood insulin, high homocysteine, altered prothrombin activity, and anti-phospho-antibodies.
The same investigators have also examined whether plasmin plays a role in schizophrenia. Read more
Patients with Schizophrenia Have Short Telomeres, Atypical Antipsychotics Increased Telomere Length in Animals
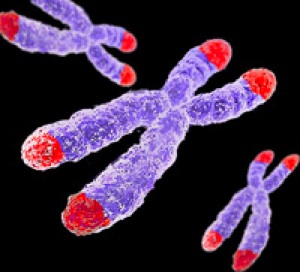 Telomeres sit at the end of DNA strands and shorten with each cell replication. A person’s percentage of short telomeres increases with aging. Telomeres also shorten with childhood adversity and as a function of number of depressive episodes.
Telomeres sit at the end of DNA strands and shorten with each cell replication. A person’s percentage of short telomeres increases with aging. Telomeres also shorten with childhood adversity and as a function of number of depressive episodes.
In a recent study, researcher Kazuya Torimi found that telomeres in white cells were shorter in 42 patients with schizophrenia compared to 56 healthy control participants.
Torimi also treated mice with various antipsychotics for 2-week periods. Treatment with atypical antipsychotics, such as risperidone, olanzapine and aripiprazole, but not typical antipsychotics like haloperidol, elongated telomere length in the hippocampus. This probably occurred through effects on serotonin.
Torimi suggests that atypical antipsychotics improve negative symptoms in part through the modulation of telomere length.
Editor’s Note: Lithium has been found to increase telomere length in patients with bipolar disorder, and appears to do this through a direct effect on telomerase, an enzyme responsible for adding to telomere length. Short telomeres are associated with a large number of medical and psychiatric illnesses.
N-acetylcysteine May Improve Prodromal Schizophrenia
 At the 2014 meeting of the International College of Neuropsychopharmacology, researcher N. Miyake described the effects of the nutritional supplement n-acetylcysteine (NAC) on clinical symptoms in subjects with subthreshold symptoms of psychosis.
At the 2014 meeting of the International College of Neuropsychopharmacology, researcher N. Miyake described the effects of the nutritional supplement n-acetylcysteine (NAC) on clinical symptoms in subjects with subthreshold symptoms of psychosis.
N-acetylcysteine, a glutathione precursor, has neuroprotective effects. In this case series, four patients with subthreshold psychosis were given 2000mg/day of NAC for 12 weeks. The patients’ symptoms improved to the point that three of the four were no longer considered at risk for psychosis.
Editor’s Note: These promising anecdotal observations deserve careful follow up using a control group. Omega-3 fatty acids have been show to slow conversion to full psychosis and performed better than placebo in a controlled study. Both n-acetylcysteine and omega-3 fatty acids should definitely be studied for those with emerging symptoms of bipolar disorder.
TDCS Promising for a Range of Illnesses
 Transcranial direct current stimulation (tDCS) shows promise for a range of problems. In new research presented at the 2014 meeting of the Society of Biological Psychiatry, it was reported to be effective for improving cognition in bipolar disorder, alleviating depression, and reducing hallucinations.
Transcranial direct current stimulation (tDCS) shows promise for a range of problems. In new research presented at the 2014 meeting of the Society of Biological Psychiatry, it was reported to be effective for improving cognition in bipolar disorder, alleviating depression, and reducing hallucinations.
How TDCS Works
At the meeting, researcher Marom Bikson discussed tDCS technology. The treatment can be delivered with a 12-volt battery. The anode directs current inward and is excitatory, while the cathode directs current outward and is inhibitory. The dendrites at the top of neurons under the anode are hyperpolarized by the tDCS, leading to relative depolarization of the cell soma, thus increasing excitation. TDCS, unlike repetitive transcranial magnetic stimulation (rTMS), which causes cells to fire, is only neuromodulatory, inducing minor changes in membrane polarization.
TDCS Improved Cognition in Bipolar Disorder
At the 2014 meeting of the American Psychiatric Association, Roberto Delle Chiaie et al. reported that two mA tDCS for 20 minutes for 15 days (anode over the left prefrontal cortex and cathode over the right cerebellum) improved immediate and delayed recall, trail making with a pointer, and motor coordination in 17 euthymic bipolar patients. This very promising result deserves further study and replication.
Antidepressant Effects of TDCS
At the 2014 meeting of the Society of Biological Psychiatry, Collen Loo reported that tDCS had positive effects in depressed patients compared to sham treatment. This complements a 2013 article by Brunoni et al. in JAMA Psychiatry that tDCS plus the selective serotonin reuptake inhibitor (SSRI) antidepressant sertraline (Zoloft) was more effective than either treatment alone.
TDCS for Treatment-Resistant Hallucinations
Jerome Brunelin et al. reported at the meeting that tDCS had positive effects in patients with schizophrenia who had hallucinations that resisted treatment. The positive electrode (anode) was placed over the left prefrontal cortex and the negative electrode (cathode) over the left temperoparietal area, where hallucinations are thought to originate. Stimulation was at two mA for 20 minutes, five days per week for two weeks. Effects lasted as long as 30 days and were associated with reduced functional connectivity of these brain regions.
Low frequency (1Hz) rTMS, which decreases neural activity, also improves refractory hallucinations when applied over the temperoparietal area, which is important for language. Placing the cathode over this area in tDCS is also inhibitory, so comparisons of rTMS with tDCS for suppressing hallucinations would be of great interest and importance.
Vitamin D Important for Brain Function, and Often Deficient
Vitamin D plays an important role in many brain functions, including synapse creation, calcium signaling, reduction of free radicals, neurotransmitter production, immune regulation, and brain development. Deficiencies in vitamin D have been linked to depression and schizophrenia. Some research has suggested that vitamin D supplementation can improve depressive symptoms, but there is still debate about a possible role for vitamin D in treating bipolar disorder.
At the 2014 meeting of the International Society for Bipolar Disorders, researcher Baseok Cha discussed the importance of vitamin D supplementation in bipolar patients, who often have deficient or insufficient levels. People receive 50 to 90% of their vitamin D from sunlight, and the rest from diet and supplements. Too much sunscreen can be a problem if it prevents a person from receiving enough vitamin D from sunlight.
The type of vitamin in supplements, D3, is converted to 25 hydroxy vitamin D in the liver, and then to 1,25 hydroxy vitamin D in the kidney. Levels of 25 hydroxy vitamin D below 20 indicate deficiency while levels between 20 and 29 indicate insufficiency. Low levels of 25 hydroxy vitamin D3 in newborns is a risk factor for schizophrenia, and vitamin D supplementation reduces this risk. Fish oils increase vitamin D, and it is possible that some of the therapeutic effects of omega-3 fatty acids in depression relate to vitamin D.
Two out of four recent studies of vitamin D supplementation have been positive, the last by Khoraminya et al. in the Australia and New Zealand Journal of Psychiatry in 2013, in which daily doses of 1,500 IU were used. Cha et al. found significantly lower levels of 25 hydroxy vitamin D in a Korean study of 21 patients with schizophrenia, 86 patients with bipolar disorder, and 42 patients with depression (mean levels about 15 µg/ml) compared to 31 controls (mean levels about 20 µg/ml).
Marijuana Addiction Associated with White Matter Loss and Brain Changes in Healthy People and Those with Schizophrenia
It has been established that cannabis use is associated with impairments in working memory, but researchers are still investigating how these impairments come about. A 2013 study by Matthew J. Smith et al. in the journal Schizophrenia Bulletin compared regular marijuana users both with and without schizophrenia with demographically similar people who did not use marijuana.
Using magnetic resonance imaging (MRI), the researchers were able to map each participant’s brain structures. Healthy people who were marijuana users showed deficits in white matter (axons of neurons that are wrapped in myelin) compared to healthy people who did not use the drug. Similarly, patients with schizophrenia who used marijuana regularly had less white matter than those patients with schizophrenia who did not use the drug. There were also differences in the shapes of brain structures, including the striatum, the globus pallidus, and the thalamus, between cannabis users and non-users.
Differences in the thalamus and striatum were linked to white matter deficits and to younger age of cannabis use disorder onset.
Differences between cannabis users and non-users were more dramatic across the populations with schizophrenia than across the healthy populations.
Editors note: Future research is needed to determine whether marijuana causes these brain changes, or whether the brain changes are a biomarker that shows a vulnerability to marijuana addiction (although the latter is less likely than the former).
Other data show that marijuana is associated with an increase in psychosis (with heavy use), cognitive deficits, and an earlier onset of both bipolar disorder and schizophrenia in users compared to non-users. These findings make pot begin to look like a real health hazard. With legalization of marijuana occurring in many states, ease of access will increase, possibly accompanied by more heavy use. The most consistent pharmacological effect of marijuana is to produce an amotivational syndrome, characterized by apathy or lack of interest in social activities. Particularly for those already struggling with depression, pot is not as benign a substance as it is often thought to be.
Ginkgo Biloba Improves Tardive Dyskinesia
 Tardive dyskinesia is a sometimes irreversible side effect of antipsychotic treatment, and is characterized by uncontrollable, subtle and spontaneous motor movements, usually of the tongue, mouth, or fingers.
Tardive dyskinesia is a sometimes irreversible side effect of antipsychotic treatment, and is characterized by uncontrollable, subtle and spontaneous motor movements, usually of the tongue, mouth, or fingers.
Extracts of the leaves of the gingko biloba tree contain potent antioxidants. In a study published by Zhang et al. in the journal Biological Psychiatry in 2012, treatment with ginkgo biloba (EGb-761) at 240mg/day for 12 weeks improved tardive dyskinesia more than placebo. Patients with tardive dyskinesia had low levels of brain-derived neurotrophic factor (BDNF) at baseline, and gingko biloba increased these levels. BDNF is important for the production and protection of neurons, and maintaining long-term memory.
The increase in BDNF was correlated with the degree of improvement achieved with gingko biloba in these patients. Different people have different variations in the gene for BDNF. As a result, some people’s BDNF is transported to dendrites and synapses more efficiently than others’. Improvement was greatest in those patients with the most common and best-functioning variant of BDNF, Val66Val, and worst in those patients with the rare and poorest-functioning variant, Met66Met.
Editor’s Note: These findings could be of great clinical importance. Tardive dyskinesia occurred in 20 to 40% of patients with bipolar disorder following treatment with the older “typical” antipsychotics. The incidence is much lower with the newer “atypical” antipsychotics, but having an effective and well-tolerated treatment for this disfiguring side effect is an extra bonus.
Metformin Effective for Treating Antipsychotic-Induced Amenorrhea, Weight Gain, and Insulin Resistance in Women
 Treatment with antipsychotics often has side effects such as amenorrhea (loss of the menstrual period) and weight gain that make sticking to a treatment regimen difficult for some patients. A 2012 study by Wu et al. in the American Journal of Psychiatry suggests that the drug metformin, often used to treat diabetes, can reverse these changes. The 84 female patients recruited for the study were being treated for a first episode schizophrenia, were on one antipsychotic, and had experienced amenorrhea for several months. They received either placebo or 1000mg/day of metformin in addition to their antipsychotic treatment for six months. Seventy-six women completed the trial.
Treatment with antipsychotics often has side effects such as amenorrhea (loss of the menstrual period) and weight gain that make sticking to a treatment regimen difficult for some patients. A 2012 study by Wu et al. in the American Journal of Psychiatry suggests that the drug metformin, often used to treat diabetes, can reverse these changes. The 84 female patients recruited for the study were being treated for a first episode schizophrenia, were on one antipsychotic, and had experienced amenorrhea for several months. They received either placebo or 1000mg/day of metformin in addition to their antipsychotic treatment for six months. Seventy-six women completed the trial.
Metformin was able to reverse the side effects in many of the women. Menstruation returned in 28 of the patients taking metformin compared to only two patients taking placebo. Among those on metformin, body mass index (BMI) decreased by a mean of 0.93, compared to a mean increase in those on placebo (0.85). Insulin resistance improved in the women on metformin as well.
Editor’s Note: Metformin can also delay the onset of type II diabetes in those in the borderline diabetic range. The weight loss on metformin was not spectacular and other options include the combination of the antidepressant bupropion (Wellbutrin) and the opiate antagonist naltrexone (Revia, 50mg/day), monotherapy with topiramate (Topamax), the fixed combination of topiramate and phentermine (Qsymia), or monotherapy with zonisamide (Zonegran).
RTMS Improves Working Memory In Patients With Schizophrenia
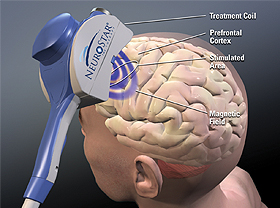 Repetitive transcranial magnetic stimulation (rTMS) may improve working memory in patients with schizophrenia, according to a small study published by Zafiris J. Daskalakis and colleagues in Biological Psychiatry in 2013. Patients with schizophrenia received either 20 Hz rTMS over the left and right prefrontal cortex or a sham treatment, and the rTMS improved working memory on a particular task, the n-back task, wherein patients are asked to recall whether a stimulus they’re currently viewing is the same as the previous one they viewed, or one they viewed several times back. Twenty sessions of rTMS over a period of 4 weeks brought memory back to the levels seen in normal controls.
Repetitive transcranial magnetic stimulation (rTMS) may improve working memory in patients with schizophrenia, according to a small study published by Zafiris J. Daskalakis and colleagues in Biological Psychiatry in 2013. Patients with schizophrenia received either 20 Hz rTMS over the left and right prefrontal cortex or a sham treatment, and the rTMS improved working memory on a particular task, the n-back task, wherein patients are asked to recall whether a stimulus they’re currently viewing is the same as the previous one they viewed, or one they viewed several times back. Twenty sessions of rTMS over a period of 4 weeks brought memory back to the levels seen in normal controls.
Editor’s Note: Since many patients with bipolar disorder also have deficits in prefrontal-based memory and performance even when euthymic, it will be important to see if rTMS would also be helpful in these patients. RTMS at 20 Hz increases neuronal activity as measured by PET scan of the prefrontal cortex and other regions of the brain, and this lasts for at least 48 hours after each treatment.
Since many patients with schizophrenia and bipolar disorder show deficits in prefrontal activity at baseline, the normalization of these alterations could relate to the memory improvement. This proposition could be tested relatively easily.