Obesity Associated with Inflammation and Brain Abnormalities
At the 2019 meeting of the International Society for Bipolar Disorders, researcher David J. Bond reviewed the data on the multiple adverse effects of obesity in patients with bipolar disorder. These include increased cardiovascular risk, poorer response to treatment, brain abnormalities, and decreased cognitive function, which is correlated with the degree of overweight.
Editor’s Note: These data emphasize the importance of starting a nutritious diet early in life and sustaining it through adulthood, avoiding the drugs most associated with weight gain such as clozapine and olanzapine, and facilitating weight loss with drugs. There are several treatments that can aid in weight loss. One is the diabetes treatment metformin, starting at a high dose of 500mg twice daily, and increasing to 1000mg twice daily if tolerated. The anticonvulsants topiramate or zonisamide also promote weight loss. The most effective option is a combination of the antidepressant bupropion sustained release (at a dose of 150–300mg) plus the anti–substance abuse drug naltrexone (50mg). This combination was associated with a loss of 10% of body weight over 12 weeks in women with diabetes.
Rich Western Diet Reprograms Immune Cells in Mice
A 2018 article by Anette Christ and colleagues in the journal Cell describes the process by which a Western diet can trigger changes to the immune system in mice. The mice fed a calorically rich Western diet started to show systemic inflammation. Blood measures of inflammation returned to normal after the mice resumed their regular diet, but their immune responses remained heightened, as if the immune system had been trained to overreact.
The vast majority of deaths in Western cultures are caused by noncommunicable diseases such as type 2 diabetes and cardiovascular disease, which have been linked to lifestyle factors such as diet and exercise. The immune system has two wings: one that responds to specific pathogens, and one that mounts general protection against infection and is triggered by immune signaling receptors. However, according to Christ and colleagues, in addition to reacting when microbes are present, this second wing may also respond to “sterile” danger signs, such as consumption of a Western diet. The immune system may become trained to react this way chronically, something that the researchers believe may trigger inflammation in noncommunicable diseases.
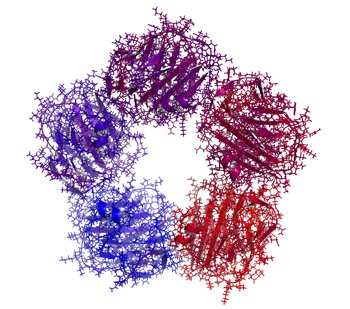
The Western diet triggered epigenetic changes to the mice’s immune system. Epigenetic changes are ones that affect the structure of DNA, for example how tightly it is packaged. In the case of the Western diet, these changes resulted in a heightened immune system that launched strong inflammatory responses in reaction to even small stimuli. Myeloid cells from bone marrow were reprogrammed to proliferate and provide a stronger immune response.
The researchers also took human monocyte cells trained with LDL (“bad”) cholesterol and stimulated them with lipopolysaccharide (an inflammatory compound made of fat and sugar). The cells showed a heightened immune reaction similar to that seen in the mice.
Mice genetically engineered to lack the inflammasome NLRP3, which activates inflammatory responses, did not show the systemic inflammation or the enhanced myeloid activity when fed the Western diet, so Christ and colleagues believe NLRP3 may play an important role in mediating the immune response to the Western diet.
Inflammation Associated With Duration of Untreated Unipolar Depression
Researcher Sophia Attwells and colleagues reported at a 2018 scientific meeting that the longer the time that a patient went without treatment for depression, the more inflammation they exhibited on positron emission tomography (PET) scans. Attwells and colleagues used the PET scans to assess the total distribution volume of TSPO, which is a marker of brain microglial activation, a form of inflammation.
Strikingly, in participants who had untreated major depressive disorder for 10 years or longer, TSPO distribution volume was 29–33% greater in the prefrontal cortex, anterior cingulate cortex, and insula than in participants who were untreated for 9 years or less. TSPO distribution volume was 31–39% greater in these three important regions of gray matter in participants with long durations of untreated major depressive disorder than in healthy control participants.
Editor’s Note: In schizophrenia, the duration of untreated interval (DUI) is associated with a poor prognosis, but not with inflammation. Researcher Yvette Sheline has also reported that less time on antidepressants compared to more time treated with them was associated with greater hippocampal volume loss with aging in patients with major depression.
Given Attwells and colleagues’ remarkable finding about the adverse effects of the DUI in depression, including inflammation and brain volume loss, and other findings that associate more episodes with poorer functioning, cognition, and treatment responsiveness, physicians and patients should think hard about committing to long-term antidepressant treatment to prevent episodes, beginning early in the course of illness.
This editor (Robert M. Post) would propose that if a second depressive episode occurs after a first depression that responded well to treatment, this would be an appropriate time to start antidepressant prophylaxis. Most guidelines suggest that prophylaxis be started after a third episode, but these recommendations generally do not account for newer data on the pernicious effects of experiencing repeated depressive episodes. In addition to causing dysfunction and disability, going through four depressive episodes doubles the risk of dementia in old age, and this risk increases further with each successive episode, according to researcher Lars Kessing.
Having too many depressions is bad for the brain. In Kessing’s studies, two episodes of unipolar or bipolar depression did not increase the risk of dementia compared to the general population, while four depressions did. One could compare the effects of repeated depressions on the brain to the effects of heart attacks on the heart muscle. A heart might still function well after one or even two heart attacks, but the chances of significant loss of function and the risk of congestive heart failure increase as a function of the number of heart attacks. After even one heart attack, most patients change their lifestyle and/or go on prophylactic medications to reduce risk factors such as elevated blood pressure, cholesterol, triglycerides, weight, blood sugar, and smoking. The benefits of reducing heart attacks are a no brainer. Trying to prevent recurrent depression with pharmacotherapy and adjunctive psychotherapy after a second depressive episode should be a no brainer too.
In addition, if antidepressants are not effective enough in preventing depressions, lithium is an option, even in unipolar depression, for preventing both episodes and suicide. The evidence of efficacy in both instances is very strong according to an article by Mohammed T. Abou-Saleh in the International Journal of Bipolar Disorders in 2017. The renowned psychiatrist Jules Angst’s recommendation as to when to start lithium treatment was that if a patient had had one episode or more in the previous five years in addition to the present episode, then they were likely to have two further episodes in the following five years, and lithium prophylaxis would be recommended.
Baseline Levels of CRP Could Help Predict Clinical Response to Different Treatments
C-reactive protein, or CRP, is a marker or inflammation that has been linked to depression and other illnesses. People with high levels of CRP respond differently to medications than people with lower CRP, so assessing CRP levels may help determine which medications are best to treat a given patient.
High baseline levels of CRP (3–5pg/ml) predict a poor response to selective serotonin reuptake inhibitor antidepressants (SSRIs) and to psychotherapy, and are associated with increased risk of recurrent depression, heart attack, and stroke.
However, high baseline CRP predicts a better response to the antidepressants nortriptyline and bupropion. High CRP is also associated with better antidepressant response to infliximab (a monoclonal antibody that inhibits the inflammatory cytokine TNF alpha), while low levels of CRP predict worsening depression upon taking infliximab.
High baseline CRP also predicts good antidepressant response to intravenous ketamine (which works rapidly to improve treatment-resistant depression), minocycline (an anti-inflammatory antibiotic that decreases microglial activation), L-methylfolate (a supplement that can treat folate deficiency), N-acetylcysteine (an antioxidant that can improve depression, pathological habits, and addictions), and omega-3 fatty acids (except in people with low levels of DHA).
High baseline CRP also predicts a good response to the antipsychotic drug lurasidone (marketed under the trade name Latuda) in bipolar depression. In people with high baseline CRP, lurasidone’s positive results have a huge effect size of 0.85, while in people with low CRP (<3pg/ml) the improvement on lurasidone has a smaller effect size (0.35).
In personal communications with this editor (Robert M. Post) in 2018, experts in the field (Charles L. Raison and Vladimir Maletic) agreed that assessing baseline CRP levels in a given patient could help determine optimal strategies to treat their depression and predict the patient’s responsiveness to different treatment approaches.
At a 2018 scientific meeting, researchers Cynthia Shannon, Thomas Weickert, and colleagues reported that high baseline levels of CRP were associated with symptom improvement in patients with schizophrenia when they were treated with the drug canakinumab (marketed under the trade name Ilaris). Canakinumab is a human monoclonal antibody that targets the inflammatory cytokine interleukin-1 beta (Il-1b). Il-1b is elevated in a subgroup of patients with depression, bipolar disorder, or schizophrenia, and CRP levels are an indication of the associated inflammation.
Il-6 Inhibitor Sirukumab May Improve Anhedonia, But Not General Depression
 At a 2018 scientific meeting, researcher Giacomo Salvadore and colleagues reported that the drug sirukumab, a monoclonal antibody that targets the inflammatory marker Il-6 and that was originally developed to treat rheumatoid arthritis, did not have a statistically significant effect on overall depression compared to placebo. However, by the twelfth week of treatment, sirukumab did have a significant effect on anhedonia (loss of interest or pleasure in activities that one previously enjoyed).
At a 2018 scientific meeting, researcher Giacomo Salvadore and colleagues reported that the drug sirukumab, a monoclonal antibody that targets the inflammatory marker Il-6 and that was originally developed to treat rheumatoid arthritis, did not have a statistically significant effect on overall depression compared to placebo. However, by the twelfth week of treatment, sirukumab did have a significant effect on anhedonia (loss of interest or pleasure in activities that one previously enjoyed).
The degree of improvement in anhedonia was significantly correlated with patients’ baseline levels of the inflammatory marker CRP. Since the inflammatory marker that sirukumab targets, Il-6, is one of those most often elevated in depression, it appears that more study of sirukumab would be warranted.
Inflammation Linked to Poor Sleep Quality and Worse Executive Functioning
At a recent scientific meeting, researcher Ellen E. Lee and colleagues reported that compared to healthy volunteers, people with bipolar disorder or schizophrenia had elevated levels of inflammatory markers, which were associated with poor sleep.
According to self-reports, people in the schizophrenia and bipolar disorder group had worse sleep quality than the control group. Those with schizophrenia or bipolar disorder also had significantly higher levels of the inflammatory markers CRP, IL-6, and TNF alpha compared to the healthy volunteers. Among people with bipolar disorder, executive functioning and sleep quality had a strong inverse association to levels of IL-6, such that lower sleep quality and worse executive functioning were associated with higher levels of IL-6. These findings suggest that sleep disturbance and inflammation may have negative consequences for cognitive functioning.
High Baseline Levels Of C-Reactive Protein Predict Better Response To Lurasidone in Bipolar Depression
In a study presented at the 2017 meeting of the International Society for Affective Disorders, Charlies L. Raison and colleagues examined whether baseline levels of the inflammatory marker C-reactive protein (CRP) affected antidepressant response to the antipsychotic drug lurasidone in bipolar depression. The participants were divided into three double-blind groups: one received 20–60mg/day of lurasidone, another received 80–120 mg/day of lurasidone, and the third received placebo over a period of six weeks. The effect was dramatic—in people with CRP levels above 5 mg/L at the beginning of the study, lurasidone (at either dosage level) had a very large effect size (d=0.85), while in people with baseline CRP levels below 5 mg/L the effect size was smaller (d=0.35).
Interestingly, 118 of the participants (24.5%) had CRP levels above 5mg/L at baseline, indicating a substantial amount of inflammation was present in a quarter of the bipolar depressed patients. Higher levels of CRP at baseline were correlated with better improvement on specific items on the Montgomery–Åsberg Depression Rating Scale (MADRS): “lassitude” (or lack of energy), “apparent sadness,” “reported sadness,” and “pessimistic thoughts.” Raison and colleagues concluded: “These findings suggest that the efficacy of lurasidone in patients with bipolar depression may in part be linked to the inflammatory status of patients prior to treatment. If confirmed in prospective investigations, [the results of a wide-range CRP assay] may prove useful as a predictive biomarker that could help optimize the use of lurasidone for the treatment of patients with bipolar depression.”
Editor’s Note: In many instances, high levels of CRP predict a poor response to treatment (such as to selective serotonin reuptake inhibitor antidepressants (SSRIs) in unipolar depression), so these findings are of considerable interest. They also suggest the untested possibility that lurasidone has anti-inflammatory effects, as those with high levels of inflammation at baseline often respond better to drugs with direct anti-inflammatory effects such as celecoxib (Celebrex) or the antioxidant N-acetylcysteine (NAC).
Inflammation is Associated with Antidepressant Treatment Resistance
Researcher Ebrahim Haroon and colleagues report in a 2018 issue of Psychoneuroendocrinology that people whose depression failed to respond to at least three different antidepressants in their current episode of depression had higher levels of inflammation than those who had fewer than three failed antidepressant trials.
The researchers found that patients who had not responded to antidepressants had higher levels of the inflammatory markers TNF-alpha, TNF-alpha receptor 2, and Il-6. The inflammatory marker CRP was also significantly elevated in these patients when statistical analyses that excluded body mass index (BMI) were used.
Haroon and colleagues reported that a third of all patients with major depressive disorder fail to respond to currently available antidepressant treatments, and that inflammation may be to blame because it interferes with the neurotransmitter systems that antidepressants target.
Editor’s Note: These data indirectly support the use of anti-inflammatory drugs to augment the effects of antidepressants in patients with treatment resistant depression. A caution that may be very important is to assess evidence of inflammation at baseline, as some data suggest that people with low CRP may, for example, do more poorly with a blocker of TNF-alpha, while people with high CRP at baseline (over 3 pg/ml) show good improvement.
Inflammatory Marker IL-6 is Elevated in People with Depression and Those with a History of Childhood Trauma
In a 2018 article in the journal Psychiatry Research, researcher Ana Munjiza and colleagues reported that the inflammatory marker IL-6 was higher in 64 depressed people than in 53 non-depressed people, and that levels of IL-6 among people in the depressed group were significantly correlated with scores on a questionnaire in which participants reported traumas experienced in childhood. They reported more physical abuse, physical neglect, and emotional abuse.
Munjiza and colleagues indicate that trauma in childhood is a risk factor for depression in adulthood, as other researchers have suggested, and that inflammation could mediate the relationship between childhood adversity and depression.
Editor’s Note: IL-6 has been associated with antidepressant treatment resistance. IL-6 is secreted from white cells in the blood and from monocytes from the bone marrow in response to stress. It enters the brain and starts an inflammatory cascade that induces depressive behaviors. Animal studies have shown that if IL-6 secretion is blocked, depressive-like behaviors do not occur.
Another indicator of inflammation is CRP, and elevations in CRP have been associated with poor response to selective serotonin reuptake inhibitor (SSRI) antidepressants, and better response to the noradrenergic tricyclic antidepressant nortriptyline and the dopamine active antidepressant bupropion.
Treatments for depressed people with histories of childhood trauma may include psychotherapy, somatic therapies such as repeated transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS), and medication. More research is needed to determine the optimal treatment regimens for this subgroup of depression sufferers, including whether anti-inflammatory drugs could play a helpful role in preventing or treating depression. People with elevated inflammatory markers (such as IL-6, CRP, IL-1, or TNF-alpha) are likely to be better candidates for adjunctive anti-inflammatory treatments than those with normal or low baseline levels of inflammation.
Inflammation and Depression: Treatment Implications
 Vladimir Maletic of the University of South Carolina School of Medicine Greenville gave a plenary talk at the 2018 meeting of the North Carolina Psychiatric Association that described a variety of ways that inflammation can drive depression.
Vladimir Maletic of the University of South Carolina School of Medicine Greenville gave a plenary talk at the 2018 meeting of the North Carolina Psychiatric Association that described a variety of ways that inflammation can drive depression.
Maletic explained that stress can increase neurotransmitters that activate brain macrophages, increase NFkB (a protein that controls DNA transcription and cell survival), and increase brain inflammation, evidenced by elevated levels of the inflammatory markers IL-1b, IL-6, TNF-alpha, and C-reactive protein (CRP). These signs of inflammation are associated with changes in brain function and connectivity that are consistent with depression, fatigue, and cognitive slowing.
Inflammation measured outside of the brain and spinal cord is associated with increased activity of the insula (a key brain sensor and modulator of emotions), disconnection between the prefrontal cortex and the reward circuits in the nucleus accumbens, and decreased function and structural changes to the hippocampus (critical for memory).
Maletic also explained that inflammation changes the way the amino acid tryptophan is metabolized. Normally tryptophan is converted into kyneurenic acid, which prevents excitotoxicity and has anticonvulsant effects. Stress can lead to tryptophan being metabolized instead into quinolinic acid, which is neurotoxic and has been linked to certain psychiatric disorders and neurodegenerative processes. This in turn impairs synaptic functioning, including increasing glutamate and decreasing brain-derived neurotrophic factor (BDNF), impairing a type of glia called oligodendroglia (which produce myelin), and the formation of new neural connections.
These findings have several important implications for treatment. Increases in inflammation have been linked to the atypical type of depression characterized by increased appetite, weight gain, and increased sleep rather than the more classic presentation of depression that includes loss of appetite, weight loss and insomnia. Thus, weight gain, waist circumference, and body mass index (BMI) are correlated with inflammation and can signal a poor response to medications (including the rapid-acting antidepressant ketamine and some other antidepressants). If someone with unipolar depression has high levels of CRP, they tend to have a poorer response to selective serotonin reuptake inhibitor (SSRI) antidepressants, and may respond better to the noradrenergic tricyclic antidepressant nortryptyline, the serotonin and norepinephrine reuptake inhibitors (SNRIs), and the dopamine active antidepressant bupropion.
There is some good news. Read more