Lumateperone Normalizes Pathological Levels of Acute Inflammation and Stimulates Important Pathways Involved in Mood Regulation
Highlights from Posters Presented at the Society of Biological Psychiatry Meeting, April 27-29, 2023 in San Diego
Sophie Dutheil of Intra-Cellular Therapies, Inc. reported that “In male and female C57BL/6 mice subjected to an acute stress or immune challenge, lumateperone reduced elevated levels of key proinflammatory cytokines. A number of key genes and pathways associated with the maintenance of tissue integrity and blood-brain barrier function were also altered by a single dose of lumateperone. Furthermore, we found that lumateperone administration conferred anxiolytic- and antianhedonic-like properties while enhancing the mTORC1 signaling pathway in the PFC.”
Chronic Fatigue, Depression and Anxiety Symptoms in Long COVID Are Strongly Predicted by Neuroimmune and Neuro- Oxidative Pathways Which Are Caused by the Inflammation during Acute Infection
HK Al-Hakeim et al in Michael Maes’ lab report in J. Clinical Medicine (2023) on very important findings about immune and oxidative changes in long COVID with “physio- somatic (chronic fatigue syndrome and somatic symptoms) and affective (depression and anxiety) symptoms. The severity of the long COVID physio-affective phenome is largely predicted by increased peak body temperature (BT) and lowered oxygen saturation (SpO2) during the acute infectious phase….. We recruited 86 patients with long COVID (3–4 months after the acute phase) and 39 healthy controls and assessed serum C-reactive protein (CRP), caspase 1, interleukin (IL) 1?, IL-18, IL-10, myeloperoxidase (MPO), advanced oxidation protein products (AOPPs), total antioxidant capacity (TAC), and calcium (Ca), as well as peak BT and SpO2 during the acute phase. Results: Cluster analysis revealed that a significant part (34.9%) of long COVID patients (n = 30) show a highly elevated NT (neurotoxicity) index as computed based on IL-1?, IL-18, caspase 1, CRP, MPO, and AOPPs. Partial least squares analysis showed that 61.6% of the variance in the physio-affective phenome of long COVID could be explained by the NT index, lowered Ca, and peak BT/SpO2 in the acute phase and prior vaccinations with AstraZeneca or Pfizer. The most important predictors of the physio-affective phenome are Ca, CRP, IL-1?, AOPPs, and MPO. Conclusion: The infection–immune–inflammatory core of acute COVID-19 strongly predicts the development of physio-affective symptoms 3–4 months later, and these effects are partly mediated by neuro-immune and neuro-oxidative pathways.”
Editors Note: These finding are important as they may lead to new treatment interventions. BNN readers are reminded of a previous BNN article by investigators from Yale (written by by Isabella Backman on Dec. 13, 2022) that in a new case study, they found that guanfacine plus N-acetylcysteine (which is an anti-inflammatory, anti-oxidant, and glutathione precursor) “mitigated and sometimes eliminated the cognitive impairment known as “brain fog” that often accompanies long COVID.
Inflammation Predicts Lower Frontal and Temporal White Matter Volumes in Early-Stage Bipolar Disorder
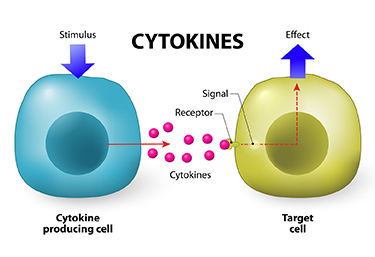 At the 2019 meeting of the International Society for Bipolar Disorders, researcher David Bond found that seven inflammatory cytokines predicted lower white matter volumes in the left frontal and bilateral temporal lobes, as well as in the cingulate and inferior frontal gyri. Cytokines are secreted by some immune cells and send signals that can produce an effect in other cells.
At the 2019 meeting of the International Society for Bipolar Disorders, researcher David Bond found that seven inflammatory cytokines predicted lower white matter volumes in the left frontal and bilateral temporal lobes, as well as in the cingulate and inferior frontal gyri. Cytokines are secreted by some immune cells and send signals that can produce an effect in other cells.
Bond noted that greater inflammation did not predict lower parietal or occipital white matter volumes, suggesting that inflammation had a greater effect on white matter volume in those parts of the brain most closely linked to mood disorders.
Inflammation Associated with Cognitive Deficits
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Katherine E. Burdick and colleagues at Brigham and Women’s Hospital and Harvard Medical School reported that in 240 patients with bipolar disorder who were not currently having a manic or depressive episode, markers of inflammation were associated with cognitive deficits.
Inflammation was associated with cognitive deficits in general, and there were also some relationships between specific inflammatory markers and types of cognitive processing. They found that the inflammatory markers TNF-alpha, TNFR1, and TNFR2 influenced cognitive flexibility. The inflammatory marker VEGF influenced reward processing, while IL-6/IL-6r influenced spatial processing. IL-1beta and IL-1RA influenced social cognition.
Burdick and colleagues found it was important to include both primary and secondary mediators of inflammation in their research “as the effects of the primary pro-inflammatory cytokines can be blocked by a number of decoy receptors and soluble antagonists.” Elevations in these can provide additional information about the function of the immune system.
Editor’s Note: Targeting inflammation with the anti-inflammatory treatments minocycline and celecoxib has been shown to improve depression. Now the role of anti-inflammatory drugs in improving cognition deserves further attention.
Links Between Mixed Depression, Insulin Resistance, Inflammation, and Cognitive Deficits
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Roger McIntyre discussed links between obesity, diabetes, and cardiovascular problems; increased inflammation; and decreased functioning of the neural networks involved in cognition.
He and his colleagues analyzed 121 studies that included empirical research and meta-analyses. McIntyre and colleagues found that patients with higher levels of inflammatory markers have more insulin resistance and cognitive dysfunction. A meta-analysis revealed that the inflammatory markers IL-6, TNF alpha, and CRP were significantly elevated in people with bipolar disorder compared to normal controls, while IL-1B was not.
People with depression who had a few manic traits (mixed depression) were particularly likely to have insulin resistance and elevated levels of pro-inflammatory markers.
People with mixed depression have increases in inflammation and increased incidence of cardiovascular disorder. People experiencing a first episode of mixed depression who are overweight show increased signs of brain aging.
In studies McIntyre and colleagues analyzed, diabetes or pre-diabetes occurred in 50% of depressed patients, and these patients had the greatest amount of cognitive dysfunction.
Treatment
McIntyre noted that taking the antipsychotic drug lurasidone for bipolar depression worked best in both adults and children who had elevated levels of CRP at baseline. The fast-acting antidepressant ketamine also works well in those who show baseline inflammation .
The anti-diabetes drug liraglutide (Victoza, Saxenda) improves mixed depression symptoms and cognition in obesity, diabetes, and mixed depression. Liraglutide belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists or incretin mimetics. They work by increasing insulin release from the pancreas and decreasing excessive glucagon release.
McIntyre now routinely uses liraglutide for cognitive deficits in patients with obesity or diabetes, including patients with mixed depression. It is injected under the skin at 0.6 mg daily, then the dosage is increased to 1.2 mg and then 1.8 mg. Victoza reduces major cardiovascular events in those with type 2 diabetes. The higher-dose Saxenda (3mg) can be used for weight control.
Another anti-diabetes drug, pioglitazine, has also been reported to be helpful in bipolar depression.
McIntyre found that the antibody infliximab, which can be used as an intravenous treatment for chronic inflammation and works by blocking the effects of TNF-alpha, did not improve depression, but did improve cognition.
McIntyre also supports the use of acetyl-L-carnitine, a potential adjunctive treatment that can reverse the insulin resistance that often occurs with obesity and thus could theoretically improve cognition.
McIntyre described preliminary literature suggesting the effectiveness of drugs such as statins, calcium channel blockers, and biguanides such as the diabetes treatment metformin in reducing inflammation.
Bariatric surgery to reduce the size of the stomach was another option discussed by McIntyre. He said the intervention is safe for patients with bipolar disorder and can help them recover cognitive function.
McIntyre noted that offspring of a mother with obesity have decreased response to sensory cues, reward preference, cognitive control, and motor control. Obesity and the inflammation that goes along with it apparently affect offspring via epigenetic mechanisms, meaning obesity may change the structure of inherited DNA (without changing its sequence).
Obesity Associated with Inflammation and Brain Abnormalities
At the 2019 meeting of the International Society for Bipolar Disorders, researcher David J. Bond reviewed the data on the multiple adverse effects of obesity in patients with bipolar disorder. These include increased cardiovascular risk, poorer response to treatment, brain abnormalities, and decreased cognitive function, which is correlated with the degree of overweight.
Editor’s Note: These data emphasize the importance of starting a nutritious diet early in life and sustaining it through adulthood, avoiding the drugs most associated with weight gain such as clozapine and olanzapine, and facilitating weight loss with drugs. There are several treatments that can aid in weight loss. One is the diabetes treatment metformin, starting at a high dose of 500mg twice daily, and increasing to 1000mg twice daily if tolerated. The anticonvulsants topiramate or zonisamide also promote weight loss. The most effective option is a combination of the antidepressant bupropion sustained release (at a dose of 150–300mg) plus the anti–substance abuse drug naltrexone (50mg). This combination was associated with a loss of 10% of body weight over 12 weeks in women with diabetes.
Inflammation Associated With Duration of Untreated Unipolar Depression
Researcher Sophia Attwells and colleagues reported at a 2018 scientific meeting that the longer the time that a patient went without treatment for depression, the more inflammation they exhibited on positron emission tomography (PET) scans. Attwells and colleagues used the PET scans to assess the total distribution volume of TSPO, which is a marker of brain microglial activation, a form of inflammation.
Strikingly, in participants who had untreated major depressive disorder for 10 years or longer, TSPO distribution volume was 29–33% greater in the prefrontal cortex, anterior cingulate cortex, and insula than in participants who were untreated for 9 years or less. TSPO distribution volume was 31–39% greater in these three important regions of gray matter in participants with long durations of untreated major depressive disorder than in healthy control participants.
Editor’s Note: In schizophrenia, the duration of untreated interval (DUI) is associated with a poor prognosis, but not with inflammation. Researcher Yvette Sheline has also reported that less time on antidepressants compared to more time treated with them was associated with greater hippocampal volume loss with aging in patients with major depression.
Given Attwells and colleagues’ remarkable finding about the adverse effects of the DUI in depression, including inflammation and brain volume loss, and other findings that associate more episodes with poorer functioning, cognition, and treatment responsiveness, physicians and patients should think hard about committing to long-term antidepressant treatment to prevent episodes, beginning early in the course of illness.
This editor (Robert M. Post) would propose that if a second depressive episode occurs after a first depression that responded well to treatment, this would be an appropriate time to start antidepressant prophylaxis. Most guidelines suggest that prophylaxis be started after a third episode, but these recommendations generally do not account for newer data on the pernicious effects of experiencing repeated depressive episodes. In addition to causing dysfunction and disability, going through four depressive episodes doubles the risk of dementia in old age, and this risk increases further with each successive episode, according to researcher Lars Kessing.
Having too many depressions is bad for the brain. In Kessing’s studies, two episodes of unipolar or bipolar depression did not increase the risk of dementia compared to the general population, while four depressions did. One could compare the effects of repeated depressions on the brain to the effects of heart attacks on the heart muscle. A heart might still function well after one or even two heart attacks, but the chances of significant loss of function and the risk of congestive heart failure increase as a function of the number of heart attacks. After even one heart attack, most patients change their lifestyle and/or go on prophylactic medications to reduce risk factors such as elevated blood pressure, cholesterol, triglycerides, weight, blood sugar, and smoking. The benefits of reducing heart attacks are a no brainer. Trying to prevent recurrent depression with pharmacotherapy and adjunctive psychotherapy after a second depressive episode should be a no brainer too.
In addition, if antidepressants are not effective enough in preventing depressions, lithium is an option, even in unipolar depression, for preventing both episodes and suicide. The evidence of efficacy in both instances is very strong according to an article by Mohammed T. Abou-Saleh in the International Journal of Bipolar Disorders in 2017. The renowned psychiatrist Jules Angst’s recommendation as to when to start lithium treatment was that if a patient had had one episode or more in the previous five years in addition to the present episode, then they were likely to have two further episodes in the following five years, and lithium prophylaxis would be recommended.
Inflammation Linked to Poor Sleep Quality and Worse Executive Functioning
At a recent scientific meeting, researcher Ellen E. Lee and colleagues reported that compared to healthy volunteers, people with bipolar disorder or schizophrenia had elevated levels of inflammatory markers, which were associated with poor sleep.
According to self-reports, people in the schizophrenia and bipolar disorder group had worse sleep quality than the control group. Those with schizophrenia or bipolar disorder also had significantly higher levels of the inflammatory markers CRP, IL-6, and TNF alpha compared to the healthy volunteers. Among people with bipolar disorder, executive functioning and sleep quality had a strong inverse association to levels of IL-6, such that lower sleep quality and worse executive functioning were associated with higher levels of IL-6. These findings suggest that sleep disturbance and inflammation may have negative consequences for cognitive functioning.
Inflammation is Associated with Antidepressant Treatment Resistance
Researcher Ebrahim Haroon and colleagues report in a 2018 issue of Psychoneuroendocrinology that people whose depression failed to respond to at least three different antidepressants in their current episode of depression had higher levels of inflammation than those who had fewer than three failed antidepressant trials.
The researchers found that patients who had not responded to antidepressants had higher levels of the inflammatory markers TNF-alpha, TNF-alpha receptor 2, and Il-6. The inflammatory marker CRP was also significantly elevated in these patients when statistical analyses that excluded body mass index (BMI) were used.
Haroon and colleagues reported that a third of all patients with major depressive disorder fail to respond to currently available antidepressant treatments, and that inflammation may be to blame because it interferes with the neurotransmitter systems that antidepressants target.
Editor’s Note: These data indirectly support the use of anti-inflammatory drugs to augment the effects of antidepressants in patients with treatment resistant depression. A caution that may be very important is to assess evidence of inflammation at baseline, as some data suggest that people with low CRP may, for example, do more poorly with a blocker of TNF-alpha, while people with high CRP at baseline (over 3 pg/ml) show good improvement.
Inflammation and Depression: Treatment Implications
 Vladimir Maletic of the University of South Carolina School of Medicine Greenville gave a plenary talk at the 2018 meeting of the North Carolina Psychiatric Association that described a variety of ways that inflammation can drive depression.
Vladimir Maletic of the University of South Carolina School of Medicine Greenville gave a plenary talk at the 2018 meeting of the North Carolina Psychiatric Association that described a variety of ways that inflammation can drive depression.
Maletic explained that stress can increase neurotransmitters that activate brain macrophages, increase NFkB (a protein that controls DNA transcription and cell survival), and increase brain inflammation, evidenced by elevated levels of the inflammatory markers IL-1b, IL-6, TNF-alpha, and C-reactive protein (CRP). These signs of inflammation are associated with changes in brain function and connectivity that are consistent with depression, fatigue, and cognitive slowing.
Inflammation measured outside of the brain and spinal cord is associated with increased activity of the insula (a key brain sensor and modulator of emotions), disconnection between the prefrontal cortex and the reward circuits in the nucleus accumbens, and decreased function and structural changes to the hippocampus (critical for memory).
Maletic also explained that inflammation changes the way the amino acid tryptophan is metabolized. Normally tryptophan is converted into kyneurenic acid, which prevents excitotoxicity and has anticonvulsant effects. Stress can lead to tryptophan being metabolized instead into quinolinic acid, which is neurotoxic and has been linked to certain psychiatric disorders and neurodegenerative processes. This in turn impairs synaptic functioning, including increasing glutamate and decreasing brain-derived neurotrophic factor (BDNF), impairing a type of glia called oligodendroglia (which produce myelin), and the formation of new neural connections.
These findings have several important implications for treatment. Increases in inflammation have been linked to the atypical type of depression characterized by increased appetite, weight gain, and increased sleep rather than the more classic presentation of depression that includes loss of appetite, weight loss and insomnia. Thus, weight gain, waist circumference, and body mass index (BMI) are correlated with inflammation and can signal a poor response to medications (including the rapid-acting antidepressant ketamine and some other antidepressants). If someone with unipolar depression has high levels of CRP, they tend to have a poorer response to selective serotonin reuptake inhibitor (SSRI) antidepressants, and may respond better to the noradrenergic tricyclic antidepressant nortryptyline, the serotonin and norepinephrine reuptake inhibitors (SNRIs), and the dopamine active antidepressant bupropion.
There is some good news. Read more







