The Unfolding Story of Poor Response to Antidepressants in Bipolar Depression
The role of the traditional antidepressants in the treatment of depression in bipolar illness remains controversial. Despite mounting evidence that they are not efficacious in the treatment of bipolar depression, they are still among the most widely used treatments for that condition. At the first biennial conference of the International Society for Bipolar Disorders held in Istanbul this past March, Mark A. Frye and Shigenobu Kanba chaired a symposium on antidepressant-induced mania and individualized treatment for bipolar depression.
This editor (Robert M. Post) discussed factors influencing antidepressants’ effects on patients with bipolar depression. In a recent meta-analysis, researchers Sidor and MacQueen reviewed data from studies encompassing 2373 patients with bipolar depression and found that antidepressants had no significant benefits over placebo on measures of response or remission. Pooled estimates for a thousand patients showed no increase in patients’ risk of switching into mania after treating with antidepressants. However, in a smaller sub-analysis, the risks of switching into mania following treatment with the older tricyclic antidepressants (43%) and venlafaxine (15%) was greater than the risk of switching after being treated with SSRIs (7%) or bupropion (5%).
There is a conundrum in the literature. While antidepressants don’t work very well in bipolar depression, there is a small subgroup of patients who, having responded well to antidepressants for two months, benefit more from continuing the antidepressant treatment than from discontinuing the drug. Continued treatment with adjunctive antidepressants (added to regular treatment with a mood stabilizer or an atypical antipsychotic) was associated with fewer relapses into depression over the next year when the antidepressants were continued compared to when they were discontinued. Lori Altshuler et al. have published two uncontrolled studies to this effect, Russell Joffe et al. have published one, and a more recent randomized study of this by Nassir Ghaemi replicated some of the results in patients who had non-rapid-cycling bipolar disorder. At the same time, the literature shows that there are number of risk factors for switching into hypomania during antidepressant treatment in bipolar depression.
Risk factors for switching into mania upon treatment with an antidepressant include: younger age, bipolar I compared to bipolar II, rapid cycling in the past year, mixed depression, use of older tricyclic antidepressants compared to newer second-generation antidepressants, use of noradrenergic active antidepressants compared to those that act on serotonin or dopamine, and a history of substance abuse. Read more
Psychiatric Medications Just as Effective as Medications for Other Illnesses
The popular media has sometimes scrutinized research on psychiatric medications, suggesting that they are not as effective as pharmaceutical companies would have us believe. Researchers in Germany recently performed a meta-analysis of research on psychiatric medications and found that the effect sizes for psychiatric drugs were comparable to effect sizes of other types of drugs. (Effect sizes communicate the size of the change that a drug brings about in patients.) The study was published in the British Journal of Psychiatry.
From the abstract:
Any comparison of different outcomes in different diseases can only serve the purpose of a qualitative perspective. The increment of improvement by drug over placebo must be viewed in the context of the disease’s seriousness, suffering induced, natural course, duration, outcomes, adverse events and societal values.
Antidepressants Work Better in Major Depressive Disorder than Previously Thought
As we’ve written before, the popular media has sometimes questioned the efficacy of antidepressants for unipolar depression. A reanalysis of data from previous controlled trials of fluoxetine and venlafaxine that was recently published in the Archives of General Psychiatry provides new evidence that these drugs are significantly more efficacious than placebo in youth, adult, and geriatric populations with major depressive disorder.
The researchers concluded,
To our knowledge, this is the first research synthesis in this area to use complete longitudinal person-level data from a large set of published and unpublished studies. The results do not support previous findings that antidepressants show little benefit except for severe depression. The antidepressants fluoxetine and venlafaxine are efficacious for major depressive disorder in all age groups, although more so in youths and adults compared with geriatric patients. Baseline severity was not significantly related to degree of treatment advantage over placebo.
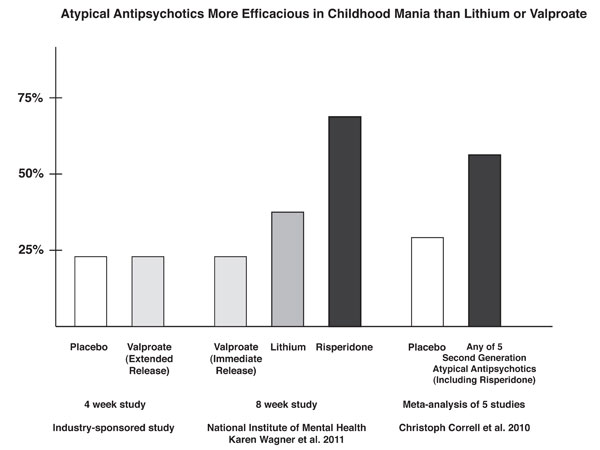
Risperidone Trumps Valproate and Placebo for Treatment of Young Children with Mania
 At another symposium at the annual meeting of the American Academy of Child and Adolescent Psychiatry, Bob Kowatch of Ohio State University discussed a controlled trial of valproate, risperidone, and placebo in children 3 to 7 years of age (average age 5.5) with a diagnosis of bipolar I disorder and a Young Mania Rating Scale score (YMRS) greater than 20 at baseline. All of the children were severely ill with an average Clinical Global Assessment of Severity (CGAS) score of 44. Seventy-six percent had comorbid attention deficit hyperactivity disorder (ADHD) and 15% had an anxiety disorder. Valproate doses started at 10mg/kg and were increased after 4 days to achieve blood levels of 80 to 100µg/ml. The average dose of valproate was 300mg/day and the average blood level was 88 µg/ml. Risperidone was started at 0.25mg and increased as needed. The average dose of risperidone was 0.5mg per day.
At another symposium at the annual meeting of the American Academy of Child and Adolescent Psychiatry, Bob Kowatch of Ohio State University discussed a controlled trial of valproate, risperidone, and placebo in children 3 to 7 years of age (average age 5.5) with a diagnosis of bipolar I disorder and a Young Mania Rating Scale score (YMRS) greater than 20 at baseline. All of the children were severely ill with an average Clinical Global Assessment of Severity (CGAS) score of 44. Seventy-six percent had comorbid attention deficit hyperactivity disorder (ADHD) and 15% had an anxiety disorder. Valproate doses started at 10mg/kg and were increased after 4 days to achieve blood levels of 80 to 100µg/ml. The average dose of valproate was 300mg/day and the average blood level was 88 µg/ml. Risperidone was started at 0.25mg and increased as needed. The average dose of risperidone was 0.5mg per day.
On the main outcome measure of decrease in the YMRS score risperidone was substantially more effective than placebo, while valproate showed only marginal nonsignificant effects. However on the Clinical Global Impressions (CGI) scale for improvement in illness, risperidone showed 87% response, valproate 75% response, and placebo no response. In terms of 50% reduction in the YMRS score, this endpoint was achieved in 88% on risperidone, 50% valproate, and 15% on placebo.
Weight gain was mild on valproate and substantially more on risperidone. Risperidone was also associated with increases in insulin and prolactin.
The effect size (the size of the change the drug brought about in this study, which is calculated by dividing the mean difference between the experimental group and the control group by the standard deviation) for risperidone was extraordinarily large (3.58); very large for valproate (1.66), and moderate for placebo (0.56). The odds of getting well were 5 times greater than placebo for risperidone and 1.9 times greater than placebo for valproate.
Editors note: These data in very young children (aged 3 to 7) resemble other controlled data in the literature about the treatment of older children and adolescents, indicating a superiority of atypical antipsychotics over placebo and a greater magnitude of effect achieved with atypicals than with valproate. Based on these new data and the Federal Drug Administration (FDA) approval of several atypical antipsychotics for children with bipolar illness from ages 10 to 17, Dr. Kowatch recommended a new treatment algorithm for childhood onset bipolar disorder. Read more
Obesity and Bipolar Disorder: News from the American Academy of Child and Adolescent Psychiatry
 At the annual meeting of the American Academy of Child and Adolescent Psychiatry in Toronto in October 2011, a symposium on the impact of obesity on the course of childhood onset bipolar illness was held.
At the annual meeting of the American Academy of Child and Adolescent Psychiatry in Toronto in October 2011, a symposium on the impact of obesity on the course of childhood onset bipolar illness was held.
Typical Treatment of Bipolar Disorder in Youth
David Axelson described the typical outcome of bipolar illness and the medications used during naturalistic treatment. The data came from the large collaborative Course and Outcome of Bipolar Illness among Youth (COBY) study, in which he and his colleagues followed 255 patients with bipolar I disorder (BP I), 30 patients with bipolar II (BP II), and 153 patients with bipolar not otherwise specified (BP NOS) for a mean of 5 years. He discussed only BP I children at the symposium.
The study initially followed 270 BP I children for a mean of 582 weeks. They ranged in age from 7 to 17 years (average 14.4 years). Ninety-three percent of the children were treated with one or more antimanic (AM) agents. These included atypical antipsychotics (AA) in 77%, valproate or carbamazepine in 44%, and lithium in 47%. Antidepressants (ADs) were used in 46% of the children, stimulants in 43%, and benzodiazepines in 21%. Sixty percent had been on two classes of antimanic medications concurrently at some point.
A univariate analysis showed that older children received smaller amounts of antipsychotics and more anticonvulsants and lithium. Variables associated with better response, that is, a rating of either much or very much improved on the Clinical Global Impressions scale for bipolar disorder (CGI-BP), included older age and treatment with atypical antipsychotics. Those who had comorbid attention deficit hyperactivity disorder (ADHD) or psychosis at baseline did more poorly. Mean symptom scores were better when the children received any anti-manic treatment including an atypical or lithium, but worse when they received valproate or carbamazepine.
These data are similar to those from other prospective treatment outcome studies in childhood-onset bipolar I illness. Taken together they all suggest that the illness is difficult to treat and stabilize even when multiple medicines are used in combination.
Obesity and Mood Disorders in Youth
Another speaker, Ben Goldstein, indicated that in the scientific literature, obesity has been associated with a higher number of depressive episodes and longer length of depression, more recurrences of depression, more anxiety disorders, increased numbers of hospitalization, more suicide attempts, and worse functional outcomes. In the same group of patients discussed by Axelson above, 42% were overweight or obese, compared to a 34% incidence in the general population of children in this age range.
Factors associated with overweight included substance abuse, a history of physical abuse, prior hospitalization, and being on 2 or more medications. Those who were overweight or obese spent more time ill in a manic or depressive episode. Read more
News From The “TEAM” Study: Risperidone Superior To Valproate And Lithium In Childhood Mania
A symposium at the Annual Meeting of the American Association of Child and Adolescent Psychiatry discussed the Treatment of Early Age Mania (TEAM) study, which comprised 5 different sites in Pittsburgh, Washington DC, Baltimore, St. Louis, and Cleveland. This randomized partially blinded study compared risperidone, valproate, and lithium for the treatment of children with bipolar I mania.
Participants were all severely ill with a Clinical Global Assessment of Severity score (C-GAS) of less than 60 (the mean was 39, indicating that the children were substantially impaired). More than three quarters had psychosis (i.e. hallucinations or delusions) and 99% had dramatic mood shifts within a day (ultradian cycling). All the children had the cardinal symptom of elevated mood.
Among the 290 participants, there was a high incidence of Axis I comorbidities, with 98% of patients having a disruptive behavioral disorder, 77.3% an anxiety disorder, 31% some form of sleep disturbance, and 17% an elimination disorder, of which 15% had enuresis (bedwetting). Nightmares were present in 25.9% of the sample, sleepwalking in 7.2%, and night terrors in 4.8%.
For the purposes of the study, response was considered to have been achieved when a child received a rating of 1 (not ill) or 2 (minimally ill) on the Clinical Global Impressions scale modified for bipolar illness (CGI-BP).
The children (age 6 to 15 with a mean age of 11) were randomized to treatment for 8 weeks with lithium, valproate, or risperidone. Lithium treatment reached blood levels of 1.1 to 1.3mEq/L, valproate reached levels of 111 – 225µg/ML, and risperidone doses were up to 3mg per day. Children who were taking psychomotor stimulants for treatment of ADHD remained on the stimulants after randomization to one of the three drugs. While the treating physicians and clinicians were not blind, blind ratings were performed at week 8.
With a response rate of 68.5%, risperidone was superior to lithium (35.6%) and valproate (24%) based on CGI-BP scores. The mean dose of risperidone was 2.6mg +/- 1.2 per day. The mean blood level at week 8 for lithium was 1.1mEq/L and for valproate was 114µg/ML.
The number of children who improved sufficiently for their C-GAS scores to rise above 60 was also greater for risperidone at 48.3% compared to lithium at 26.7% and valproate at 17.0%. Read more
Valproate Can Cause Increases in Blood Ammonia
 Researcher C. Lewis reported in two posters presented at the Ninth International Conference on Bipolar Disorder (ICBD) in 2011 that in a study of patients treated with valproate, some increases in ammonia levels occurred. This condition, hyperamonaemia, was identified in 31 patients among those treated between 2005 and 2009 at the Cleveland Clinic in Cleveland, Ohio. High levels of ammonia are associated with a flapping tremor and, in some cases, encephalopathy with confusion, psychiatric symptoms, and motor incoordination.
Researcher C. Lewis reported in two posters presented at the Ninth International Conference on Bipolar Disorder (ICBD) in 2011 that in a study of patients treated with valproate, some increases in ammonia levels occurred. This condition, hyperamonaemia, was identified in 31 patients among those treated between 2005 and 2009 at the Cleveland Clinic in Cleveland, Ohio. High levels of ammonia are associated with a flapping tremor and, in some cases, encephalopathy with confusion, psychiatric symptoms, and motor incoordination.
The recommended management for hyperamonaemia is discontinuation of valproate and use of lactulose, a synthetic sugar that can lower ammonia levels. These approaches were not always used. Another option for patients who require valproate treatment is to supplement the drug with carnitine, which is available as a nutritional supplement. Lewis reported success in three such cases.
Editor’s Note: Patients on valproate presenting with a gross flapping tremor of the hands, confusion, or motor imbalance should be tested for hyperamonaemia and treated accordingly.
Clinical Evidence May Explain the Mechanisms of Ketamine’s Rapid Acting Antidepressant Effects
At the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011, C.G. Abdallah from SUNY Downstate Medical Center reported on a study of intravenous ketamine for treatment-resistant depression. Twelve medication-free participants aged 18-65 received 0.5mg/kg ketamine over 40 minutes. There was a rapid-onset antidepressant effect, as there has been in other studies of unipolar and bipolar depressed patients. In a subgroup of 4 patients examined with magnetic resonance spectroscopy (MRS), there were rapid increases in brain GABA followed shortly thereafter by increases in brain glutamate concentrations.
Editor’s note: The rapid increases in GABA and glutamate that occur after the administration of intravenous ketamine may help account for its therapeutic effects. Other studies have shown that brain GABA is low in depressed patients, so the rapid increase in GABA with ketamine administration could partly explain the antidepressant effects of the drug. The role of the glutamate increases remains to be further explored.
Neli and associates from Yale had reported that in animals, ketamine was able to rapidly alter synapse structure and function. In an animal model of depression, rodents are exposed to chronic and unpredictable stress and develop depressive-like behavior. The mature, mushroom-shaped spines on their dendrites (the parts of neurons that receive synapses and determine the neuron’s excitability) also lose their shape, becoming straighter and spikier like immature spines. Intravenous ketamine not only improves the animals’ behavior, but also increases the number of mushroom-shaped spines within a matter of hours, rapidly improving synaptic function. This effect of ketamine was dependent on a novel intracellular pathway involving the enzyme mTOR, which if blocked prevented the re-emergence of the mature spines.
In the brains of depressed humans studied at autopsy there is reduced neural volume in the frontal cortex, which could possibly be related to dendritic atrophy and associated changes in spine shape as it appears to be in rodents. The animal data suggest the remarkable possibility that intravenous ketamine’s rapid onset of antidepressant effects could also be associated with rapid improvement in the microanatomy of the brain.
The data on ketamine’s effects in animals and the new clinical data showing that GABA and glutamate increases occurred rapidly in depressed patients administered ketamine provide further insight into the potential mechanisms of ketamine’s effect.
Aripiprazole Makes Lamotrigine More Effective
 In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
Editor’s note: These data add to a growing literature that shows that an atypical antipsychotic added to a mood stabilizer is associated with better prophylactic effects than use of the mood stabilizer alone. Previously, most of the studies of this type of combination used lithium or valproate as the mood stabilizer and, to our knowledge, this is the first to demonstrate that long-term prevention with lamotrigine is enhanced by the addition of an atypical antipsychotic.
Many of the atypical antipsychotics are FDA-approved as adjunctive treatments to mood stabilizers in the long-term treatment of bipolar disorder. The controlled clinical trial data that led to this FDA approval support the practice of many clinicians who prescribe combination treatment rather than monotherapy in order to achieve a more rapid onset of anti-manic stabilization and longer-term maintenance effects. The use of aripiprazole and quetiapine as adjuncts to lithium and valproate is particularly common in bipolar disorder since the same atypical antipsychotics are FDA-approved as adjunctive treatments in unipolar depression, and clinicians are familiar with prescribing them to improve ineffective acute antidepressant treatment.
The Risk-Benefit Ratio Encourages the Use of Antidepressants in Unipolar Depression
Wednesday we reviewed new data that shows that despite the FDA warning that antidepressants can increase suicidal ideation among young people in the first few months they are taken, antidepressants actually reduce acute suicidal ideation and decrease suicidal acts. As we described last year in our article on five myths about antidepressants, antidepressant treatment in recurrent unipolar depression is important to patients’ long-term wellbeing, cognitive functioning, and even life expectancy.
Untreated depression, and particularly untreated recurrent depression, carries high risks not only for lethality by suicide, but also for increases in medical mortality, particularly from cardiovascular disease. In addition to these medical risks, data from many studies suggest that a higher number of prior depressions is associated with increased cognitive dysfunction, and recent large data sets from a case registry in Denmark indicate that patients with four or more prior unipolar or bipolar depressive episodes have double the risk of receiving a diagnosis of dementia in old age. Thus, depressions are dangerous for a patient’s psychological, medical, and cognitive health.
Antidepressants Are Highly Effective in Depression Prevention
In 1992 researcher John Davis completed a meta-analysis of all antidepressant data available at the time in unipolar depression studies and not only found that antidepressant continuation was more effective than placebo in reducing the likelihood of later depressions, but also calculated that the statistical likelihood that this finding was due to chance was minuscule, i.e., p<10-34. John Geddes and colleagues in a meta-analysis in 2003 indicated that there was an approximate 70% reduction in the risk of depressive recurrences with antidepressant continuation compared with discontinuation.
Treatment of a first or second episode of unipolar depression is recommended for six to nine months following achievement of remission. After a third episode, all treatment guidelines of which this editor is aware recommend long-term preventive treatment with antidepressants, particularly if episodes have been severe or close together temporally. This long-term antidepressant continuation for prophylaxis is much like long-term treatment of high blood pressure or high cholesterol recommended for those with or at high risk for cardiovascular disease.
There is some evidence that cognitive behavior therapy reduces the risk for depressive recurrence in those discontinuing antidepressant treatment, but it appears maximally beneficial to engage both psychotherapeutic and pharmacological treatment to prevent future episodes. Read more