Antidepressants Prevent Suicide in Patients with Unipolar Depression
Researcher A. Kahn reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in Boca Raton in 2011 that severely depressed and suicidal patients taking citalopram (Celexa) or a combination of citalopram and low dose lithium experienced improvements in depression and suicidal thoughts. This study was unusual because most clinical trials exclude actively suicidal patients. In the group of subjects receiving citalopram plus lithium (300 mg/day and achieving 0.5 mEq/l or higher), there were several indications of better anti-suicide effects than in those on citalopram alone. The authors concluded that with appropriate doses, antidepressants plus lithium may prospectively reduce suicidal thoughts, and that it is possible to conduct clinical trials in severely depressed and suicidal patients if adequate safety measures are included.
Surprisingly, improvement in suicidal ideation preceded improvement in depressed mood per se.
Editor’s note: The study reported here suggests that in those with high suicidal ideation scores at baseline, antidepressants with or without lithium may quickly bring about anti-suicidal effects on thoughts, desires, and behaviors. Whether these effects occur reliably in studies in other groups of patients and in younger individuals remains to be established.
These data are an interesting contrast to data on antidepressant use in those with low levels of suicidality at baseline. A number of studies have suggested that in children and adolescents who were exposed to an antidepressant, a small percentage experienced increases in suicidal ideation in the first two months of treatment compared to patients taking placebo. This led to a Federal Drug Administration (FDA) warning (directed at all patients taking antidepressants) that increases in suicidal ideation and action may occur upon starting antidepressants.
It is important to note that the warning does not refer to completed suicides; the data set that led to the FDA warning included no completed suicides. More than 70% of those with suicidal ideation do not make an attempt, and the vast majority of attempts do not result in a completed suicide.
Most of the studies that found the slight increase in suicidal ideation in some patients after beginning antidepressant treatment actively excluded acutely suicidal patients. Since the study of citalopram and lithium above used a population of severely depressed and suicidal patients and found that antidepressants improved suicidality, it appears important to consider a patient’s baseline state when considering psychiatric interventions. In another example, there is an interesting difference between the way depressed patients and non-depressed normal volunteers respond to one night’s sleep deprivation: depressed patients often show dramatic improvement, while normal volunteers tend to feel worse.
More Evidence that Antidepressants Prevent Suicide in Unipolar Depression
A new study by DeLeon published in the Journal of Clinical Psychiatry in 2011 found that during periods of life when unipolar patients were taking antidepressants (compared to times when they were not taking them) the patients experienced 20% fewer suicidal acts or completed suicides. Read more
Lithium More Effective than Valproate for Bipolar Disorder
 According to two studies in 2011, lithium is more effective in treating episodes of bipolar disorder than valproate, while the drugs may be equally effective in reducing suicidality among bipolar patients.
According to two studies in 2011, lithium is more effective in treating episodes of bipolar disorder than valproate, while the drugs may be equally effective in reducing suicidality among bipolar patients.
The first study, of more than 4000 Danish patients with bipolar disorder, found that patients taking lithium had fewer hospital visits and were less likely to need new medications than those taking valproate. Patients taking lithium had fewer admissions to a hospital for any type of episode. In addition, patients taking valproate had a higher rate of switching to or adding on treatment with antidepressants, antipsychotics, or anticonvulsants than those taking lithium. The study included up to 12 years of follow-up with the patients and is the largest study with the longest period of follow-up of patients taking valproate or lithium to date. Results were published by Lars Kessing et al. in the British Journal of Psychiatry in July 2011.
In the other study, a randomized controlled trial of 100 patients with bipolar disorder who had attempted suicide at least once in the past, Maria Oquendo of Columbia University found that there were no significant differences in number of suicide attempts, hospitalizations for suicide attempts, or time to a new attempt between patients taking lithium and those taking valproate over a follow-up period of 2.5 years.
Forty-five suicide events, which included attempts, hospitalizations, and changes to medication in response to suicide plans, were experienced by 35 patients (16 who were taking lithium and 19 who were taking valproate). Eighteen suicide attempts were made by 6 patients taking lithium and 8 taking valproate. There were no suicide completions during this study, which was published in Volume 168 of the American Journal of Psychiatry in 2011.
Editor’s Note: Suicide attempts are much more common than completed suicides. It appears that the second study was not large enough or long enough to detect differences in the rate of completed suicides. Older naturalistic studies suggest that treatment results in low suicide rates and that in patients who stop treatment with lithium, the rate of suicide attempts and completion increases dramatically. This is another reason for good responders to treatment regimens that include lithium to continue taking their medications.
Childhood Bipolar Disorder Still Poorly Treated
Kathleen Merikangas of the National Institute of Mental Health (NIMH) gave a plenary presentation on developmental manifestations of the bipolar spectrum at the 2011 Pediatric Bipolar Disorder Conference in Cambridge, Massachusetts this past March, which was sponsored by Massachusetts General Hospital and the Ryan Licht Sang Foundation. There were several striking take-away messages from her epidemiological research. She found that:
- Rates of bipolar disorder in childhood were relatively similar to rates among adults
- Only 22% of youth with bipolar spectrum diagnoses actually obtained mental health treatment for their conditions
- There was no evidence that these children were being over-medicated, as some non-epidemiological reports had suggested
She also reported that those with subthreshold bipolar spectrum disorders, i.e. those not meeting strict criteria for BP-I (including full-blown mania) or BP-II (including hypomania for four or more days) still were very ill and had considerable disability and dysfunction.
Merikangas reported on interviews of 10,123 youth aging from 13 to 18 found in the National Comorbidity Survey Replication Adolescent Supplement (NCS-A), and found rates of illness among the youth similar to those seen in adults. However, these children with bipolar spectrum disorders were more than ten times more likely to be on antidepressants than mood stabilizers, and more than four times more likely to be on antidepressants than atypical antipsychotics, again suggesting these children were not receiving the treatments recommended by consensus guidelines.
Risks and Difficulties of Treating Childhood-Onset Bipolar Disorder
 Early treatment is needed in childhood onset bipolar disorder
Early treatment is needed in childhood onset bipolar disorder
Multiple factors make childhood-onset bipolar disorder a difficult problem for affected children and families. Early onset is common, and treatment is often delayed or inappropriate. It takes an average of nine months to achieve remission, and relapses are common. In studies children have remained symptomatic for an average of two-thirds of the time they receive naturalistic follow up treatment, and the illness impairs social and educational development. Episodes and stressors tend to accumulate, and substance abuse is a frequent complication. Dysfunction and disability occur at a high rate among children with the illness, and suicidal ideation and acts are common.
When we surveyed adults in our treatment network, the Bipolar Collaborative Network (BCN), about the history of their illness, we found that the duration of the time lag between illness onset and first treatment was independently related to a poor outcome in adulthood. A longer delay to first treatment was associated in adulthood with greater depression severity, more days depressed, fewer days euthymic, more episodes, and more ultradian cycling (or cycling within a single day). Because treatment delay is a risk factor that can be avoided or prevented, efforts should be made to initiate treatment early in the course of bipolar illness. Read more
RTMS Versus ECT
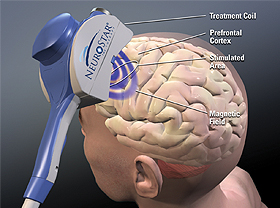
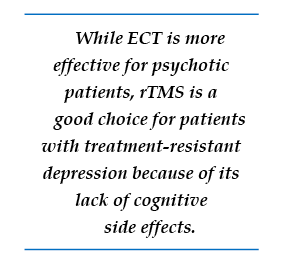 We’ve been posting about repeated transcranial magnetic stimulation (rTMS), a treatment in which a magnetic field is applied to a patient’s head, where it is able to affect tissue 2-3 centimeters into the brain.
We’ve been posting about repeated transcranial magnetic stimulation (rTMS), a treatment in which a magnetic field is applied to a patient’s head, where it is able to affect tissue 2-3 centimeters into the brain.
In randomized, controlled, head to head comparisons of electroconvulsive therapy (ECT) and repeated transcranial magnetic stimulation (rTMS), ECT often proves superior, particularly for a more severe psychotic or medically compromised patient. Nonetheless, for a more routine patient with non-psychotic depression, multiple studies have shown approximate equivalence of rTMS and ECT, while rTMS may have a superior benefit-to-risk ratio because it brings less risk of cognitive dysfunction. Thus, given almost equivalent efficacy for some subgroups of depressed patients, and a clear advantage for rTMS in terms of lack of cognitive side effects, this editor/clinician would recommend a course of rTMS prior to a series of ECT for the subgroup of non-emergency treatment-resistant depressed patients.
However, for highly treatment-refractory, severe, and particularly psychotic depression, few treatments appear to approach the efficacy and rapid response onset of electroconvulsive therapy (ECT). ECT as given in the modern era involves anesthesia and muscle paralysis while the patient is mechanically ventilated in order to prevent any damage from muscle contractions during the seizure. Read more
RTMS Parameters
 As we wrote yesterday, repeated transcranial magnetic stimulation (rTMS) is a treatment in which a magnetic field is applied to a patient’s head, where it is able to affect tissue 2-3 centimeters into the brain. The major studies of rTMS, by O’Reardon and colleagues (2007) and George et al. (2010), were performed with patients who were medication-free during the course of rTMS treatment. However, it is routine clinical practice to use rTMS as an adjunctive treatment to ongoing antidepressant therapy, and in these cases, response rates appear to be close to 50%, even in patients with considerable treatment resistance to prior antidepressants.
As we wrote yesterday, repeated transcranial magnetic stimulation (rTMS) is a treatment in which a magnetic field is applied to a patient’s head, where it is able to affect tissue 2-3 centimeters into the brain. The major studies of rTMS, by O’Reardon and colleagues (2007) and George et al. (2010), were performed with patients who were medication-free during the course of rTMS treatment. However, it is routine clinical practice to use rTMS as an adjunctive treatment to ongoing antidepressant therapy, and in these cases, response rates appear to be close to 50%, even in patients with considerable treatment resistance to prior antidepressants.
Using the FDA-approved parameters, treatment is typically delivered with with an rTMS machine that stimulates the left prefrontal cortical area of the brain at a stimulation intensity of 120% of the patient’s motor threshold at a frequency of magnetic impulses of 10 per second or 10 Hz. The motor threshold is the intensity of stimulation necessary to cause the thumb to move when the motor cortex is stimulated, but the treatment is given over the frontal cortex which does not produce any movements or other sensations.
Each treatment lasts for about 20 minutes and does not require any anesthesia or premedication. The patient is awake and alert during the procedure, and cognitive side effects are minimal. Patients occasionally experience some pain from contraction of the scalp muscles under the magnet.
The rapid reversal of the magnetic field occurring ten times per second induces electrical stimulation of the brain at the same frequency and causes discharge of neurons. High frequency (at 10 or 20Hz) neuronal activity appears to increase activity (blood flow or metabolism) in the brain, while lower frequency stimulation, such as at 1 Hz, appears to decrease brain activity. In both cases, the effects last at least 48 hours after the last of a two- or three-week series of treatments. RTMS increases brain-derived neurotrophic factor (BDNF) in the brain, and BDNF is released when nerves fire at a fast frequency. The release of BDNF appears to be necessary for long-term learning and memory.
Sitting passively versus receiving therapy during rTMS
In clinical practice, most treatments are administered by a technician. However, in some instances, clinicians engage patients in forms of active psychotherapy while they are receiving the rTMS. Read more
Repeated Transcranial Magnetic Stimulation Now More Widely Available
 As reported in the BNN last year, a study by George and colleagues that was published in the Archives of General Psychiatry provided independent support and replication of earlier findings that active repeated transcranial magnetic stimulation (rTMS) is more effective than a sham procedure in the treatment of partially drug-resistant depressed patients.
As reported in the BNN last year, a study by George and colleagues that was published in the Archives of General Psychiatry provided independent support and replication of earlier findings that active repeated transcranial magnetic stimulation (rTMS) is more effective than a sham procedure in the treatment of partially drug-resistant depressed patients.
RTMS is a treatment in which a magnetic field is applied to a patient’s head, where it is able to affect tissue 2-3 centimeters into the brain. According to Neuronetics, the company that produces the rTMS machine, “The magnetic field passes through the hair, scalp, and skull and into the prefrontal cortex unimpeded. This method allows for precise, targeted stimulation, minimizing the stimulation of brain tissue not involved in mood.” The Federal Drug Administration approved the Neuronetics rTMS machine after a large, multi-center sham-controlled study was published by O’Reardon et al. in Biological Psychiatry in 2007. Since the FDA approval, availability of rTMS treatment and insurance reimbursement for the procedure have improved.
Covering the cost of treatment
A number of hospitals and private practitioners around the country are now able to offer treatment with rTMS. The Neuronetics website allows patients to search for sites where the treatment is offered. While a treatment sequence typically consisting of treatment five times a week for four to six weeks is relatively expensive (often in the range of $8,000-$12,000 or more for the series), some health insurance plans will now (perhaps after some argument and negotiation) cover some of the cost of treatment. It was estimated by Neuronetics personnel that about 75% of the time, with the assistance of Neuronetics and the physician staff delivering the rTMS, such insurance coverage can successfully be arranged. Neuronetics suggested that even if the claim is initially rejected, many treatment series will eventually be covered.
Neuronetics also provides assistance for patients with annual income under $42,000. These patients may be able to receive treatment free of charge. In addition, for those who have a higher income but are uninsured, Neuronetics offers a loan program for the gradual repayment of the cost of the procedure.
Stay tuned for more articles about rTMS this week!
Treatment Plans for Maladaptive Impulsive Aggression in Children
Maladaptive impulsive aggression often co-occurs with other psychiatric illnesses in children, so it can be difficult to find treatment solutions. A symposium at the 57th Annual Meeting of the American Academy of Child and Adolescent Psychiatry yielded some suggestions. Read on for an overview of impulsive aggression and possible treatment plans.
At the symposium, held in New York Oct. 26-31, 2010, panelists called maladaptive aggression the “fever” of child psychiatry (because it is common but also nonspecific) and described the phenomenon as “the language of the inarticulate.” The panelists drew a distinction between impulsive aggression, which describes behavior that is unplanned, unprofitable, and poorly controlled, and another phenomenon, predatory aggression, which describes behavior that is planned, sometimes profitable, and highly controlled.
The speakers on the panel indicated that impulsive aggression is related to other psychiatric syndromes including depression, attention deficit hyperactivity disorder (ADHD), mania, conduct disorder, oppositional defiant disorder, anxiety, post-traumatic stress disorder (PTSD), borderline personality disorder, autism, and schizophrenia. This raises problems for drug development, as Tom Laughren of the Federal Drug Administration (FDA) indicated in one talk at the symposium, because when new treatments are developed, they are studied in the context of only one primary disorder. Read more
Diet, Depression, Inflammation and the Brain
We’ve been posting recently about diet and about treatments that are weight-neutral. There is evidence that diet, inflammation and depression are all linked. Epidemiological studies by Joe Hiblen have shown that in countries whose populations eat more fish and thus have high levels of omega-3 fatty acids in their diet, there is lower incidence of depression, suicide, and cardiovascular disease such as heart attacks and strokes. This may be because the major omega-3 fatty acids, EPA and DHA, are anti-inflammatory, and inflammation has been linked to depression. EPA inhibits the enzymes phospholipase A2 and cyclo-oxygenase-2 (COX-2), and their subsequent inflammatory effects on cytokines. DHA inhibits the pro-inflammatory cytokine IL6.
Researcher John Davis recently reviewed relevant literature and found that diets high in anti-inflammatory omega-3 fatty acids are associated with lower incidence of depression, cardiovascular disease, and markers of inflammatory processes. Conversely, diets high in fat and in inflammatory omega-6 fatty acids are associated with obesity, depression, and cardiovascular disease.
Various studies have shown the links between inflammation and depression. For example, when patients are given alpha-interferon to treat viral hepatitis, there is a subsequent increase in inflammatory cytokines IL-1 and IL-6, and depression often follows. Also, depressed patients have an increased ratio of pro-inflammatory to anti-inflammatory cytokines in their blood.
Another sign of a link between bipolar illness and inflammation can be seen in biochemical analysis of brain specimens obtained at autopsy. Researcher Rapaka Rao in the laboratory of Stanley Rapoport at the National Institute on Aging at the National Institutes of Health in Bethesda, Maryland, has reported that increased markers of neuronal inflammation and excitotoxicity were found in the brains of people who had had bipolar disorder. Phospholipase A2 and COX-2 were significantly elevated in the brains of those with bipolar illness and those with schizophrenia compared with controls. Pro-inflammatory interleukin I was also significantly increased in the brains of those who had had either illness. Read more
The Evolving Omega-3 Fatty Acid Story: The Icing on the Cake (And Why It Shouldn’t Be Eaten)
 Omega-3 fatty acids are important for brain development and function and are essential to the human diet since they cannot be synthesized by the body. Omega-3 fatty acids are derived from canola oil, walnuts, flax seed oil, leafy vegetables, and especially fish. The main omega-3 fatty acids include eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). They have anti-inflammatory effects, unlike omega-6 fatty acids, which are pro-inflammatory. The omega-6 fatty acids come from soy, peanuts, corn oil, and meats, and are associated with increases in obesity, myocardial infarction, and stroke.
Omega-3 fatty acids are important for brain development and function and are essential to the human diet since they cannot be synthesized by the body. Omega-3 fatty acids are derived from canola oil, walnuts, flax seed oil, leafy vegetables, and especially fish. The main omega-3 fatty acids include eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). They have anti-inflammatory effects, unlike omega-6 fatty acids, which are pro-inflammatory. The omega-6 fatty acids come from soy, peanuts, corn oil, and meats, and are associated with increases in obesity, myocardial infarction, and stroke.
In a recent review of the literature, John Davis and Joe Hiblen found that diets that include high levels of omega-3 fatty acids are associated with decreased incidence of depression, suicide, and cardiovascular disease. The researchers performed a meta-analysis of all the prospective depression treatment studies of omega-3 fatty acids compared to placebo. They found that EPA had antidepressant effects in humans, with moderate effect size and a high degree of statistical significance. DHA, however, did not appear to have an antidepressant effect, and pure DHA was even associated with some worsening of depression.
Editor’s note: This meta-analysis helps clarify some of the ambiguities in the literature about the antidepressant efficacy of the omega-3 fatty acids, clarifying that EPA alone is an effective antidepressant. The one study that did not find antidepressant effects with EPA was carried out by the Bipolar Collaborative Network, in which I am an investigator. Our study, published in an article by Keck et al., showed that 6g of EPA was not significantly more effective than placebo in bipolar depression or in rapid cyclers. However, there is some indication that 6g may be too high a dose of EPA, and most of the recommendations now suggest using 1-2g of either EPA or an EPA/DHA combination. Read more





