Tests of Generic Lamotrigine Successful
Studies published in 2015 and 2016 have established that generic versions of the anti-convulsant lamotrigine are bioequivalent to the name-brand drug (Lamictal) and to each other. Lamotrigine is used to treat epilepsy and is also prescribed for the prevention of bipolar depression.
An article by T.Y. Ting and colleagues in the journal Epilepsia in 2015 established that generic lamotrigine works similarly enough to the name brand drug that patients with epilepsy could be switched from one drug to the other without worsening seizures. More recently, M.D. Privitera and colleagues reported in the journal Lancet Neurology that different generic versions of lamotrigine were bioequivalent. No significant changes in seizure frequency or other negative outcomes were reported.
These studies show that generic versions of lamotrigine have the same anticonvulsant effectiveness as the original drug. The same should also be true for lamotrigine’s effectiveness in preventing bipolar depression.
Clarifying the Effects of a Diabetes Drug that Improves Bipolar Depression
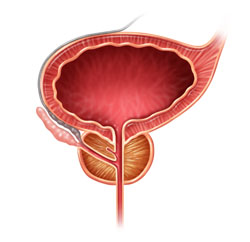
Research continues on pioglitazone, a drug typically used to treat diabetes but with other positive effects on depression and stroke risk. Some researchers are working on determining whether the drug increases the risk of developing certain cancers, including bladder, prostate, and pancreatic cancers. A recent study by James D. Lewis and colleagues in the journal JAMA found no statistically significant increase in risk of bladder cancer among patients taking the drug, but the researchers said they also couldn’t rule out that the drug may increase this risk, as has been seen in previous studies. The study by Lewis did show an increase in pancreatic and prostate cancers in patients taking pioglitazone, but the researchers did not determine whether this was caused by the drug.
Another recent study by Walter N. Kernan and colleagues in the New England Journal of Medicine reported that pioglitazone reduced the incidence of stroke and heart attack in patients with a history of stroke or blocked blood vessels in the brain but without a diagnosis of diabetes. Patients who received pioglitazone also experienced side effects including weight gain, edema (an increase in fluids in the body’s tissues) and serious bone fractures.
Pioglitazone has had positive effects in bipolar depression and may one day be used as a treatment for bipolar disorder. For now, it may be worthy of consideration for the treatment of diabetes in patients who also have bipolar depression.
Very Low Doses of Opioid Buprenorphine May Reduce Suicidal Ideation
There is no perfect treatment to reduce the risk of suicide in someone who is considering it. Antidepressants can reduce suicidal ideation, but they take several weeks to start working. Intravenous ketamine is used at higher doses as an anesthetic, but in low doses works quickly to reduce suicidal thoughts. However, it requires repeated infusions to keep working. Researchers led by Yoram Yovell are exploring another option: ultra-low doses of the opioid buprenorphine.
In a study published in the American Journal of Psychiatry in 2015, Yovell and colleagues compared low-dose buprenorphine to placebo in 62 patients with no history of substance abuse who had been contemplating suicide for a week or more. Many had attempted suicide before, and more than half met the criteria for borderline personality disorder.
Buprenorphine was administered under the tongue, in doses of 0.1 mg once or twice a day. The researchers used these low doses to minimize the side effects of a drug that could potentially be addictive. Those randomized to receive buprenorphine saw greater reductions in suicidal ideation compared to those who received placebo, both after two weeks and after four weeks.
Use of antidepressants did not affect the likelihood that patients would respond to buprenorphine. The researchers suggest that buprenorphine specifically treats suicidal thoughts, rather than improving depression in general.
Patients with borderline personality disorder, who are often unresponsive to medication, also saw improvement in suicidal ideation after taking buprenorphine, suggesting that the opioid treated a particular symptom of their disorder—sensitivity to feelings of separation from the people with whom they are close.
Patients did not experience withdrawal when they discontinued buprenorphine. Side effects included fatigue, nausea, dry mouth, and constipation. Patients who started out taking 0.2 mg per day were much more likely to drop out than those who started at 0.1 mg per day.
There is another reason the researchers used very low doses. A potential benefit to ultra-low–dose buprenorphine is that even a week’s supply of the drug would not produce a dangerous overdose, so patients could potentially be prescribed a week’s worth of medication to take at home instead of in an inpatient setting.
Buprenorphine is not recommended for patients with a history of substance abuse. The study only explored short-term use of the drug, and replication studies are needed to clarify its effects.
Anxiety, Depression, Unstable Mood, and Low-Level Mania Best Predictors of Bipolar Disorder
Researchers are looking for better ways of predicting whether children at risk for bipolar disorder will go on to develop the illness. A 2015 study by David Axelson and colleagues in the American Journal of Psychiatry reported that in the offspring of parents with bipolar disorder, diagnoses of sub-threshold mania, depression, and disruptive behavior disorders were associated with subsequent diagnosis of full-blown Bipolar I or Bipolar II disorders six to seven years later.
More recently, in an article by Danella M. Hafeman and colleagues in the American Journal of Psychiatry, the same group of investigators has examined how symptoms (rather than categorical diagnoses, as in the earlier study) predict the development of bipolar disorder. In children and adolescents at high risk for bipolar disorder (because they have a parent with the disorder) three types of symptoms were the best predictors of later bipolar disorder: anxiety/depression at the time participants entered the study, unstable mood or irritability both when entering the study and shortly before a bipolar diagnosis, and low-level manic symptoms observed shortly before diagnosis.
The earlier the age at which a parent was diagnosed with a mood disorder, the greater the risk that the offspring would also be diagnosed with bipolar disorder. Youth with all four risk factors (anxiety or depression, mood changes, low-level mania, and a parent who was diagnosed with a mood disorder at an early age) had a 49 percent chance of developing bipolar disorder, compared to a 2 percent chance among those without those risk factors.
Childhood onset of bipolar disorder and long delays until first treatment for depression or mania are both significant predictors of a poor outcome in adulthood compared to adult onsets and shorter delays to treatment. Read more
Psychotherapy Improves Outcomes for People with Bipolar Disorder
Studies have shown that therapy can be helpful for people with bipolar disorder. In a 2016 article in the British Journal of Psychiatry, researchers led by M. Oud described the findings of their systematic review of studies evaluating different types of therapy for bipolar disorder. The research team reviewed the findings of 55 randomized controlled trials of psychotherapeutic interventions that included a total of 6,010 adult participants with bipolar disorder. The team found moderate-quality evidence that psychological interventions reduced relapses following treatment, and that collaborative care reduced hospital admissions for adults with bipolar disorder. Oud and colleagues found lower-quality evidence that group interventions reduced depression relapses following treatment, and that family psychoeducation reduced symptoms of depression and mania.
The reseachers concluded that there is evidence that therapy can be helpful for people with bipolar disorder. Since some of the evidence was of low quality, more research is needed to identify the most effective therapies for different phases of bipolar disorder.
Editor’s Note: The data are clear that therapy is helpful. In particular, one approach worth emulating is that described in an article by Lars V. Kessing and colleagues in the British Journal of Psychiatry in 2013. They found that comprehensive care in an outpatient mood disorder clinic, which included psychotherapy, psychoeducation, mood monitoring, and drug treatment, reduced relapses significantly compared to treatment as usual.
Treating Prenatal Depression Improves Outcomes for Mothers and Babies
 A recent study confirms that women who are depressed during pregnancy are more likely to experience adverse pregnancy outcomes such as preterm or cesaerean delivery and small or underweight babies. However, antidepressant treatment improved outcomes for pregnant women with depression.
A recent study confirms that women who are depressed during pregnancy are more likely to experience adverse pregnancy outcomes such as preterm or cesaerean delivery and small or underweight babies. However, antidepressant treatment improved outcomes for pregnant women with depression.
The 2016 study by Kartik K. Venkatesh and colleagues in the journal Obstetrics & Gynecology included 7,267 women who gave birth after at least 20 weeks of pregnancy. About 11% of the women screened positive for depression during their pregnancy. Depressed mothers-to-be were more likely to give birth before 37 weeks and before 32 weeks compared to nondepressed mothers-to-be. The depressed women were also more likely to deliver small babies or babies weighing under 2500g.
About 7% of the women in the study received antidepressant medication. Compared to nondepressed women, the women taking antidepressants did not have greater rates of early delivery or small babies. However, the authors caution that because so few women received antidepressants, the study does not reveal whether antidepressants improve outcomes for depressed pregnant women.
Oxytocin May Reduce PTSD Symptoms
 The hormone oxytocin, best known for creating feelings of love and bonding, may help treat post-traumatic stress disorder, since it also reduces anxiety. A study by Saskia B.J. Koch and colleagues that will soon be published in the journal Neuropsychopharmacology reports that a single intranasal administration of oxytocin (at a dose of 40 IU) reduced anxiety and nervousness more than did placebo among police officers with PTSD.
The hormone oxytocin, best known for creating feelings of love and bonding, may help treat post-traumatic stress disorder, since it also reduces anxiety. A study by Saskia B.J. Koch and colleagues that will soon be published in the journal Neuropsychopharmacology reports that a single intranasal administration of oxytocin (at a dose of 40 IU) reduced anxiety and nervousness more than did placebo among police officers with PTSD.
Oxytocin also improved abnormalities in connectivity of the amygdala. Male participants with PTSD showed reduced connectivity between the right centromedial amygdala and the left ventromedial prefrontal cortex compared to other male participants who had also experienced trauma but did not have PTSD. This deficit was corrected in the men with PTSD after they received a dose of oxytocin. Female participants with PTSD showed greater connectivity between the right basolateral amygdala and the bilateral dorsal anterior cingulate cortex than female participants who had experienced trauma but did not have PTSD. This was also restored to normal following a dose of oxytocin.
These findings suggest that oxytocin can not only reduce subjective feelings of anxiety in people with PTSD, but may also normalize the way fear is expressed in the amygdala.
Inflammation Linked to Bipolar Illness in Young People
 The Course and Outcome of Bipolar Youth study, or COBY, has been collecting information on young people with bipolar disorder and tracking their symptoms into adulthood since 2000. A 2015 study by Benjamin I. Golstein in the Journal of Clinical Psychiatry analyzed COBY data, identifying links between higher than average levels of inflammatory markers measured in the blood and participants’ histories of illness and familial risk factors.
The Course and Outcome of Bipolar Youth study, or COBY, has been collecting information on young people with bipolar disorder and tracking their symptoms into adulthood since 2000. A 2015 study by Benjamin I. Golstein in the Journal of Clinical Psychiatry analyzed COBY data, identifying links between higher than average levels of inflammatory markers measured in the blood and participants’ histories of illness and familial risk factors.
High levels of the inflammatory marker hsCRP were associated with longer duration of illness, substance use disorder, and family history of suicide attempts or completed suicides. High levels of TNF-alpha were linked to suicide attempts, self-injury behaviors, and family history of substance use disorders. IL-6 was also linked to family history of substance use disorders.
There were also links between inflammatory markers and participants’ symptoms over the 6 months leading up to the blood tests. Levels of the inflammatory marker TNF-alpha were linked to the percentage of weeks patients had psychotic symptoms. Levels of IL-6 were associated with percentage of weeks with subthreshold mood symptoms and also with any suicide attempt. Levels of HsCRP were linked to maximum severity of depressive symptoms.
It is possible that targeting the elevated levels of inflammatory markers with anti-inflammatory treatments could improve patients’ response to treatments, but this topic requires further study.