Heading Off Early Symptoms of Bipolar Disorder in Children at High Risk
 At the American Academy of Child and Adolescent Psychiatry (AACAP) annual meeting in Toronto in October 2011, there was a symposium on risk and resilience factors in the onset of bipolar disorder in children who have a parent with the disorder.
At the American Academy of Child and Adolescent Psychiatry (AACAP) annual meeting in Toronto in October 2011, there was a symposium on risk and resilience factors in the onset of bipolar disorder in children who have a parent with the disorder.
Family Focused Therapy Highly Encouraged
Amy Garrett reported that family focused therapy (FFT) in those at risk for bipolar disorder was effective in ameliorating symptomatology compared to treatment as usual. Family focused therapy, pioneered by Dave Miklowitz, PhD of UCLA involves three components. The first component is education about the illness and methods of self-management. The second is enhancement of communication in the family with practice and rehearsal of new modes of conversation. The third component is assistance with problem solving.
In Garrett’s study, 50 children aged 7 to 17 were randomized to family focused treatment or treatment as usual. These children were not only at high risk for bipolar disorder, they were already prodromal, meaning they were already diagnosable with bipolar not otherwise specified (BP-NOS), cyclothymia, or major depressive disorder, and had also shown concurrent depressive and/or manic symptoms in the two weeks prior to the study. At baseline, compared to controls, these children at high risk for full-blown bipolar disorder by virtue of a parental history of the illness showed increased activation of the amygdala and decreased activation of the prefrontal cortex. Most interestingly, after improvement with the family focused therapy (FFT), amygdala reactivity to emotional faces became less prominent and dorsolateral prefrontal cortical activity increased in proportion to the degree of the patient’s improvement.
The discussant for the symposium was Kiki Chang of Stanford University, who indicated that the results of this study of family focused therapy were already sufficient to convince him that FFT was a useful therapeutic procedure in children at high risk for bipolar disorder by virtue of having a parent with a history of bipolar illness. Chang is now employing the therapy routinely in all of his high-risk patients.
Editors Note: This is an extremely important recommendation as it gives families a specific therapeutic process in which to engage children and others in the family when affective behavior begins to become abnormal, even if it does not meet full criteria for a bipolar I or bipolar II disorder.
FFT also meets all the important criteria needed for putting it into widespread clinical practice. Family focused therapy has repeatedly been shown to be effective in adults and adolescents with bipolar illness and now also in these children who are prodromal. The psychoeducational part of FFT is common sense, and dealing with communication difficulties and assisting with problem solving also have merit in terms of stress reduction. Finally, this treatment intervention appears to be not only safe but also highly effective in a variety of different prodromal presentations of affect disorders even if children do not meet full criteria for bipolar disorder. While the few studies of early intervention with psychopharmacological agents have not yet identified efficacious medications for the prodromes of bipolar disorder and in particular medications with a high degree of safety, such family focused therapy appears to be an ideal early intervention.
I would concur with Dr. Chang’s assessment. Family focused therapy (FFT) should be offered to all children with this high-risk status who have begun to be symptomatic. Early onset of unipolar depressive disorder or of bipolar disorder carries a more adverse prognosis than the adult onset variety and thus should not be ignored. If more serious illness is headed off early, it even raises the possibility that the full-blown illness will not develop at all.
Gray Matter Volume Abnormalities
Tomas Hajek of Dalhousie University in Halifax presented data indicating that in children at high risk for bipolar disorder, gray matter volume in the right inferior frontal gyrus is increased. Read more
Quetiapine May Be an Effective Monotherapy for Bipolar I
 An article published by Weisler et al. last year in the Journal of Clinical Psychiatry suggests that quetiapine may be effective as a monotherapy maintenance treatment for bipolar I disorder. It has previously been shown to work in combination with lithium or divalproex and is approved by the Federal Drug Administration for this combination treatment.
An article published by Weisler et al. last year in the Journal of Clinical Psychiatry suggests that quetiapine may be effective as a monotherapy maintenance treatment for bipolar I disorder. It has previously been shown to work in combination with lithium or divalproex and is approved by the Federal Drug Administration for this combination treatment.
Adult patients diagnosed with bipolar I disorder who were currently or recently in a mood episode received open-label quetiapine in doses of 300-800mg per day for up to 24 weeks. Patients who became stable either remained on quetiapine or were switched to lithium (at doses of 0.6-1.2 mEq/L) or placebo. This double-blind phase of the study continued for up to 104 weeks.
The study began with 2,438 patients, 1,172 of whom made it to the second phase of the trial. On the main outcome measure of time to recurrence of any mood event, both quetiapine and lithium were significantly better than placebo.
Editor’s Note: In the 50% of patients with a recent mood episode who were able to be stabilized on quetiapine monotherapy, those who remained on long-term quetiapine or those who switched to lithium were both much less likely to have subsequent relapses into either depression or mania than those who switched to placebo. Whether Astra-Zeneca, the company that produces quetiapine, will file to gain Federal Drug Administration approval of quetiapine monotherapy for long-term preventive treatment is not known.
Creative People More Likely to Have Mental Illness
According to a large family study of people with severe mental disorders that was published by Kyaga et al. in the British Journal of Psychiatry last year, people with bipolar disorder and siblings of people with schizophrenia or bipolar disorder were much more likely to be working in creative professions than people without severe mental illness.
Kyaga talked to Medscape Medical News about the study:
“I think the study stresses the importance of treating all patients individually, and with the aim of finding the optimal treatment with regards to effectiveness, while minimizing the adverse effects that medication can have on positive aspects of psychiatric disorders,” Dr. Kyaga said.
“We often encounter the suggestion that lithium reduces creativity in patients with bipolar disorder and that adherence therefore is difficult. Now we can say that it is true that bipolar disorder is in fact associated with increased creativity, but we also know from previous research that terminating treatment with lithium in bipolar disorder will, in the long run, disrupt creative behavior,” he continued.
“We therefore need to pay close attention to what patients tell us while being treated, so that we can find a regimen that will work for them to prevent the disastrous consequences of severe psychiatric disorder, while providing them opportunities to uphold their creative behaviors in the long run,” Dr. Kyaga said.
Lamotrigine Effective Adjunct for Lithium in Bipolar Disorder
 In a long-term study of bipolar patients taking lithium published in Bipolar Disorders last year, the addition of lamotrigine (or paroxetine for those who did not respond to lamotrigine) was significantly better than the addition of placebo. Patients taking lamotrigine with lithium averaged 10 months until a recurrence of a depressive or manic episode, while patients taking placebo with lithium averaged 3.5 months until an episode.
In a long-term study of bipolar patients taking lithium published in Bipolar Disorders last year, the addition of lamotrigine (or paroxetine for those who did not respond to lamotrigine) was significantly better than the addition of placebo. Patients taking lamotrigine with lithium averaged 10 months until a recurrence of a depressive or manic episode, while patients taking placebo with lithium averaged 3.5 months until an episode.
Among Bipolar Patients, Women Spend More Time Depressed Than Men Do
An article by Lori Altshuler et al. (including this editor Robert M. Post) published in the American Journal of Psychiatry in 2010 presents research that among bipolar patients studied over a period of 7 years, women spent more time than men depressed. Women had higher rates of rapid cycling and of anxiety disorders, both of which were associated to higher rates of depression.
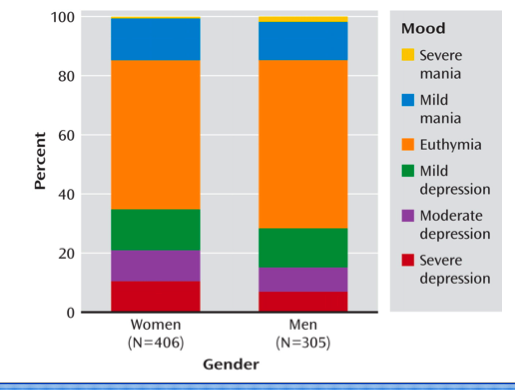
Proportion of Time Spent Ill During Clinical Visits for Women and Men With Bipolar I or II Disorder (N=711)aaWomen and men, 35.6% compared with 28.7% of visits depressed; 50.4% compared with 56.9% of visits euthymic; 14.1% compared with 14.4% of visits hypomanic or manic.
Sleep Apnea Common Among Rapid Cyclers
Kellen and colleagues presented a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, in which they reported that 21% of patients with rapid cycling bipolar disorder have confirmed sleep apnea. Since many patients who screened positive for sleep apnea on the study’s sleep questionnaire did not undergo follow-up sleep studies to confirm the diagnosis, it is estimated that up to 40% of rapid cycling patients may, in fact, have sleep apnea.
Editor’s note: Given such a high incidence of sleep apnea among rapid cycling bipolar patients, it would be prudent for patients and clinicians to be alert to the possibility of sleep apnea and follow up with appropriate sleep studies. Sleep apnea can cause daytime fatigue, cognitive dysfunction, and treatment resistance, so its identification and treatment with continuous positive airway pressure (CPAP) may be enormously beneficial to a substantial number of rapid cycling bipolar patients. A just-published article by Sukys-Claudino in Sleep Medicine presents findings that compared to placebo, the anti-Alzheimer’s drug donepezil (Aricept) started at 5mg/day for 2 weeks and then increased to 10 mg given twice a day (20 mg/day total) helped all measures of sleep apnea including daytime sleepiness.
Clinical hints that a patient may be suffering from sleep apnea include loud snoring, long pauses between breaths, and non-restorative sleep. The likelihood of sleep apnea increases with age and with overweight or obesity.
Antioxidants May Be Deficient in Patients with Bipolar Disorder, NAC May Help
In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Guy Goodwin and colleagues reported that relative to controls, blood from patients with bipolar disorder contained more total glutathione, a potent antioxidant, and a higher ratio of oxidized to reduced glutathione. Measurements of blood glutathione could eventually serve as a biomarker, suggesting when a diagnosis of bipolar disorder is likely.
Editor’s note: Glutathione is one of the major antioxidants in humans. Oxidized glutathione is a less active form, so the higher levels of oxidized glutathione compared to reduced glutathione in patients with bipolar disorder suggests they may have a relative deficiency of the active form. These data are consistent with reports that patients in manic and depressive phases of bipolar disorder have increased oxidative stress and free radicals that impair cellular functioning.
Together, these results highlight the potential utility of treatments that increase antioxidant activity. One option is N-acetylcysteine (NAC), which the body converts into glutathione. As previously noted in the BNN, Michael Berk reported in Biological Psychiatry in 2008 that NAC (1000 mg twice a day) appears to exert greater antidepressant effects over a period of 24 weeks than placebo when added into previously ineffective regimens in patients with bipolar disorder.
In another poster at the conference, Magalhaes and colleagues reported on NAC treatment for a subgroup of the bipolar patients in the study by Berk who were in a major depressive episode at the time of the study. They found that NAC had highly significant acute antidepressant effects of large magnitude in this subgroup of patients.
The glutathione data by Goodwin et al. provide a further rationale for consideration of the use of NAC in bipolar disorder, particularly in the acute and longer-term treatment of the depressive phases. As we reported in BNN Issue 1 from 2010, NAC also exerts positive effects in many illnesses that commonly occur comorbidly with bipolar disorder. These include cocaine and heroin addiction, gambling addiction, obsessive compulsive disorder (as an adjunct to selective serotonin reuptake inhibitors (SSRIs)), and trichotillomania (compulsive hair-pulling).
Aripiprazole Makes Lamotrigine More Effective
 In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
Editor’s note: These data add to a growing literature that shows that an atypical antipsychotic added to a mood stabilizer is associated with better prophylactic effects than use of the mood stabilizer alone. Previously, most of the studies of this type of combination used lithium or valproate as the mood stabilizer and, to our knowledge, this is the first to demonstrate that long-term prevention with lamotrigine is enhanced by the addition of an atypical antipsychotic.
Many of the atypical antipsychotics are FDA-approved as adjunctive treatments to mood stabilizers in the long-term treatment of bipolar disorder. The controlled clinical trial data that led to this FDA approval support the practice of many clinicians who prescribe combination treatment rather than monotherapy in order to achieve a more rapid onset of anti-manic stabilization and longer-term maintenance effects. The use of aripiprazole and quetiapine as adjuncts to lithium and valproate is particularly common in bipolar disorder since the same atypical antipsychotics are FDA-approved as adjunctive treatments in unipolar depression, and clinicians are familiar with prescribing them to improve ineffective acute antidepressant treatment.
Lithium More Effective than Valproate for Bipolar Disorder
 According to two studies in 2011, lithium is more effective in treating episodes of bipolar disorder than valproate, while the drugs may be equally effective in reducing suicidality among bipolar patients.
According to two studies in 2011, lithium is more effective in treating episodes of bipolar disorder than valproate, while the drugs may be equally effective in reducing suicidality among bipolar patients.
The first study, of more than 4000 Danish patients with bipolar disorder, found that patients taking lithium had fewer hospital visits and were less likely to need new medications than those taking valproate. Patients taking lithium had fewer admissions to a hospital for any type of episode. In addition, patients taking valproate had a higher rate of switching to or adding on treatment with antidepressants, antipsychotics, or anticonvulsants than those taking lithium. The study included up to 12 years of follow-up with the patients and is the largest study with the longest period of follow-up of patients taking valproate or lithium to date. Results were published by Lars Kessing et al. in the British Journal of Psychiatry in July 2011.
In the other study, a randomized controlled trial of 100 patients with bipolar disorder who had attempted suicide at least once in the past, Maria Oquendo of Columbia University found that there were no significant differences in number of suicide attempts, hospitalizations for suicide attempts, or time to a new attempt between patients taking lithium and those taking valproate over a follow-up period of 2.5 years.
Forty-five suicide events, which included attempts, hospitalizations, and changes to medication in response to suicide plans, were experienced by 35 patients (16 who were taking lithium and 19 who were taking valproate). Eighteen suicide attempts were made by 6 patients taking lithium and 8 taking valproate. There were no suicide completions during this study, which was published in Volume 168 of the American Journal of Psychiatry in 2011.
Editor’s Note: Suicide attempts are much more common than completed suicides. It appears that the second study was not large enough or long enough to detect differences in the rate of completed suicides. Older naturalistic studies suggest that treatment results in low suicide rates and that in patients who stop treatment with lithium, the rate of suicide attempts and completion increases dramatically. This is another reason for good responders to treatment regimens that include lithium to continue taking their medications.
Childhood Bipolar Disorder Still Poorly Treated
Kathleen Merikangas of the National Institute of Mental Health (NIMH) gave a plenary presentation on developmental manifestations of the bipolar spectrum at the 2011 Pediatric Bipolar Disorder Conference in Cambridge, Massachusetts this past March, which was sponsored by Massachusetts General Hospital and the Ryan Licht Sang Foundation. There were several striking take-away messages from her epidemiological research. She found that:
- Rates of bipolar disorder in childhood were relatively similar to rates among adults
- Only 22% of youth with bipolar spectrum diagnoses actually obtained mental health treatment for their conditions
- There was no evidence that these children were being over-medicated, as some non-epidemiological reports had suggested
She also reported that those with subthreshold bipolar spectrum disorders, i.e. those not meeting strict criteria for BP-I (including full-blown mania) or BP-II (including hypomania for four or more days) still were very ill and had considerable disability and dysfunction.
Merikangas reported on interviews of 10,123 youth aging from 13 to 18 found in the National Comorbidity Survey Replication Adolescent Supplement (NCS-A), and found rates of illness among the youth similar to those seen in adults. However, these children with bipolar spectrum disorders were more than ten times more likely to be on antidepressants than mood stabilizers, and more than four times more likely to be on antidepressants than atypical antipsychotics, again suggesting these children were not receiving the treatments recommended by consensus guidelines.