Memory Tips for Bipolar Disorder
 Like cancer patients undergoing chemotherapy, patients with bipolar disorder often have memory problems, particularly if they have had many prior episodes. Some memory tips from CancerCare’s Chemobrain Information Series may also help patients with bipolar disorder remember things better and keep their memory sharp. Here are some of their tips:
Like cancer patients undergoing chemotherapy, patients with bipolar disorder often have memory problems, particularly if they have had many prior episodes. Some memory tips from CancerCare’s Chemobrain Information Series may also help patients with bipolar disorder remember things better and keep their memory sharp. Here are some of their tips:
Make lists. Carry a notepad with you, or use a smartphone to keep track of errands, shopping lists, daily tasks, and when you should take your medications.
Use a paper or electronic day planner or a personal organizer to keep track of appointments and special days like birthdays or anniversaries.
Use a wall calendar and hang it in a place that you will see it multiple times per day.
Carry a notebook and record everything you need to remember, including to-do lists; the dates, times, and addresses of appointments; important telephone numbers; and the names of people you meet and a brief description of them. You can also use the notebook to keep track of medical information: your medication schedule, any symptoms or side effects you are having, or questions to ask your doctor. You can also do this using an app like What’s My M3 or by downloading a personal mood charting calendar from our website.
Leave yourself a voicemail message to remember something important. When you listen to it later, write down the information.
Organize your home or office. Keep things in familiar places so you always know where to find them.
Avoid distractions. Find a quiet, uncluttered place to work or think where you can focus your attention for longer.
Have conversations in quiet places. This will help you concentrate better on what the other person is saying.
Repeat information aloud, and write down important points. If someone gives you information about an appointment, you might repeat the time, date, and location of the appointment out loud while righting it down.
Keep your mind active. You can use crossword puzzles, word or math games, or attend events about topics that interest you.
When writing, proofread. Double-check whether you’ve used the correct words and spellings.
Train yourself to focus through mindfulness. For example, if you keep misplacing your keys, pay extra attention each time you set down your keys. You may say aloud, “I’m putting my keys down on the counter.” Hearing the auditory cue can boost your memory.
Exercise, eat well, and get plenty of rest and sleep. These habits will help your memory work best.
Tell your loved ones that you are having memory problems, so that they’ll understand that you may forget things you may normally be able to remember. They can help you or encourage you.
Low Omega-3s in Children Associated with Poor Cognitive Performance
Omega-3 fatty acids (especially the type known as DHA) are essential for brain development and functioning, but most people eating a modern western diet consume low amounts of these compared to omega-6 fatty acids. Omega-3s are anti-inflammatory while omega-6s are pro-inflammatory. A large UK study published in the journal PLOS One in 2013 reported that healthy 7- to 9-year-olds with lower levels of omega-3 long-chain polyunsaturated fatty acids in their blood (including DHA, DPA, and EPA) had lower reading ability and working memory, and also had more behavior problems.
The oils in fish are the best source of omega-3 fatty acids, and most of the children with poor reading ability in the study fell short of the UK nutritional guideline that recommends eating two portions of fish per week.
Girls in the study had more dramatic deficits in omega-3 levels than boys. In adults, women tend to metabolize long chain polyunsaturated fatty acids more easily than men, but this difference is driven by hormones, and because the girls in the study had not yet reached child-bearing age, they did not reflect this benefit.
Omega-3 deficits in children have been connected with attention deficit hyperactivity disorder (ADHD), and supplementation with extra omega-3 fatty acids in the diet has led to improvements in ADHD.
Caffeine Improves Memory
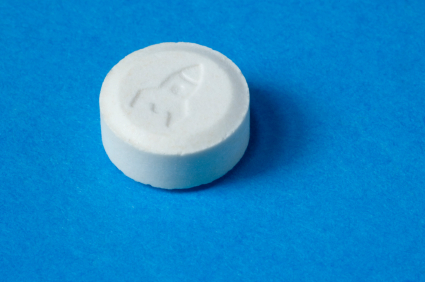
In a 2014 study published by Michael A. Yassa et al. in the journal Nature Neuroscience, a 200mg caffeine pill (about the equivalent of a strong cup of coffee) improved long-term recognition memory. One hundred sixty participants who were not regular coffee drinkers were shown a series of 200 pictures, and 24 hours later they were given a surprise test. Compared to participants who received a placebo, those participants who received 200mg of caffeine were better able to discriminate which pictures they had seen before and which ones were new. Participants who received 100mg of caffeine did not show this effect, while those who received 300mg showed the same improvement in memory but also experienced side effects such as headache and nausea.
As long as a cup of coffee does not make its drinker more anxious, it may help boost memory.
Editor’s Note: Coffee may have other benefits. In research collected by the Bipolar Collaborative Network (in which this editor is an investigator), patients who drank coffee were less likely to be overweight. Yassa also believes based on other research that caffeine is associated with a reduced risk for Alzheimer’s disease and that it increases longevity.
Exercise Helps Mice with Spacial Learning
Exercise increases brain-derived neurotrophic factor (BDNF), a protein that protects neurons and is important for learning and memory. In a study of mice who were trained to find objects, sedentary mice could not discriminate between familiar object locations and novel ones 24 hours after receiving weak training, while mice who had voluntarily taken part in exercise over a 3-week period could easily distinguish between these locations after the weak training.
Mice who received sodium butyrate (NaB) after training behaved similarly well to those who had exercised. Sodium butyrate is a histone deacetylase (HDAC) inhibitor, meaning it helps keep acetyl groups on histones, around which DNA is wrapped, making the DNA easier to transcribe. In this case the easy transcription of DNA enables learning under conditions in which it might not usually take place.
Both sodium butyrate and exercise promote learning through their effects on BDNF in the hippocampus. They make the DNA for BDNF easier to transcribe, suggesting that exercise can put the brain in a state of readiness to create new or more lasting memories.
HDAC Inhibitor Facilitates Extinction of Fear Memories in the Reconsolidation Window
Unwanted recall and re-experiencing of traumatic memories is thought to be a crucial mechanism leading to the onset of post-traumatic stress disorder (PTSD). The inability to diminish (extinguish) those memories contributes to the persistence of PTSD. A new study suggests that the extinction of fear memories can be enhanced by a drug that acts epigenetically to alter the structure of DNA and subsequent gene expression.
DNA is wound around structures called histones, and chemical changes can affect how loosely or tightly the DNA is wound. Johannes Graff et al. reported in the journal Cell in 2014 that application of a histone deacetylase (HDAC) inhibitor, which keeps acetyl groups on histones, ensuring that DNA is wrapped more loosely and is easier to activate (or transcribe), helps rodents revise both new and old fear memories after they have been actively recalled.
When a memory is actively recalled, the trace of that memory in the brain becomes more amenable to revision over the proceeding five minutes to one hour (a period known as the reconsolidation window). New learning and extinction training (to get rid of the memory) lasts much longer when it takes place during the reconsolidation window than when the same procedures are performed 6 hours later (after the reconsolidation window has closed) or if the procedures are performed in the absence of active recall of the memory (when the reconsolidation window is never opened).
We have previously described the 2013 work of Xue et al. published in the journal Science, which showed that this specific procedure could yield long-lasting extinction of a patient’s craving for cocaine or heroin, and could reduce amygdala activation (as observed via functional magnetic resonance imaging) in response to an experiment that produces conditioned fear (Agren et al. Science, 2013).
Editor’s Note: This new work by Graff et al. adds another twist. Older long-term memories are more stable and less amenable to new learning than more recent (but still long-term) memories. The application of an HDAC inhibitor changes this and makes even very old memories amenable to lasting revision. The HDAC inhibitor that Graff et al. used was a specific inhibitor for HDAC type II. However, the anticonvulsant valproate (Depakote) is a potent although nonspecific HDAC inhibitor, and presumably could have the same facilitating effect as the more selective drug.
EMDR (Eye Movement Desensitization and Reprocessing), which has been widely used for the treatment of PTSD, includes active memory recall, immediately followed by an attempt to re-interpret and construct new memories of the trauma. These elements could open the reconsolidation window. However, EMDR works less well with older memories compared to more recent traumatic memories.
The Graff et al. data would suggest that adding an HDAC inhibitor such as valproate to EMDR-like work might make it more effective in revising more remote memories. Graff et al. encourage controlled clinical trials with a type II inhibitor to confirm that their findings in rodents would generalize to humans. While awaiting such validation through controlled clinical trials, it would not be surprising if clinicians started trying out the paradigm on their own using valproate.
BDNF in Learning and Memory
Brain-derived neurotrophic factor (BDNF) is involved in various aspects of learning and memory. The DNA for BDNF contains nine different regulatory sites, each of which is involved in different aspects of learning. Researcher Keri Martinovich studied each site by selectively knocking each one out with a genetic manipulation. She found that blocking the e1 site increased acquisition of new learning and recall in mice, while e2 did the opposite. Blockade of e4 had no effect on these memory functions but markedly blocked the process of extinction, which involves a different kind of new learning.
A mouse that learned to associate a particular cue with a shock (a process known as conditioned fear) will stop reacting to the cue after it is presented many times without a shock. This learning that the cue is no longer associated with the shock is referred to as extinction. The animals with e4 blocked in their BDNF did not develop the new extinction learning, and continued to react to the cue as if it were still associated with the shock.
Editor’s Note: These data may have clinical relevance for humans. The anticonvulsant valproate (trade name Depakote), a histone deacetylase inhibitor, selectively increases the e4 promoter site of BDNF and facilitates extinction of conditioned fear, according to research by Tim Bredy et al. published in 2010.
Clinical trails should examine whether valproate could enhance fear extinction in patients with post-traumatic stress disorder (PTSD).
Fear Memories Can Be Erased or Provoked in Animals
Researchers have identified neurons responsible for remembering conditioned fear in the amygdala of rodents, and can turn them on and off. At the 2013 meeting of the Society of Biological Psychiatry, Sheena A. Josselyn gave a breath-taking presentation on this process.
When animals hear a tone they have learned to associate with the imminent delivery of a shock in a given environment, they learn to avoid that environment, and they reveal their learning of the tone-shock association by freezing in place. Josselyn was able to observe that 20% of the neurons in the lateral nucleus of the amygdala were involved in this memory trace. They were revealed by their ability to increase the transcription factor CREB, which is a marker of cell activation. Using cutting-edge molecular genetic techniques, the researchers could selectively eliminate only these CREB-expressing neurons (using a new technology in which a diphtheria toxin is attached to designer receptors exclusively activated by designer drugs, or DREADDs) and consequently erase the fear memory.
The researchers could also temporarily inhibit the memory, by de-activating the memory trace cells, or induce the memory, so that the animal would freeze in a new context. Josselyn and colleagues were able to identify the memory trace for two different tones in two different populations of amygdala neurons.
The same molecular tricks with memory also worked with cocaine cues, using what is known as a conditioned place preference test. A rodent will show a preference for an environment where it received cocaine. Knocking out the selected neurons would remove the memory of the cocaine experience, erasing the place preference.
The memory for cocaine involved a subset of amygdala neurons that were also involved in the conditioned fear memory trace. Incidentally, Josselyn and her group were eventually able to show that amygdala neurons were in competition with each other as to whether they would be involved in the memory trace for conditioned fear or for the conditioned cocaine place preference.
Citicoline Might Improve Memory
 We’ve written before that the dietary supplement citicoline improved depression in both unipolar and bipolar patients with methamphetamine dependence, reduced cocaine use in bipolar depressed patients with cocaine dependence, and improved cognition in healthy middle-aged women. Findings from a 2013 Italian study by Gareri et al. published in Clinical Interventions in Aging suggests that citicoline improves mild vascular cognitive impairment in older adults, though the study was not randomized, so its results may not be reliable. Citicoline is a natural substance found in the brain and the liver that can also be taken as a nutritional supplement.
We’ve written before that the dietary supplement citicoline improved depression in both unipolar and bipolar patients with methamphetamine dependence, reduced cocaine use in bipolar depressed patients with cocaine dependence, and improved cognition in healthy middle-aged women. Findings from a 2013 Italian study by Gareri et al. published in Clinical Interventions in Aging suggests that citicoline improves mild vascular cognitive impairment in older adults, though the study was not randomized, so its results may not be reliable. Citicoline is a natural substance found in the brain and the liver that can also be taken as a nutritional supplement.
The study examined 349 patients over age 64 (mean age 79.9) who had memory impairment and evidence of vascular lesions in the brain (but not Alzheimer’s disease). Participants who received citicoline (500mg twice daily for 9 months) scored better on a memory examination at 3 months and at the completion of the study, while participants who did not receive citicoline performed worse on the exam. Those who received citicoline also saw some statistically non-significant improvement in mood.
The researchers believe that citicoline’s effects may also extend to Alzheimer’s dementia because citicoline contributes to the synthesis of acetylcholine. (Most Alzheimer’s drugs inhibit the breakdown of acetylcholine).
Side effects were minimal, and included occasional excitability or restlessness, digestive intolerance, and headaches.
Even Short-Term Recreational Use Of Ecstasy Causes Deficits In Visual Memory
German researchers have found that MDMA (ecstasy) users who took more than 10 pills in a one-year period showed deficits in visual memory. Wagner et al. published the study in the journal Addiction in 2012.
In tests where participants were trained to associate certain words with certain images and then recall one in response to the other, those who had taken ecstasy at least ten times the previous year showed deterioration in both their immediate and delayed recall skills.
Given the role of the hippocampus in relational memory, the researchers suspect that there is a relationship between ecstasy use and hippocampal dysfunction.
Editor’s Note: This is the most definitive study on this subject so far because it observed new users before and after they had used ecstasy for at least 10 times in one year (unlike many retrospective studies that observed participants only after they had been using the drug for some time, so it was impossible to know if they had pre-existing memory problems).
Other data in animals and humans suggest that ecstasy burns out the terminals of serotonergic neurons and thus causes brain damage. It now appears this damage to the brain and memory can occur even during short-term or casual ecstasy use.
Psychiatric Revolution: Changes in Behavior Are Associated with Dendritic Spine Shape and Number
New research shows that cocaine, defeat stress, the rapid-acting antidepressant ketamine, and learning and memory can change the size, shape, or number of spines on the dendrites of neurons. Dendrites conduct electrical impulses into the cell body from neighboring neurons.
Cocaine
Several researchers, including Peter Kalivas at the Medical University of South Carolina, have reported that cocaine increases the size of the spines on the dendrites of a certain kind of neurons (GABAergic medium spiny neurons) in the nucleus accumbens (the reward center in the brain). This occurs through a dopamine D1 selective mechanism. N-acetylcysteine, a drug that can be found in health food stores, decreases cocaine intake in animals and humans, and also normalizes the size of dendritic spines.
Depression
Depression in animals and humans is associated with decreases in Rac1, a protein in the dendritic spines on GABA neurons in the nucleus accumbens. Rac1 regulates actin and other molecules that alter the shape of the spines.
In an animal model of depression called defeat stress, rodents are stressed by repeatedly being placed in a larger animal’s territory. Their subsequent behavior mimics clinical depression. This kind of social defeat stress decreases Rac1 and causes spines to become thin and lose some function. Replacing Rac1 returns the spines to a more mature mushroom shape and reverses the depressive behavior of these socially defeated animals. Researcher Scott Russo has also found Rac1 deficits in the nucleus accumbens of depressed patients who committed suicide. Russo suggests that decreases in Rac1 are responsible for the manifestation of social avoidance and other depressive behaviors in the defeat stress animal model, and that finding ways to increase Rac1 in humans would be an important new target for antidepressant drug development.
Another animal model of depression called chronic intermittent stress (in which the animals are exposed to a series of unexpected stressors like sounds or mild shocks) also induces depression-like behavior and makes the dendritic spines thin and stubby. The drug ketamine, which can bring about antidepressant effects in humans in as short a time as 2 hours, rapidly reverses the depressive behavior in animals and converts the spines back to the larger, more mature mushroom-shape they typically have.
Learning and Extinction of Fear
Researcher Wenbiao Gan has reported that fear conditioning can change the number of dendritic spines. When animals hear a tone paired with an electrical shock, they begin to exhibit a fear response to the tone. In layer 5 of the prefrontal cortex, spines are eliminated when conditioned fear develops, and are reformed (near where the eliminated spines were) during extinction training, when animals hear the tones without receiving the shock and learn not to fear the tone. However, in the primary auditory cortex the changes are opposite: new spines are formed with learning, and spines are eliminated with extinction.
Editor’s Note: It appears that we have arrived at a new milestone in psychiatry. In the field of neurology, changes seen in the brains of patients with strokes or Alzheimer’s dementia have been considered “real” because cells were obviously lost or dead. Psychiatry, in comparison, has been considered a soft science because neuronal changes have been more difficult to see and illnesses were and still are called “mental.” Now that new technologies have made a deeper level of precision, observation, and analysis possible, we know that the brain’s 12 billion neurons and 4 times as many glial cells are exquisitely plastic–capable of biochemical and structural changes that can be reversed using appropriate therapeutic maneuvers.
The changes associated with abnormal behaviors, addictions, and even normal processes of learning and memory now have clearly been shown to correspond with the size, shape, and biochemistry of dendritic spines. These subtle, reproducible changes in the brain and body are amenable to therapeutic intervention, and are now even more demanding of sophisticated medical attention.