Midday Bright Light Therapy Improved Bipolar Depression
A study by Dorothy K. Sit and colleagues published in the American Journal of Psychiatry in 2017 found that delivering bright white light therapy to patients with bipolar depression between the hours of noon and 2:30pm improved their depression compared to delivering inactive dim light, and did not cause mood switches into mania. The study included 46 patients with moderate bipolar depression, no hypomania and no psychosis.
The active therapy group was exposed to broad-spectrum bright white fluorescent light at 7,000 Lux while the inactive group received dim red light at 50 Lux. Both groups were instructed to sit 12 inches from the light and face it without looking directly at it. The therapy began with 15-minute afternoon sessions and increased to 60 minutes per day by 4 weeks. Participants were assessed weekly. Remission rates increased dramatically in the active group beginning in the fourth week. At weeks 4 through 6, the remission rate for those in the active bright light group was 68.2% compared to only 22.2% in the dim light group.
Mean depression scores were better in the treated group, as were global functioning and response rates.
Some participants were taking antidepressants concurrently, and these participants were evenly distributed across the two study groups.
An earlier pilot study by the same researchers had found that bright light therapy delivered in the morning was followed by some hypomanic reactions or bipolar cycling. The midday sessions did not cause any mood switching.
Bright light therapy is often used to treat seasonal affective disorder (SAD) using a 10,000 Lux light box. This study took place mostly during the fall and winter months.
Editor’s Note: Bright light therapy is generally safe and boasts a high remission rate. Light boxes can be acquired without a prescription and are portable and easy to use. Midday light may have the best results and the least risk of provoking a mood switch into mania.
Study Suggests Magnesium Could Improve Mild to Moderate Depression as Much as SSRIs
Researcher Emily Tarleton and colleagues report in a 2017 article in the journal PLoS One that over-the-counter magnesium may improve mild to moderate unipolar depression with efficacy similar to that of selective serotonin reuptake inhibitor (SSRI) antidepressants. Magnesium is a mineral that can fight inflammation.
The 126 participants in the open study had an average age of 52. Compared to not taking magnesium, taking 248 mg/day of magnesium produced statistically significant improvement in depression and anxiety symptoms after only two weeks.
The magnesium was well-tolerated by participants. Tarleton and colleagues hope to replicate their findings with a larger and more diverse population.
Making Lithium Treatment More Tolerable For Patients
 In a slideshow at Psychiatric Times, Chris Aiken describes seven ways to improve lithium’s tolerability. Since many researchers, including BNN Editor-in-Chief Robert M. Post, have suggested that lithium should be used more often as a treatment for bipolar disorder, ways of making its side effects more manageable are of great interest. Here we summarize Dr. Aiken’s seven points and add a few perspectives of our own.
In a slideshow at Psychiatric Times, Chris Aiken describes seven ways to improve lithium’s tolerability. Since many researchers, including BNN Editor-in-Chief Robert M. Post, have suggested that lithium should be used more often as a treatment for bipolar disorder, ways of making its side effects more manageable are of great interest. Here we summarize Dr. Aiken’s seven points and add a few perspectives of our own.
Aiken writes that “when it comes to the side effects that matter most to patients—sedation, weight gain, and cognition—lithium’s tolerability ranks right behind lamotrigine.” In fact, lithium plus lamotrigine is an excellent combination, as lithium excels at preventing manias while lamotrigine excels at depression prevention.
Post’s philosophy is that many of lithium’s side effects can be avoided in the first place through judicious dose titration. He suggests gradually increasing dosage, and stopping before side effects become difficult, or reducing a dosage that has already become a problem. The idea is to avoid lithium side effects even if blood levels of lithium remain below clinically therapeutic levels. Post suggests using lithium at whatever dose is not associated with side effects.
Many of lithium’s positive therapeutic effects emerge at low doses, and if this improvement is insufficient, the rest of the needed efficacy can be achieved by adding other medications. As noted above, lamotrigine is a good option for break-through depression, as is lurasidone. For breakthrough mania, the mood stabilizers valproate and carbamazepine or an atypical antipsychotic can be added to lithium.
A little-appreciated option for enhancing lithium’s mood stabilizing effects is nimodipine, a dihydropyridine calcium blocker. It has both antimanic and antidepressant efficacy without lithium’s side effects. Research showed that a year on the combination of lithium and nimodipine was more effective than a year of either drug alone.
If a patient taking lithium experiences a tremor at a dose that is not fully effective, nimodipine can be added in order to lower the lithium dose enough to eliminate the tremor.
Nimodipine specifically blocks the calcium influx gene CACNA1C that has been repeatedly been associated with the vulnerability to bipolar disorder and depression.
If side effects do occur on lithium, they can often be managed. The following suggestions are adapted from Aiken’s article with input from Post. Read more
The New News About Lithium
Robert M. Post, Editor-in-Chief of the BNN, recently published an open access article in the journal Neuropsychopharmacology, “The New News About Lithium: An Underutilized Treatment in the United States.” Here we summarize the main points of the publication, including: the multiple benefits of lithium, its relative safety, predictors of lithium responsiveness, and principles for treatment.
Benefits of lithium
Lithium prevents both depressions and manias in bipolar disorder, and also prevents depressions in unipolar disorder and can augment antidepressant effects acutely. In addition to these mood benefits, lithium has anti-suicide effects. Lithium also enhances the efficacy of atypical antipsychotics and other mood stabilizers when used in combination with them.
Lithium is good for the brain. It has been shown to reduce the incidence of dementia. Lithium increases the volume of the hippocampus and cortex, and can increase the production of new neurons and glia. It also protects neurons. In animals, lithium has been shown to reduce lesion size in neurological syndromes that are models for human disorders such as AIDS-related neurotoxicity, ischemic/hemorrhagic stroke, traumatic brain/spinal cord injury, Huntington’s disease, Alzheimer’s disease, amyotrophic lateral sclerosis (ALS or Lou Gehrig’s disease), fragile X syndrome, Parkinson’s disease, retinal degeneration, multiple sclerosis, alcohol-induced degeneration, Down’s syndrome, spinocerebellar ataxia-1, and irradiation.
Lithium’s benefits include more general ones as well. It can increase the length of telomeres, bits of DNA on the ends of chromosomes that protect them during replication. Short telomeres have been linked to various illnesses and the aging process. Lithium also decreases the incidence of several medical illnesses and enhances survival.
Side Effects Are Often Benign, Treatable
Lithium side effects are more benign than many people think. Even low levels of lithium may be therapeutically sufficient. Read more
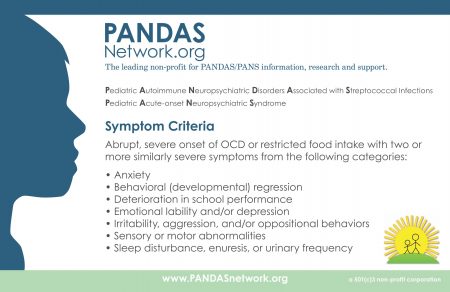
IVIG Produces Long-Term Results in PANDAS
PANDAS, or pediatric autoimmune neuropsychiatric disorder associated with streptococcal infection, is an autoimmune condition that produces psychiatric symptoms that appear suddenly following a case of strep throat in children. These symptoms can include obsessive-compulsive symptoms, tics, and behavioral dyscontrol and regression. Treatments are still experimental, but those that target the immune system are expected to be most successful at improving PANDAS.
In 2015, Miro Kovacevic and colleagues published a case series describing the use of intravenous immunoglobulin treatment (IVIG) in twelve children with PANDAS in the Journal of Child and Adolescent Psychopharmacology. One or in some cases two injections of IVIG brought about long-term remission in the children with PANDAS.
IVIG consists of a wide range of antibodies from multiple individuals delivered via injection. This increase in the quality or quantity of antibodies in the recipient is thought to suppress the production of antibodies that attack brain cells, causing PANDAS. The case series was based on patients at a large clinical practice that specializes in the treatment of PANDAS. The practice used a dosage of 1.5g/kg divided into two daily doses of 750 mg/kg, meant to match twice the volume of the patients’ own immunoglobulin G.
IVIG and other anti-inflammatory approaches are also effective in PANS, a more general variation on PANDAS in which psychiatric symptoms occur following an infection other than strep.
Reduced Functional Connectivity of Amygdala Linked to Autism in Pre-School Boys
A 2016 study in the Journal of the American Academy of Child and Adolescent Psychiatry found that preschool-aged boys with autism have weaker functional connectivity of the amygdala than typically-developing children of the same age. Researchers led by Mark D. Shen used resting-state functional connectivity magnetic resonance imaging (MRI) to measure how connected the amygdala was to other regions of the brain in 72 young boys (average age 3.5).
The boys with autism had weaker connectivity between the amygdala and regions linked to social communication, language deficits, and repetitive behaviors. These areas include the medial prefrontal cortex (mPFC), bilateral temporal lobe, striatum, thalamus, cingulate cortex, and cerebellum.
The weaker the connectivity between these regions, the more severe the boys’ autism symptoms were. They showed impairments in overall cognitive ability and both verbal and nonverbal ability.
Brain Growth in Infancy Predicts Autism
A 2017 article in the journal Nature suggests that brain scans during infancy can predict which kids at risk for autism will go on to develop the disorder, leading to earlier treatment. Studies have shown that children with autism have enlarged brains. The new research zeroes in on the time period when this overgrowth occurs.
Researcher Heather Cody Hazlett and colleagues used magnetic resonance imaging (MRI) scans to measure brain growth in 106 high-risk infants with siblings who have autism spectrum disorder and 42 infants at low risk. The scans were performed when the infants were 6 months, 12 months, and 24 months old.
In 15 infants diagnosed with autism at 24 months, the researchers saw hyperexpansion of cortical surface area between 6 and 12 months and brain overgrowth between 12 and 24 months. The overgrowth coincided with symptoms of autism appearing, and with symptom severity.
The reseachers were able to create a computer algorithm that could predict whether an infant would develop autism based on images of brain growth. The algorithm corrected predicted autism 81% of the time.
Studies have suggested that starting interventions to treat autism early provides the best benefits, so using MRI to diagnose or predict autism before symptoms appear might allow for even earlier treatment that could be more effective.
The study also identified the sites of unusual brain development, which may help researchers determine what mechanisms lead to brain overgrowth in autism and eventually develop treatments that prevent these changes.
Diuretic Looks Promising for Autism
 Phase 2 clinical trials showed that the diuretic bumetanide can reduce the severity of autism spectrum disorders in children aged 3 to 11. A 2017 phase 2B trial assessed side effects and determined the dosage that maximizes benefits and minimizes side effects. Bumetanide will now move on to year-long phase 3 trials in five European countries and may be on the market by late 2021. Bumetanide is an unusually potent ‘loop diuretic’ (a diuretic that works at the loop of Henle in the kidney). In preliminary studies, it has also been used to prevent seizures in newborns.
Phase 2 clinical trials showed that the diuretic bumetanide can reduce the severity of autism spectrum disorders in children aged 3 to 11. A 2017 phase 2B trial assessed side effects and determined the dosage that maximizes benefits and minimizes side effects. Bumetanide will now move on to year-long phase 3 trials in five European countries and may be on the market by late 2021. Bumetanide is an unusually potent ‘loop diuretic’ (a diuretic that works at the loop of Henle in the kidney). In preliminary studies, it has also been used to prevent seizures in newborns.
The phase 2B study included 88 mostly male participants with autism spectrum disorder between the ages of 2 and 18. The participants were randomly assigned to receive 0.5 mg, 1.0 mg, or 2.0 mg twice daily of bumetanide or a placebo for three months.
Bumetanide improved core symptoms of autism such as social communication and restricted interest across all ages. Side effects were worse at higher doses, and included hypokalemia (low potassium), increased urine production, loss of appetite, dehydration, and weakness or lack of energy.
Researchers led by Eric Lemonnier determined that doses of 1.0 mg twice/day produces the most benefits while controlling side effects.
Study of Baby Teeth Links Autism and Exposure to Heavy Metals Such as Lead
Recent research has revealed that autism is linked to new onset genetic mutations (called ‘de novo’ mutations) that occur during early fetal development. A new study suggests that levels of heavy metals such as lead and zinc (but not mercury) may affect the likelihood that these mutations will occur.
The 2017 study by Manish Arora and colleagues in the journal Nature Communications included twins with and without autism, particularly twin pairs in which one twin had autism and the other did not. An international team of scientists collected naturally shed baby teeth from the twins. The researchers then used lasers to extract specific layers of dentine, the hard substance beneath tooth enamel, which correspond to different developmental periods, including before birth and in early childhood. The researchers then analyzed these dentine samples to determine the children’s uptake of various heavy metals in early life.
The analysis showed that children with autism had higher levels of lead (a neurotoxin) throughout development, but particularly right after birth. Children with autism also had lower uptake of manganese, an essential nutrient. Compared to children without autism, children with autism had lower zinc levels in utero, but higher zinc levels after birth. Zinc is another essential nutrient. Lead and manganese levels were also linked to autism severity.
The method of analyzing teeth allows researchers to look back in time and measure what children were exposed to years earlier. This may help identify environmental factors that contribute to autism spectrum disorders.
Autism Linked to Banned Chemicals
 An explanation for the increase in autism rates over the past few decades has remained elusive in the years since researcher Andrew Wakefield fabricated a link between the disorder and mercury in vaccinations that was eventually completely debunked.
An explanation for the increase in autism rates over the past few decades has remained elusive in the years since researcher Andrew Wakefield fabricated a link between the disorder and mercury in vaccinations that was eventually completely debunked.
In 2016, researcher Kristin Lyall of Drexel University’s A.J. Drexel Autism Institute published findings suggesting that high exposure during pregnancy to chemicals banned in the 1970s increased risk of an autism spectrum disorder.
The study looked at 1144 children born in southern California between 200 and 2003. Their mothers had participated in California’s Expanded Alphafetoprotein Prenatal Screening Program, intended to identify birth defects during pregnancy. Second trimester blood samples from these women could be used to determine to what extent their children were exposed to the chemicals while in utero. The researchers found an association between the highest exposure levels and later autism diagnoses.
Lyall and colleagues measured levels of two different classes of organochlorine chemicals: polychlorinated biphenyls (PCBs), used as lubricants, coolants, and insulators; and organochlorine pesticides (OCPs), including DDT, which was banned in 1972. All production of organochlorine chemicals was banned in the US in 1977, but they remain in the environment and are absorbed in the fat of animals that humans eat. According to Lyall, people in the US generally have detectable levels of organochlorine chemicals in their bodies.
The study revealed that exposure to two compounds in particular—PCB 138/158 and PCB 153—was linked to dramatically higher autism rates. Level of exposure is key to autism risk. Those children in the top 25 percentile of exposure were 79% and 82% more likely to have an autism diagnosis than those with the lowest levels of exposure, respectively.
High exposure to two other compounds, PCB 170 and PCB 180, increased autism risk by 50%.
The findings by Lyall and colleagues were published in the journal Environmental Health Perspectives.
Editor’s Note: Another study by Manish Arora and colleagues links autism risk to levels of lead, zinc and manganese absorbed in early life.
The myth that mercury in vaccines causes autism still lingers in our popular culture. Mercury is no longer used in vaccines, but autism rates are still increasing. Perhaps the new findings of a link between heavy metals and autism will help end the misinformation about the safety of vaccines and allow more parents to vaccinate their children without worry.