Amygdala Size Linked to Manic Symptom Severity
 In two posters presented at the 2012 meeting of the American Academy of Child and Adolescent Psychiatry, a research group led by Kiki Chang reported that increased severity of manic symptoms is associated with increased size of the amygdala (especially the right amygdala) in adolescents who are at high risk for developing bipolar disorder.
In two posters presented at the 2012 meeting of the American Academy of Child and Adolescent Psychiatry, a research group led by Kiki Chang reported that increased severity of manic symptoms is associated with increased size of the amygdala (especially the right amygdala) in adolescents who are at high risk for developing bipolar disorder.
The amygdala is a crucial area for emotion regulation. The increasing size, either with more manic symptoms or as patients with bipolar disorder age into adulthood compared to normal volunteer controls (as we describe in the article on brain imaging at far left) could reflect increased use of the amygdala in bipolar disorder.
The increased amygdala size could be linked to increased emotion dysregulation, or it could be a compensatory mechanism in which the amygdala works harder to exert better emotion control.
Experience-dependent neuroplasticity describes a phenomenon in which the volume of a brain area increases as it gets more use (like a muscle that grows when it gets more exercise). One interesting example in which this may occur is London taxi drivers, who have larger hippocampi than the general public. (The hippocampus is responsible for some of the brain’s spatial recognition abilities.) This could be explained in two different ways. The discrepancy in size between the hippocampi of taxi drivers and of the general population may exist because the taxi drivers’ brains change over the course of their careers via experience-dependent neuroplasticity, or it may exist because those with excellent spatial recognition abilities and bigger hippocampi choose to become taxi drivers.
The Unfolding Story of Poor Response to Antidepressants in Bipolar Depression
The role of the traditional antidepressants in the treatment of depression in bipolar illness remains controversial. Despite mounting evidence that they are not efficacious in the treatment of bipolar depression, they are still among the most widely used treatments for that condition. At the first biennial conference of the International Society for Bipolar Disorders held in Istanbul this past March, Mark A. Frye and Shigenobu Kanba chaired a symposium on antidepressant-induced mania and individualized treatment for bipolar depression.
This editor (Robert M. Post) discussed factors influencing antidepressants’ effects on patients with bipolar depression. In a recent meta-analysis, researchers Sidor and MacQueen reviewed data from studies encompassing 2373 patients with bipolar depression and found that antidepressants had no significant benefits over placebo on measures of response or remission. Pooled estimates for a thousand patients showed no increase in patients’ risk of switching into mania after treating with antidepressants. However, in a smaller sub-analysis, the risks of switching into mania following treatment with the older tricyclic antidepressants (43%) and venlafaxine (15%) was greater than the risk of switching after being treated with SSRIs (7%) or bupropion (5%).
There is a conundrum in the literature. While antidepressants don’t work very well in bipolar depression, there is a small subgroup of patients who, having responded well to antidepressants for two months, benefit more from continuing the antidepressant treatment than from discontinuing the drug. Continued treatment with adjunctive antidepressants (added to regular treatment with a mood stabilizer or an atypical antipsychotic) was associated with fewer relapses into depression over the next year when the antidepressants were continued compared to when they were discontinued. Lori Altshuler et al. have published two uncontrolled studies to this effect, Russell Joffe et al. have published one, and a more recent randomized study of this by Nassir Ghaemi replicated some of the results in patients who had non-rapid-cycling bipolar disorder. At the same time, the literature shows that there are number of risk factors for switching into hypomania during antidepressant treatment in bipolar depression.
Risk factors for switching into mania upon treatment with an antidepressant include: younger age, bipolar I compared to bipolar II, rapid cycling in the past year, mixed depression, use of older tricyclic antidepressants compared to newer second-generation antidepressants, use of noradrenergic active antidepressants compared to those that act on serotonin or dopamine, and a history of substance abuse. Read more
Efficacy, Tolerability, and Utility of Treatments for Pediatric Mania
The following table analyzes the information currently available about various treatment options (including treatments NOT yet FDA approved for the treatment of children):
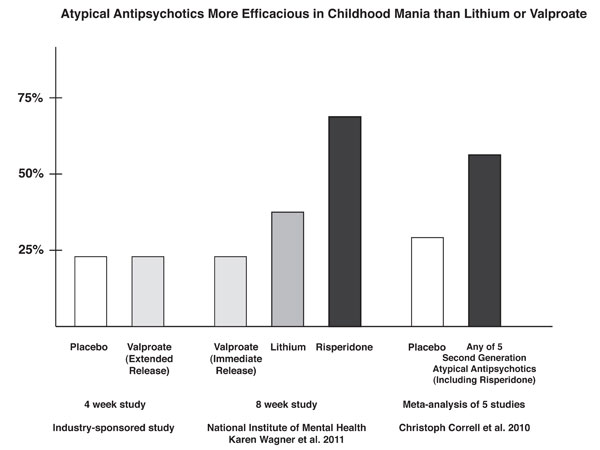
Risperidone Trumps Valproate and Placebo for Treatment of Young Children with Mania
 At another symposium at the annual meeting of the American Academy of Child and Adolescent Psychiatry, Bob Kowatch of Ohio State University discussed a controlled trial of valproate, risperidone, and placebo in children 3 to 7 years of age (average age 5.5) with a diagnosis of bipolar I disorder and a Young Mania Rating Scale score (YMRS) greater than 20 at baseline. All of the children were severely ill with an average Clinical Global Assessment of Severity (CGAS) score of 44. Seventy-six percent had comorbid attention deficit hyperactivity disorder (ADHD) and 15% had an anxiety disorder. Valproate doses started at 10mg/kg and were increased after 4 days to achieve blood levels of 80 to 100µg/ml. The average dose of valproate was 300mg/day and the average blood level was 88 µg/ml. Risperidone was started at 0.25mg and increased as needed. The average dose of risperidone was 0.5mg per day.
At another symposium at the annual meeting of the American Academy of Child and Adolescent Psychiatry, Bob Kowatch of Ohio State University discussed a controlled trial of valproate, risperidone, and placebo in children 3 to 7 years of age (average age 5.5) with a diagnosis of bipolar I disorder and a Young Mania Rating Scale score (YMRS) greater than 20 at baseline. All of the children were severely ill with an average Clinical Global Assessment of Severity (CGAS) score of 44. Seventy-six percent had comorbid attention deficit hyperactivity disorder (ADHD) and 15% had an anxiety disorder. Valproate doses started at 10mg/kg and were increased after 4 days to achieve blood levels of 80 to 100µg/ml. The average dose of valproate was 300mg/day and the average blood level was 88 µg/ml. Risperidone was started at 0.25mg and increased as needed. The average dose of risperidone was 0.5mg per day.
On the main outcome measure of decrease in the YMRS score risperidone was substantially more effective than placebo, while valproate showed only marginal nonsignificant effects. However on the Clinical Global Impressions (CGI) scale for improvement in illness, risperidone showed 87% response, valproate 75% response, and placebo no response. In terms of 50% reduction in the YMRS score, this endpoint was achieved in 88% on risperidone, 50% valproate, and 15% on placebo.
Weight gain was mild on valproate and substantially more on risperidone. Risperidone was also associated with increases in insulin and prolactin.
The effect size (the size of the change the drug brought about in this study, which is calculated by dividing the mean difference between the experimental group and the control group by the standard deviation) for risperidone was extraordinarily large (3.58); very large for valproate (1.66), and moderate for placebo (0.56). The odds of getting well were 5 times greater than placebo for risperidone and 1.9 times greater than placebo for valproate.
Editors note: These data in very young children (aged 3 to 7) resemble other controlled data in the literature about the treatment of older children and adolescents, indicating a superiority of atypical antipsychotics over placebo and a greater magnitude of effect achieved with atypicals than with valproate. Based on these new data and the Federal Drug Administration (FDA) approval of several atypical antipsychotics for children with bipolar illness from ages 10 to 17, Dr. Kowatch recommended a new treatment algorithm for childhood onset bipolar disorder. Read more
News From The “TEAM” Study: Risperidone Superior To Valproate And Lithium In Childhood Mania
A symposium at the Annual Meeting of the American Association of Child and Adolescent Psychiatry discussed the Treatment of Early Age Mania (TEAM) study, which comprised 5 different sites in Pittsburgh, Washington DC, Baltimore, St. Louis, and Cleveland. This randomized partially blinded study compared risperidone, valproate, and lithium for the treatment of children with bipolar I mania.
Participants were all severely ill with a Clinical Global Assessment of Severity score (C-GAS) of less than 60 (the mean was 39, indicating that the children were substantially impaired). More than three quarters had psychosis (i.e. hallucinations or delusions) and 99% had dramatic mood shifts within a day (ultradian cycling). All the children had the cardinal symptom of elevated mood.
Among the 290 participants, there was a high incidence of Axis I comorbidities, with 98% of patients having a disruptive behavioral disorder, 77.3% an anxiety disorder, 31% some form of sleep disturbance, and 17% an elimination disorder, of which 15% had enuresis (bedwetting). Nightmares were present in 25.9% of the sample, sleepwalking in 7.2%, and night terrors in 4.8%.
For the purposes of the study, response was considered to have been achieved when a child received a rating of 1 (not ill) or 2 (minimally ill) on the Clinical Global Impressions scale modified for bipolar illness (CGI-BP).
The children (age 6 to 15 with a mean age of 11) were randomized to treatment for 8 weeks with lithium, valproate, or risperidone. Lithium treatment reached blood levels of 1.1 to 1.3mEq/L, valproate reached levels of 111 – 225µg/ML, and risperidone doses were up to 3mg per day. Children who were taking psychomotor stimulants for treatment of ADHD remained on the stimulants after randomization to one of the three drugs. While the treating physicians and clinicians were not blind, blind ratings were performed at week 8.
With a response rate of 68.5%, risperidone was superior to lithium (35.6%) and valproate (24%) based on CGI-BP scores. The mean dose of risperidone was 2.6mg +/- 1.2 per day. The mean blood level at week 8 for lithium was 1.1mEq/L and for valproate was 114µg/ML.
The number of children who improved sufficiently for their C-GAS scores to rise above 60 was also greater for risperidone at 48.3% compared to lithium at 26.7% and valproate at 17.0%. Read more
New Drug Cariprazine May Be Effective in Acute Mania
 Medscape Medical News reported that a new antipsychotic, cariprazine, may be effective in treating acute mania in bipolar I disorder. The drug is produced by Forest Laboratories Inc. and Gedeon Richter Plc.
Medscape Medical News reported that a new antipsychotic, cariprazine, may be effective in treating acute mania in bipolar I disorder. The drug is produced by Forest Laboratories Inc. and Gedeon Richter Plc.
The data showed that patients with acute manic episodes who were treated with cariprazine experienced significant improvements in symptoms compared with patients given placebo, as measured by the Young Mania Rating Scale (YMRS). These improvements, report the companies, were observed as early as day 5 of treatment and at each subsequent time point in the study.
The multicenter, double-blind placebo-controlled parallel group study showed statistically significant improvement in patients receiving cariprazine in each of 2 dosages — 3 to 6 mg/day (-6.1 points, P < 0.001) and 6 to 12 mg/day (-5.9 points, P < 0.001) — as compared with patients receiving placebo.
See here for a history of the research on cariprazine.
Aripiprazole Makes Lamotrigine More Effective
 In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
Editor’s note: These data add to a growing literature that shows that an atypical antipsychotic added to a mood stabilizer is associated with better prophylactic effects than use of the mood stabilizer alone. Previously, most of the studies of this type of combination used lithium or valproate as the mood stabilizer and, to our knowledge, this is the first to demonstrate that long-term prevention with lamotrigine is enhanced by the addition of an atypical antipsychotic.
Many of the atypical antipsychotics are FDA-approved as adjunctive treatments to mood stabilizers in the long-term treatment of bipolar disorder. The controlled clinical trial data that led to this FDA approval support the practice of many clinicians who prescribe combination treatment rather than monotherapy in order to achieve a more rapid onset of anti-manic stabilization and longer-term maintenance effects. The use of aripiprazole and quetiapine as adjuncts to lithium and valproate is particularly common in bipolar disorder since the same atypical antipsychotics are FDA-approved as adjunctive treatments in unipolar depression, and clinicians are familiar with prescribing them to improve ineffective acute antidepressant treatment.
Quetiapine (Seroquel) May Be Effective in Childhood Mania
 Gagan Joshi performed an 8-week open study of quetiapine in 30 preschool children and 19 school-age children. The mean dose was 176 mg/day on average for the preschool children, and 248 mg/day for the school age children, and both appeared highly effective in treating manic symptomatology. At the 57th Annual Meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in October 2010, Joshi reported that while the drug was generally well tolerated, it was associated with significant weight gain; the preschoolers gained 3.1 lbs on average in the 8-week period, while the school age children gained an average of 7.4 lbs.
Gagan Joshi performed an 8-week open study of quetiapine in 30 preschool children and 19 school-age children. The mean dose was 176 mg/day on average for the preschool children, and 248 mg/day for the school age children, and both appeared highly effective in treating manic symptomatology. At the 57th Annual Meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in October 2010, Joshi reported that while the drug was generally well tolerated, it was associated with significant weight gain; the preschoolers gained 3.1 lbs on average in the 8-week period, while the school age children gained an average of 7.4 lbs.
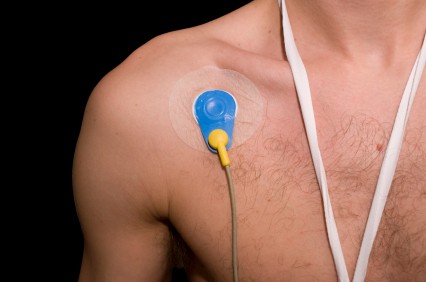
Ziprasidone Does Not Seem to Cause Arrhythmias, As Once Feared
A comprehensive review of ziprasidone’s effect on the QTc interval, a measure of electrical activity in the heart, has been completed by John Kane of the Zucker Hillside Hospital in Glen Oaks, NY. He and his colleagues reviewed relevant data that had been published over the past decade. Ziprasidone can prolong the QTc interval, which theoretically puts a person at risk for cardiac arrhythmias. Kane and colleagues concluded that the effect of ziprasidone on the QTc interval is related to dose and to the patient’s baseline QTc interval.
The QTc prolongation appears to plateau at the higher end of the usual clinical dose range of ziprasidone. In their review, the researchers found no cases of a QTc interval greater than 480 milliseconds, which is thought to be the threshold for developing vulnerability to arrhythmias. Additionally, no deaths were attributed to ziprasidone in any of the studies reviewed.
Ziprasidone side effects differ in different mood states
Keming Gao from Case-Western Reserve University reviewed the adverse effects of ziprasidone monotherapy in the treatment of patients with bipolar depression, mania, or schizophrenia. Gao noted that akathisia (restless legs) and other extrapyramidal side effects (such as tremor or speech problems) during mania were more common among patients on ziprasidone than among those on placebo, and these effects were more often found in patients with mania than those with depression.
Editor’s note: The finding that these extrapyramidal side effects are more common during mania is interesting because it runs contrary to findings on another atypical antipsychotic, aripiprazole. Aripiprazole is a partial dopamine agonist, meaning it partially activates dopamine receptors, and bipolar depressed patients on aripiprazole experience more akathisia than patients taking aripiprazole for mania or schizophrenia do.
Ziprasidone fully blocks dopamine receptors, and this may explain why its effects on dopamine turnover may, in contrast to aripiprazole, convey greater risk for extrapyramidal side effects in mania than in depression. This is unusual since most side effects tend to be more prominent during the depressive phases than manic phases of the illness. The reasons for this reversal with ziprasidone deserve further investigation and clarification.
Brain Volume Reduced As Early As First Episode Of Mania
 Researchers Manpreet K. Singh and Kiki D. Chang et al. from Stanford reported at the 65th Annual Scientific Convention of the Society of Biological Psychiatry that adolescents experiencing a first episode of mania show reduced volume in the subgenual anterior cingulate cortex (Brodmann area 25). Previous studies have indicated that teens and adults with bipolar disorder exhibit decreased volume in prefrontal gray matter. Read more
Researchers Manpreet K. Singh and Kiki D. Chang et al. from Stanford reported at the 65th Annual Scientific Convention of the Society of Biological Psychiatry that adolescents experiencing a first episode of mania show reduced volume in the subgenual anterior cingulate cortex (Brodmann area 25). Previous studies have indicated that teens and adults with bipolar disorder exhibit decreased volume in prefrontal gray matter. Read more