Heading Off Early Symptoms of Bipolar Disorder in Children at High Risk
 At the American Academy of Child and Adolescent Psychiatry (AACAP) annual meeting in Toronto in October 2011, there was a symposium on risk and resilience factors in the onset of bipolar disorder in children who have a parent with the disorder.
At the American Academy of Child and Adolescent Psychiatry (AACAP) annual meeting in Toronto in October 2011, there was a symposium on risk and resilience factors in the onset of bipolar disorder in children who have a parent with the disorder.
Family Focused Therapy Highly Encouraged
Amy Garrett reported that family focused therapy (FFT) in those at risk for bipolar disorder was effective in ameliorating symptomatology compared to treatment as usual. Family focused therapy, pioneered by Dave Miklowitz, PhD of UCLA involves three components. The first component is education about the illness and methods of self-management. The second is enhancement of communication in the family with practice and rehearsal of new modes of conversation. The third component is assistance with problem solving.
In Garrett’s study, 50 children aged 7 to 17 were randomized to family focused treatment or treatment as usual. These children were not only at high risk for bipolar disorder, they were already prodromal, meaning they were already diagnosable with bipolar not otherwise specified (BP-NOS), cyclothymia, or major depressive disorder, and had also shown concurrent depressive and/or manic symptoms in the two weeks prior to the study. At baseline, compared to controls, these children at high risk for full-blown bipolar disorder by virtue of a parental history of the illness showed increased activation of the amygdala and decreased activation of the prefrontal cortex. Most interestingly, after improvement with the family focused therapy (FFT), amygdala reactivity to emotional faces became less prominent and dorsolateral prefrontal cortical activity increased in proportion to the degree of the patient’s improvement.
The discussant for the symposium was Kiki Chang of Stanford University, who indicated that the results of this study of family focused therapy were already sufficient to convince him that FFT was a useful therapeutic procedure in children at high risk for bipolar disorder by virtue of having a parent with a history of bipolar illness. Chang is now employing the therapy routinely in all of his high-risk patients.
Editors Note: This is an extremely important recommendation as it gives families a specific therapeutic process in which to engage children and others in the family when affective behavior begins to become abnormal, even if it does not meet full criteria for a bipolar I or bipolar II disorder.
FFT also meets all the important criteria needed for putting it into widespread clinical practice. Family focused therapy has repeatedly been shown to be effective in adults and adolescents with bipolar illness and now also in these children who are prodromal. The psychoeducational part of FFT is common sense, and dealing with communication difficulties and assisting with problem solving also have merit in terms of stress reduction. Finally, this treatment intervention appears to be not only safe but also highly effective in a variety of different prodromal presentations of affect disorders even if children do not meet full criteria for bipolar disorder. While the few studies of early intervention with psychopharmacological agents have not yet identified efficacious medications for the prodromes of bipolar disorder and in particular medications with a high degree of safety, such family focused therapy appears to be an ideal early intervention.
I would concur with Dr. Chang’s assessment. Family focused therapy (FFT) should be offered to all children with this high-risk status who have begun to be symptomatic. Early onset of unipolar depressive disorder or of bipolar disorder carries a more adverse prognosis than the adult onset variety and thus should not be ignored. If more serious illness is headed off early, it even raises the possibility that the full-blown illness will not develop at all.
Gray Matter Volume Abnormalities
Tomas Hajek of Dalhousie University in Halifax presented data indicating that in children at high risk for bipolar disorder, gray matter volume in the right inferior frontal gyrus is increased. Read more
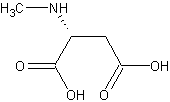
Rare Encephalitis Affects NMDA Receptor
At the 57th Annual Meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in October 2010, Nadine Schwartz reported that in a rare type of encephalitis, antibodies specifically target and bind to N-methyl-D-aspartate (NMDA) receptors, the major receptors for excitatory neurotransmission in the brain. Individuals usually develop psychiatric symptoms before neurological ones, and were previously often thought to be malingering or inventing their illness. Eventually they may develop profound cognitive and motor deterioration and many may require treatment in an intensive care unit in order to provide adequate respiration. Studies show that children with this syndrome appear to respond to anti-immune therapeutic approaches including steroids, plasmaphoresis, and antimetabolites.
Editor’s Note: The recognition that auto-antibodies can attack the major receptors for excitatory neurotransmission in brain brings to light another potential mechanism that could explain neurochemical dysregulation in the neuropsychiatric disorders.
Dopamine D2 and D3 Agonist Pramipexole May Enhance Cognitive Function in Bipolar I Disorder
Anil Malhotra from the Zucker Hillside Hospital found that pramipexole (Mirapex), a dopamine D2 and D3 agonist used in the treatment of Parkinson’s disease, improved measures of processing speed and working memory in euthymic bipolar patients (whose average age was 42) when compared with placebo in an adjunctive clinical trial.
Editor’s Note: Bipolar patients in a euthymic phase have consistently been shown to have some degree of cognitive dysfunction that is typically correlated with the number of prior depressive and/or manic episodes they have experienced. This is one of the first studies to directly target this cognitive dysfunction with a pharmacotherapeutic agent.
Pramipexole may be of additional value among depressed patients, because in two small, placebo-controlled studies, one led by Carlos Zarate at the National Institute of Mental Health and one led by Joseph F. Goldberg in New York, pramipexole has been shown to exert acute antidepressant effects in bipolar patients in the depressive phase of the illness. The new data from Malhotra raise the possibility that there could be a two-for-one benefit when pramipexole is used in the depressive phase of bipolar illness—improvement in both depression and cognition.
Other approaches to improving cognition in patients with bipolar disorder
Inflammation and Oxidative Stress in Bipolar Disorder
A number of studies presented at the 4th Biennial Conference of the International Society for Bipolar Disorders conference in Sao Paulo, Brazil in March reported new data relevant to inflammation and oxidative stress. Both inflammation and oxidative stress increase risk of cardiovascular disorders, and patients with inadequately treated mood disorders lose 10 or more years of life expectancy from cardiovascular disorders compared to the general population. Inflammation and oxidative stress may also contribute to the symptoms, evolution, and progression of the mood disorders themselves.
It is possible that these two processes could become new targets for therapeutic intervention in addition to more traditional psychopharmacological drugs that primarily target the neurotransmitters dopamine, norepinephrine, serotonin, and the neurotrophic factor BDNF. Read more