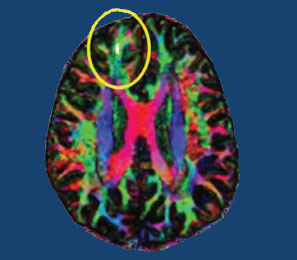
Poverty Early in Life Decreases White Matter Integrity in the Brain
One-fifth of children in America grow up in poor families. Poverty can affect development, health, and achievement, and new evidence shows it even affects brain structure.
New unpublished research suggests that early poverty can affect the brain’s structure into adulthood. At a 2015 scientific meeting, researcher James Swain reported that socio-economic status at age 9 was associated with the integrity of white matter in several regions of the brain, including the hippocampus, parahippocampal gyrus, dorsolateral prefrontal cortex, ventrolateral prefrontal cortex, corpus collosum, and thalamus at age 23–25, regardless of income at that time.
The brain regions affected by childhood poverty support executive function (planning and implementation skills), social cognition, memory, and language processing. White matter provides the physical connections between parts of the brain, so damage to white matter may lead to problems with functional connectivity of the brain.
Brain Inflammation in People at High Risk for Schizophrenia
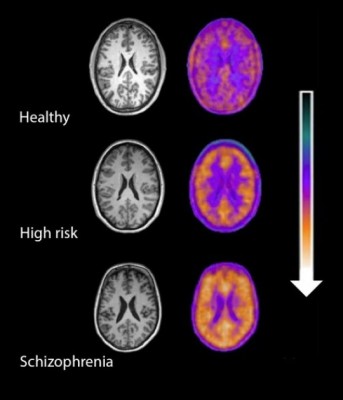
Microglial activity in the brains of people who are healthy, people at high risk for schizophrenia, and people who have been diagnosed with schizophrenia.
A 2016 study by Peter S. Bloomfield and colleagues in the American Journal of Psychiatry used PET scans to compare the activity of microglia, immune cells in the central nervous system, in healthy controls, people with schizophrenia, and those at high risk for the illness. It found that both people with schizophrenia and those at high risk had greater brain inflammation than the healthy controls.
The study was the first to show that microglial activity was elevated in people at high risk (who showed some preliminary symptoms of schizophrenia). The finding had a large effect size.
Microglial activity was also correlated with symptom severity in the high-risk participants. Increased microglial activity was not linked to depression, suggesting that it is specific to the development of psychosis.
These findings resemble those of other recent studies showing increased inflammation in people at high risk for psychosis.
The study suggests that increased microglial activity occurs before a first episode of psychosis. That means it could help identify people who may develop schizophrenia. The findings also suggest that anti-inflammatory treatment could theoretically be used to prevent psychosis.
RTMS for Depression Increases Volume of Specific Brain Regions
Repeated transcranial magnetic stimulation (rTMS) is a treatment for depression in which magnets placed near the skull stimulate electrical impulses in the brain. In a poster presented at the 2015 meeting of the Society of Biological Psychiatry, Martin Lan and colleagues presented results of the first study of structural changes in the brain following rTMS.
In the study, 27 patients in an episode of major depression underwent magnetic resonance brain scans before and after receiving rTMS treatment over their left prefrontal cortices. Lan and colleagues reported that several cortical regions related to cognitive appraisal, the subjective experience of emotion, and self-referential processing increased in volume following rTMS treatment: the anterior cingulate, the cingulate body, the precuneous, right insula, and gray matter in the medial frontal gyrus. The increases ranged from 5.3% to 15.7%, and no regions decreased in volume. More than 92% of the participants showed increased gray matter in all of these regions.
The brain changes were not correlated with antidepressant response to rTMS, but suggest a possible mechanism by which rTMS is effective in some people. Lan and colleagues concluded that rTMS likely had neuroplastic effects in areas of the brain that are important for emotion regulation.
Blood and Now Brain Inflammation Linked to Depression
 There is growing evidence of a link between inflammation of depression. At the 2015 meeting of the Society of Biological Psychiatry, researcher Jeff Meyer summarized past studies on inflammatory markers. These are measurements, for example of certain proteins in the blood, that indicate the presence of inflammation in the body.
There is growing evidence of a link between inflammation of depression. At the 2015 meeting of the Society of Biological Psychiatry, researcher Jeff Meyer summarized past studies on inflammatory markers. These are measurements, for example of certain proteins in the blood, that indicate the presence of inflammation in the body.
Common inflammatory markers that have been linked to depression include IL-6, TNF-alpha, and c-reactive protein. At the meeting, Meyer reviewed the findings on each of these. Twelve studies showed that IL-6 levels are elevated in the blood of patients with depression. Four studies had non-significant results of link between IL-6 and depression, and Meyer found no studies indicating that IL-6 levels were lower in those with depression. Similarly, for TNF-alpha, Meyer found 11 studies linking elevated TNF-alpha with depression, four with non-significant results, and none showing a negative relationship between TNF-alpha and depression. For c-reactive protein, six studies showed that c-reactive protein was elevated in people with depression, six had non-significant results, and none indicated that c-reactive protein was lower in depressed patients.
Most studies that have linked inflammation to depression have done so by measuring inflammatory markers in the blood. It is more difficult to measure inflammation in the brain of living people, but Meyer has taken advantage of new developments in positron emission tomography (PET) scans to measure translocator protein binding, which illustrates when microglia are activated. Microglial activation is a sign of inflammation. Translocator protein binding was elevated by about 30% in the prefrontal cortex, anterior cingulate cortex, and insula in study participants who showed symptoms of a major depressive episode compared to healthy control participants. The implication is that the depressed people with elevated translocator protein binding have more brain inflammation, probably via microglial activation.
The antibiotic minocycline reduces microglial activation. It would be interesting to see if minocycline might have antidepressant effects in people with depression symptoms and elevated translocator protein binding.
Neuropsychological Deficits After Concussion Are Correlated with White Matter Abnormalities
Many people suffer problems with mental functioning after an apparent concussion (otherwise known as mild traumatic brain injury, or mTBI) that does not show abnormalities on traditional brain imaging measures such as the MRI. New technology called diffusion tensor imaging (DTI) shows that the integrity of white matter tracts may be disturbed by concussions. White matter comprises parts of the brain where myelin wraps around axons, as opposed to grey matter, which reflects the presence of neuronal cell bodies.
In a longitudinal study published in the Journal of Neurotrauma, Vigneswaran Veeramuthu and colleagues compared 61 people with an mTBI to 19 healthy controls. The mTBI participants had their neuropsychological faculties assessed an average of 4.35 hours after their trauma, and participated in DTI scans an average of 10 hours after the trauma. Both the neuropsychological assessment and the DTI scan were repeated six months later. When the acute and follow-up assessments were compared to the same assessments in control participants, the two groups showed differences in numerous white matter tracts at the six-month mark. There was also an association between the degree of abnormality observed on the DTI scans and decrements in performance on the tests of neuropsychological functioning both immediately after the trauma and six months later.
The researchers concluded that their results “provide new evidence for the use of DTI as an imaging biomarker and indicator of [white matter] damage occurring in the context of mTBI, and [the results] underscore the dynamic nature of brain injury and possible biological basis of chronic neurocognitive alterations.”
Editor’s Note: People should be aware of these findings, which confirm earlier studies, and begin rehabilitative treatment as soon as possible after a concussion. New research should target white matter tract changes, with the goal of secondary prevention, i.e. limiting damage to the brain after a traumatic injury has occurred. There are several promising drugs that can prevent damage if administered immediately after an mTBI, including the antioxidant supplement N-acetylcysteine (NAC), which has shown promise in preliminary clinical and laboratory studies, and many others, including lithium and valproate, as reported by De-Maw Chuang and this editor Robert M. Post in a 2015 article in the Journal of Neurology and Stroke titled “Preventing the Sequelae of Concussions and Traumatic Brain Injury.”
Brain Activity Differentiates Youth with Bipolar Disorder from Youth with Unipolar Depression
Both bipolar disorder and unipolar depression often begin in childhood or adolescence, but it can be difficult to distinguish the two using symptoms only. People with bipolar illness may go a decade without receiving a correct diagnosis. Researcher Jorge Almeida and colleagues recently performed a meta-analysis of previous studies to determine what neural activity is typical of children with bipolar disorder versus children with unipolar depression while processing images of facial emotion. They found that youth with bipolar disorder were more likely to show limbic hyperactivity and cortical hypoactivity during emotional face processing than youth with unipolar depression. Almeida and colleagues hope that this type of data may eventually be used to diagnose these disorders or to measure whether treatment has been successful.
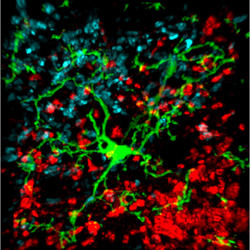
Lighting Up Neural Networks in Mice
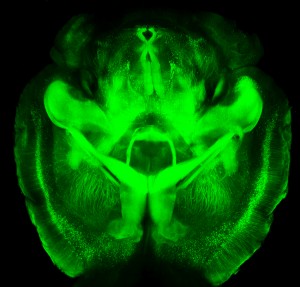 A new technology is making it possible to view the mammalian brain’s structure and connectivity for the first time. Karl Deisseroth discussed the technology, called CLARITY, at a plenary lecture at the 2014 meeting of the International College of Neuropsychopharmacology.
A new technology is making it possible to view the mammalian brain’s structure and connectivity for the first time. Karl Deisseroth discussed the technology, called CLARITY, at a plenary lecture at the 2014 meeting of the International College of Neuropsychopharmacology.
The way CLARITY works is by replacing lipids in the brain with a hydrogel substance. This preserves the structure of the brain’s neural networks, leaves proteins and nucleic acids intact, but allows for observation by rendering the brain transparent. This can be done in a system as large as the entire adult mouse brain. Early attempts took a whole day, but Deisseroth eventually found a way to render a mouse’s brain transparent in a matter of minutes.
The pictures are truly amazing, allowing for the visualization of previously microscropic neurons, dendrites, axons and connections in life-sized images. Pictures and details are available at www.clarityresourcecenter.org.
Deisseroth and colleagues have used CLARITY imaging to determine where neurons fire during different social activities. By placing photosensitive fibers in selected neurons using a virally based gene insertion technique, Deisseroth and colleagues were able to selectively fire dopamine neurons in the ventral tegmental area, part of the brain’s reward system, and thus increase or decrease the social interaction of mice by increasing or decreasing firing. The effects were selective to social interaction; the firing did not affect locomotor activity or exploration of an inanimate object.
The ventral tegmental area contains neurons that project to several locations in the brain, and Deisseroth and colleagues hoped to observe which were important to social interaction. Stimulating the ventral tegmental area to drive the medial prefrontal cortex caused anxiety in the mice and made them averse to social interaction. However, when the ventral tegmental area was used to selectively drive the nucleus accumbens, another part of the brain’s reward system, social interaction increased.
Deisseroth wanted to know if the nucleus accumbens was also involved in normal spontaneous social interactions. The researchers used a virus to insert an opsin-sensitive calcium gene that could give an ongoing readout of neural activity. (Opsin is a light-sensitive receptor found in cells in the retina.) The team found that the nucleus accumbens was implicated in social interaction with another mouse, but not in exploration of a novel object. Based on CLARITY imaging of the structure of ion channels (which are so small they cannot even be seen with an electron microscope), Deisseroth was able to selectively alter ion fluxes and turn neuronal firing on or off at will.
In the last 50 years, the brain and its billions of neurons and hundreds of trillions of synapses have gone from complete inaccessibility toward increasing clarity.
Learning to Change Brain Activity to Decrease Cocaine Craving
Colleen Hanlon, a researcher at the Medical University of South Carolina, has found that biofeedback can be used to decrease cocaine craving in people with substance abuse problems. In her research, patients were given real time feedback from functional magnetic resonance imaging (fMRI) and learned to decrease the activation of a part of the brain called the anterior cingulate when exposed to cocaine cues (reminders of their desire for cocaine). They were able to decrease drug craving as well as heart rate and skin conduction, which often accompany it.
Ecstasy Use Increases Serotonin Receptors in Women
MDMA, better known as the drug ecstasy, has been found to reduce serotonin axons in animals. A small study by Di Iorio et al. published in the Archives of General Psychiatry in 2012 suggests that the drug also has detrimental effects on serotonin signaling in humans.
The researchers used positron emission tomography (PET) scans to identify serotonin receptors in the brains of 10 women who had never used ecstasy and 14 who had used the drug at least five times before and then abstained for at least 90 days. The team found significantly greater cortical serotonin2A receptor nondisplaceable binding potential (serotonin2ABPND, an indicator of serotonin receptors) in abstaining MDMA users than in those women who had never used the drug.
The increase in serotonin receptors observed in these ecstasy users could be a sign of chronic serotonin neurotoxicity. Loss of serotonin nerve terminals decreases serotonin levels and secondarily results in the production of more serotonin receptors. Thus, one explanation for the receptor increase is that it is prompted by the decrease in serotonin transmission that MDMA is known to cause.
The higher levels of serotonin2ABPND were found in several regions of the MDMA users’ brains: occipital-parietal, temporal, occipito-temporal-parietal, frontal, and frontoparietal. Lifetime use of the drug was associated with serotonin2ABPND in the frontoparietal, occipitotemporal, frontolimbic, and frontal regions. There were no regions in which the MDMA users had lower levels of receptors than women in the control group. The duration of the ecstasy users’ abstinence from using the drug had no effect on levels of serotonin2ABPND observed, suggesting that the effects might be long-lasting, if not permanent.
Editor’s Note: Given serotonin’s importance in brain function and the drug’s popularity for recreational use, this finding has implications both for ecstasy users and for research on serotonin signaling. Ecstasy is supposed to be a “love drug,” but people should show their serotonin nerve terminals some love and look after them by avoiding the drug.
Meditation Improves Mood and White Matter Integrity
New research shows that regular meditation in the form of mindfulness training improves both mood and measures of white matter (axon tract) integrity and plasticity in the anterior cingulate cortex (a key node in the brain network modulating self-regulation).
This research by Tang et al. published in the Proceedings of the National Academy of Sciences in 2012 was a continuation of the same research group’s investigation of integrative mind-body training (IMBT), a type of mindfulness training that incorporates increased awareness of body, breathing, and attention to external instructions meant to induce a state of balanced relaxation and focused attention. In a previous Tang et al. study comparing participants who received IMBT training with a control group who spent the same amount of time doing relaxation training, the participants who practiced IMBT for five days (20 minutes/day) had better scores on measures of attention, anxiety, depression, anger, fatigue, and energy. In another study the researchers found that four weeks of IMBT (30 minutes/day) increased fractional anisotrophy (FA) in white matter areas involving the anterior cingulate cortex, while four weeks of relaxation training did not bring about any effect on white matter. Decrease in FA is a part of aging. The four weeks of IMBT also decreased axial and radial diffusivity, suggesting better alignment of axons along white matter tracts.
In the most recent study, two weeks of IMBT (30 minutes/day) produced a reduction in axial diffusivity, but not effects on fractional anisotrophy or radial diffusivity, suggesting that the reduced axial diffusivity leads to the other changes seen with longer IMBT.
Editor’s Note: In those with unresolved problems with anxiety and depression, regular 20-30 minutes/day mindfulness practice may have beneficial effects not only on mood, but also on central nervous system structures. Mindfulness training involves focused attention on sequentially different parts of the body leading to exclusive focus on the physical aspects of breathing in and out. Intruding thoughts are recognized, but let go as trivial, passing interruptions, and focus is returned to the body and breathing. The aim is to clear the mind of its usual ideas, thoughts, and worries by continually refocusing on breathing. It takes practice to achieve, but regular mindfulness training can be a helpful addition to pharmaco- and psychotherapy.
It is also noteworthy that mindfulness training is one of the processes that helps elongate the ends of each strand of DNA, called telomeres. Telomeres shorten with aging, stress, and episodes of depression, and short telomeres lead to a variety of adverse medical consequences.