Antioxidant NAC Improves Symptoms of Schizophrenia and Bipolar Disorder
N-acetylcysteine (NAC), an antioxidant available without a prescription in health food stores, has shown remarkable effectiveness when added to regular treatments for schizophrenia, bipolar disorder, and the substance abuse that often accompanies these illnesses.
A 2008 article by Michael Berk and colleagues in the journal Biological Psychiatry reported that compared to placebo, 2 grams/day of NAC reduced both positive symptoms of schizophrenia (hallucinations, delusions) and negative symptoms (social withdrawal, difficulty planning and problem-solving). A 2013 study by Mehdi Farokhnia found that 2 grams/day of NAC improved negative symptoms in 42 patients with schizophrenia. Two other studies found that NAC improved deficits in auditory sensory processing in people with schizophrenia.
NAC also improves symptoms of bipolar disorder. A 2008 study by Berk and a 2011 study by Pedro Vieira da Silva Magalhães showed that NAC improved bipolar depression, and a small 2013 study by Magalhães showed that it improved mania in 15 patients. After 24 weeks, 60% of those who took NAC were in remission, compared to 15% of those taking placebo.
NAC is also effective at reducing habitual behaviors such as substance abuse, which is common in patients with schizophrenia and bipolar disorder. Studies have shown that NAC can reduce patients’ use of marijuana, cocaine, alcohol, and nicotine. It is relatively safe with minimal side effects, and fights oxidative stress, which is also common in severe mental illness.
NAC comes in 500mg or 600mg capsules. Dosing typically begins with one capsule twice a day for a week, followed by two tablets twice a day thereafter. As with any recommendations in the BNN, these should not be acted on without guidance from a treating physician.
Schizophrenia: The Importance of Catching It Early
By the time psychosis appears in someone with schizophrenia, biological changes associated with the illness may have already been present for years. A 2015 article by R.S. Kahn and I.E. Sommer in the journal Molecular Psychiatry describes some of these abnormalities and how treatments might better target them.
One such change is in brain volume. At the time of diagnosis, schizophrenia patients have a lower intracranial volume on average than healthy people. Brain growth stops around age 13, suggesting that reduced brain growth in people with schizophrenia occurs before that age.
At diagnosis, patients with schizophrenia show decrements in both white and grey matter in the brain. Grey matter volume tends to decrease further in these patients over time, while white matter volume remains stable or can even increase.
Overproduction of dopamine in the striatum is another abnormality seen in the brains of schizophrenia patients at the time of diagnosis.
Possibly years before the dopamine abnormalities are observed, underfunctioning of the NMDA receptor and low-grade brain inflammation occur. These may be linked to cognitive impairment and negative symptoms of schizophrenia such as social withdrawal or apathy, suggesting that there is an at-risk period before psychosis appears when these symptoms can be identified and addressed. Psychosocial treatments such as individual, group, or family psychotherapy and omega-3 fatty acid supplementation have both been shown to decrease the rate of conversion from early symptoms to full-blown psychosis.
Using antipsychotic drugs to treat the dopamine abnormalities is generally successful in patients in their first episode of schizophrenia. Use of atypical antipsychotics is associated with less brain volume loss than use of the older typical antipsychotics. Treatments to correct the NMDA receptor abnormalities and brain inflammation, however, are only modestly effective. (Though there are data to support the effectiveness of the antioxidant n-acetylcysteine (NAC) on negative symptoms compared to placebo.) Kahn and Sommer suggest that applying treatments when cognitive and social function begin to be impaired (rather than waiting until psychosis appears) could make them more effective.
The authors also suggest that more postmortem brain analyses, neuroimaging studies, animal studies, and studies of treatments’ effects on brain abnormalities are all needed to clarify the causes of the early brain changes that occur in schizophrenia and identify ways of treating and preventing them.
Mixed Depression
Mixed depression describes a state of depression accompanied by a few symptoms typically associated with mania. At the 2015 meeting of the International Society for Bipolar Disorders, researcher Roger McIntyre shared some findings about mixed depression.
People with mixed depression have higher levels of MHPG, which is produced as the neurotransmitter norepinephrine breaks down. They also have higher levels of the stress hormone cortisol and their depressions are more difficult to treat. Those with unipolar mixed depression may respond poorly to traditional antidepressants.
There are also medical risks associated with mixed depression. People with mixed depression are more susceptible to cardiovascular disease than are people with depressive symptoms alone.
The drugs lurasidone, olanzepine, and ziprasidone have each shown efficacy in mixed depression.
Lamotrigine potentiates the antidepressant effects of quetiapine in bipolar depression
At the 2015 meeting of the International Society for Bipolar Disorders, researcher John Geddes presented an important study showing in inadequate responders to quetiapine that compared to adding placebo, adding the anticonvulsant lamotrigine to their treatment improved depression rapidly and lastingly. Some psychiatrists have been prescribing this combination to patients for some time, but this is the first formal clinical trial documenting its efficacy. The article was published online in December in the journal Lancet Psychiatry.
Researcher Guy Goodwin described details of the study, called CEQUEL, at the meeting. It included 202 patients with bipolar I or II disorder who required treatment for a depressive episode. Participants who did not respond completely to 14 days of treatment with quetiapine were prescribed either an additional dose of lamotrigine or a placebo. Lamotrigine was very slowly titrated up to maximum doses of 200mg/day. Its antidepressant effects were striking. They began early and persisted for 50 weeks. (The published article covers only the first 12 weeks.) Response rates for the combination of quetiapine and lamotrigine were 52%, compared to 22% for quetiapine alone. Remission rates were 35% for quetiapine and lamotrigine and 12% for quetiapine alone.
Folic acid interaction
Another part of the study assessed whether folic acid supplements could improve outcomes, but in fact they did the opposite, reversing the benefits of adding lamotrigine. Geddes did not have an explanation for why this might be the case. Lamotrigine can inhibit folate metabolism, and it had been thought that adding folate would be useful. Until further data are gathered on folate augmentation in patients taking the combination of lamotrigine and quetiapine, folate should be used cautiously if at all in these patients.
Possible combination with lithium
In Goodwin’s talk, he also noted lithium’s potential to lower suicide rates, premature mortality, and cognitive impairment, and to increase hippocampal and cortical volume.
Since lamotrigine was shown to potentiate the antidepressant effects of lithium in a study by Van der Loos and colleagues, and quetiapine is approved by the Food and Drug Administration for the prevention of depression as an adjunct to lithium (or valproate), there might be theoretical acute and long-term benefits to combining the three: lithium, quetiapine, and lamotrigine.
Treating Women During Pregnancy and Breastfeeding
A Danish working group has released guidelines for prescribing psychotropic drugs to women who are pregnant or breastfeeding. After a comprehensive review of the literature, researchers from several different Danish medical societies reported that sertraline and citalopram are the first choice among selective serotonin reuptake inhibitors (SSRIs) for depression in women who are pregnant or breastfeeding. The working group suggested that women with bipolar disorder who need a mood stabilizer because of frequent relapses could be prescribed lithium, though lithium use is associated with a small risk of cardiac abnormalities in the child. Lamotrigine may also be used, and has not been associated with any congenital abnormalities.
Valproate and carbamazepine are not recommended for use during pregnancy and breastfeeding. Use of valproate among women of child-bearing age should particularly be avoided due to several risks for the potential child. These include spina bifida and other serious congenital problems, but also severe developmental delay and loss of about 9 IQ points. Other possible treatments for bipolar disorder and schizophrenia in pregnant and breastfeeding women include olanzapine, risperidone, quetiapine, and clozapine. The data about the safety of these medications are not extensive.
The working group included members of the Danish Psychiatric Society, the Danish Society of Obstetrics and Gynecology, the Danish Paediatric Society, and the Danish Society of Clinical Pharmacology. The recommendations may be found in an article by E.R. Larsen and colleagues in a 2015 supplement to the journal Acta Psychiatrica Scandinavica.
Ultrabrief Right Unilateral ECT Similar in Efficacy to Brief ECT with Fewer Side Effects
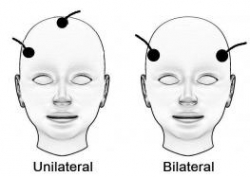 A new meta-analysis suggests that right unilateral ultrabrief electroconvulsive therapy (ECT) may be a better choice than standard brief pulse ECT for the treatment of severe depression. Researchers at the University of New South Wales in Australia led by Colleen Loo say that while standard ECT (with a pulsewidth of 1.0 ms) is recommended when urgency is paramount, ultrabrief ECT (with a pulsewidth of 0.3 ms) is better for patients at risk for cognitive side effects or those who do not require an urgent response. The researchers’ findings were reported in the Journal of Clinical Psychiatry in July.
A new meta-analysis suggests that right unilateral ultrabrief electroconvulsive therapy (ECT) may be a better choice than standard brief pulse ECT for the treatment of severe depression. Researchers at the University of New South Wales in Australia led by Colleen Loo say that while standard ECT (with a pulsewidth of 1.0 ms) is recommended when urgency is paramount, ultrabrief ECT (with a pulsewidth of 0.3 ms) is better for patients at risk for cognitive side effects or those who do not require an urgent response. The researchers’ findings were reported in the Journal of Clinical Psychiatry in July.
Loo and colleagues analyzed the findings of six different studies that compared right unilateral standard brief pulse ECT with ultrabrief pulse ECT and included a total of 689 patients. Standard ECT was more effective, producing more improvement in mood and more remissions, and working faster than ultrabrief ECT. However, standard ECT also produced greater cognitive side effects in every area tested, including thinking, learning and recall, and memory.
(When bilateral ECT is used, the cognitive effects are even worse, and researcher Harold Sacheim and colleagues have reported that the severity of the impairment in autobiographic memory is directly proportional to the number of bilateral ECT treatments a patient received, even when measured one year after the last session of bilateral ECT. This editor (Robert Post) believes bilateral ECT should be avoided if at all possible, as cognitive side effects can occasionally be severe.)
When Loo and colleagues removed nonrandomized trials from the analysis, the differences in efficacy between ultrabrief and standard right unilateral ECT were not statistically significant. Loo told Medscape Medical News that while the differences in efficacy between brief and ultrabrief ECT are minimal, the differences in side effects are greater. Right unilateral ultrabrief ECT works about as well as standard right unilateral brief pulse ECT, but preserves patients’ cognitive function better.
New TMS System Approved for Depression
In August the US Food and Drug Administration (FDA) approved the marketing of the MagVita TMS Therapy system from the company MagVenture. This machine can be used to provide transcranial magnetic stimulation (TMS) to patients with major depression that has not responded to antidepressant drugs. A TMS system uses magnets placed close to the head to stimulate the brain.
There are several existing systems that can provide TMS. The Neuronetics Neurostar TMS machine was the first one to be approved, in 2008. Then came Brainway’s Deep TMS machine. Now MagVenture says that the benefits of their new system include a simple design, low operating costs, no disposable components, and safety and efficacy rates comparable to those of other FDA-approved TMS devices.
Treatment with the MagVita system is typically provided five times per week for a duration of six weeks.
As TMS treatment becomes available to more patients, coverage by insurance companies is also increasing, but is still not guaranteed for patients in the US.
Treating Bipolar Disorder in Children and Adolescents
Bipolar disorder in childhood or adolescence can destroy academic, family, and peer relationships and increase vulnerability to drug use, unsafe sexual encounters, disability, and suicide. Treatment is critical to avoid cognitive decline. Given the potential tragic outcomes of undertreating bipolar illness, it is concerning that 40–60% of children and adolescents with bipolar disorder are not in treatment.
In a talk at the 2015 meeting of the International Society for Bipolar Disorder, researcher Cristian Zeni reviewed the existing research on the treatment of bipolar disorder in children and adolescents. A 2012 study by Geller reported response rates of 68% for the atypical antipsychotic risperidone, 35% for lithium and 24% for valproate. Risperidone was linked to weight gain and increases in prolactin, a protein secreted by the pituitary gland, while lithium was linked to more discontinuations and valproate to sedation.
For children or adolescents with aggression, researcher Robert Kowatch recommends quetiapine, aripiprazole, and risperidone. For those with a family history of bipolar disorder, he recommends lithium or alternatively, valproate plus an atypical antipsychotic.
Reseacher Robert Findling has found that lamotrigine has positive effects in childhood mania, and Duffy et al. found in a study of 21 children with mania that 13 remained stable on monotherapy with quetiapine for 40 weeks without relapse, while 5 others required combination treatment with more than one drug. In studies by Karen Wagner, oxcarbazepine was significantly better than placebo at reducing mania in younger children (ages 7–12), but not older children (13–18).
Studies by Duffy and colleagues in 2007 and 2009 recommend lithium for those with a family history of bipolar disorder, atypical antipsychotics for children with no family history of bipolar disorder, and lamotrigine for those with a family history of anxiety disorders.
In children with bipolar disorder and comorbid attention deficit hyperactivity disorder, there is universal agreement that mood should be stabilized first, and then small amounts of stimulants may be added for residual ADHD symptoms. Too often, the opposite occurs, with stimulants given prior to mood stabilization with lithium, anticonvulsants (valproate, lamotrigine, carbamazepine/oxcarbazepine) and/or an atypical antipsychotic. Read more
Cognitive Behavioral Prevention Program Can Reduce Incidence of Depression Among Teens
Adolescents whose parents have a history of depression are at greater risk for depression themselves. A new study suggests that a cognitive-behavioral prevention program aimed at these teens can reduce depression rates compared to the usual care.
The study, by David A. Brent and colleagues in the journal JAMA Psychiatry, included 316 participants aged 13–17, each of whom had a parent with a current or prior depression. Half of the participants participated in the cognitive-behavioral prevention program in addition to usual care initiated by their families. The program consisted of 8 weeks of 90-minute group sessions focused on developing positive thinking habits and improving problem solving, followed by six monthly sessions. The training was based on the Adolescents Coping with Depression program described in a June 2009 JAMA article by Garber et al.
The group who participated in the prevention program had a lower incidence of depression than the group who received only the usual care, and this difference persisted over six years of followup. Most of this effect was due to a reduced incidence of depression in the first nine months following the intervention. (Depression was roughly equal among the two groups at two later followups.)
Importantly, the benefit of the prevention program was only seen among adolescents whose parents were not depressed at the time of enrollment in the study, underscoring the importance of treating parents in order to keep the whole family healthy.
Benefits of the prevention program included reductions in onset of depression and days depressed, and improvement in interpersonal and academic competence.
Brent and colleagues say that the study shows that it is possible to prevent depression, and this can have long-term developmental consequences. They encourage focusing on the entire family’s mental health treatment.
While the main benefits came early, Brent suggests that booster sessions for teens who begin to show symptoms of depression might refresh the benefits of the prevention program at a later time.
Editor’s Note: This study has enormous health implications as depression in adolescents tends to recur and is associated with a more difficult course than depression beginning in adulthood. Preventing depressions would theoretically have positive consequences for both psychiatric and physical health, as depression is associated with increased risk of suicide and decreased longevity from increases in cardiovascular disease. Researcher Joan Luby recently reported that children with prepubescent onset of depression have decreased hippocampal volume in adolescence, so it is possible that preventing depression may have positive implications for brain volume and function.
Several Types of Psychotherapy Effective in Childhood Bipolar Disorder
Childhood onset bipolar disorder can be highly impairing. Treatment usually includes medication, but several types of psychotherapy have also been found to be superior to treatment as usual. These include family focused therapy, dialectical behavior therapy and multifamily psychoeducation groups, including Rainbow therapy.
Family focused therapy, developed by David Miklowitz, consists of psychoeducation about bipolar disorder and the importance of maintaining a stable medication routine. Families are taught to recognize early symptoms of manic and depressive episodes, and how to cope with them. Families also learn communication and problem solving skills that can prevent stressful interactions.
Dialectical behavior therapy was developed by Marsha Linehan, initially for the treatment of borderline personality disorder. It can be useful in bipolar disorder because participants learn how to manage stressors that might otherwise trigger depression or mania. DBT teaches five skills: mindfulness, distress tolerance, emotion regulation, interpersonal effectiveness, and self management.
Multifamily psychoeducation was developed by Mary Fristad. In groups, children and parents learn about mood disorders, including how to manage symptoms, and also work on communication, problem solving, emotion regulation, and decreasing family tension.
Rainbow therapy is a type of multifamily approach also known as child and family-focused cognitive-behavioral therapy (CFF CBT). It integrates individual cognitive-behavioral therapy with family psychoeducation and mindfulness skills training. In a recent article in the journal Evidence Based Mental Health, Miklowitz reviewed the current research on Rainbow therapy. While the research to date has many limitations, he highlighted some benefits of Rainbow therapy: its flexibility, and its focus on treating parents’ symptoms along with children’s illness.










