Atypical Antipsychotics with the Lowest Risk of Weight Gain
 There is a major problem of overweight and obesity in the US, with about 50% of the population affected. Patients with mood disorders, and particularly bipolar disorder, appear to be at increased risk for weight gain, which often accompanies depression. Thus, it is important that when treating these patients, doctors prescribe medications with low likelihood of weight gain.
There is a major problem of overweight and obesity in the US, with about 50% of the population affected. Patients with mood disorders, and particularly bipolar disorder, appear to be at increased risk for weight gain, which often accompanies depression. Thus, it is important that when treating these patients, doctors prescribe medications with low likelihood of weight gain.
Among the atypical antipsychotics that are widely used not only in schizophrenia but also in bipolar disorder and sometimes as adjunctive treatments in unipolar depression, there are wide differences in potential for weight gain and alterations in metabolic indices such as cholesterol, triglycerides, and blood glucose. Clozapine and olanzapine convey the greatest risk for abnormalities in these indices; risperidone and quetiapine convey moderate risk, and aripiprazole and ziprasidone are the least likely to affect metabolic indices. Newly approved lurasidone also has a mild side-effects profile.
The atypical ziprasidone (Geodon) appears to be truly weight-neutral and to have minimal impact on metabolic indices, but is not widely used due to two potential complications, neither of which must necessarily cause problems. One is the difficulty of dose titration with this drug. Surprisingly, low doses of the drug may be somewhat activating. (Atypicals are usually sedating.) Studies suggest that starting treatment with higher doses or increasing doses more quickly may be better tolerated. So rather than starting at 20mg twice a day, 40mg twice a day with rapid increases towards the range of 80mg twice a day may be associated with better tolerability. Read more
Ziprasidone Improves Mood With Possible Weight Loss Side Effects
 In an open study of bipolar disorder treatment, Shefali Srivastava, Terence Ketter and colleagues at Stanford University evaluated ziprasidone as an aid to patients unresponsive to other medications. This study was part of the multi-center research program Systematic Treatment and Evaluation Program for Bipolar Disorder, or STEP-BD. During naturalistic treatment, ziprasidone was added to an average of 3.6 other psychotropic medications and 1.2 other nonpsychotropic medications patients had already been prescribed. The researchers found substantial improvement in mood with ziprasidone, particularly in the patients who had symptomatic levels of depression at baseline. The research team also observed a mean weight decrease from 195 + 50lbs at baseline to 183 + 47lbs at the final visit, with 34.3% of the patients achieving at least a 7% weight loss with ziprasidone.
In an open study of bipolar disorder treatment, Shefali Srivastava, Terence Ketter and colleagues at Stanford University evaluated ziprasidone as an aid to patients unresponsive to other medications. This study was part of the multi-center research program Systematic Treatment and Evaluation Program for Bipolar Disorder, or STEP-BD. During naturalistic treatment, ziprasidone was added to an average of 3.6 other psychotropic medications and 1.2 other nonpsychotropic medications patients had already been prescribed. The researchers found substantial improvement in mood with ziprasidone, particularly in the patients who had symptomatic levels of depression at baseline. The research team also observed a mean weight decrease from 195 + 50lbs at baseline to 183 + 47lbs at the final visit, with 34.3% of the patients achieving at least a 7% weight loss with ziprasidone.
Mean trial duration was 860 + 700 days, with no subsequent psychotropic agents added in 51.2% of the patients who had a mean trial duration of 221 + 272 days. Ziprasidone was discontinued in 57.3% of the 82 trials after a mean of 208 + 364 days. This was due to side effects in 26.8% of the participants and due to inefficacy for mood in 23.2%.
The investigators concluded that in bipolar patients treated naturalistically with complex pharmacotherapy, ziprasidone decreased overall bipolar illness severity, was helpful in patients with substantial depression at baseline, and also yielded clinically significant weight loss in about one-third of the patients.
Editor’s note: These data are notable because they support ziprasidone’s pattern of weight neutrality and because of the overall improvement in mood symptomatology the drug brought about. Read more
Ziprasidone Does Not Seem to Cause Arrhythmias, As Once Feared
A comprehensive review of ziprasidone’s effect on the QTc interval, a measure of electrical activity in the heart, has been completed by John Kane of the Zucker Hillside Hospital in Glen Oaks, NY. He and his colleagues reviewed relevant data that had been published over the past decade. Ziprasidone can prolong the QTc interval, which theoretically puts a person at risk for cardiac arrhythmias. Kane and colleagues concluded that the effect of ziprasidone on the QTc interval is related to dose and to the patient’s baseline QTc interval.
The QTc prolongation appears to plateau at the higher end of the usual clinical dose range of ziprasidone. In their review, the researchers found no cases of a QTc interval greater than 480 milliseconds, which is thought to be the threshold for developing vulnerability to arrhythmias. Additionally, no deaths were attributed to ziprasidone in any of the studies reviewed.
Ziprasidone side effects differ in different mood states
Keming Gao from Case-Western Reserve University reviewed the adverse effects of ziprasidone monotherapy in the treatment of patients with bipolar depression, mania, or schizophrenia. Gao noted that akathisia (restless legs) and other extrapyramidal side effects (such as tremor or speech problems) during mania were more common among patients on ziprasidone than among those on placebo, and these effects were more often found in patients with mania than those with depression.
Editor’s note: The finding that these extrapyramidal side effects are more common during mania is interesting because it runs contrary to findings on another atypical antipsychotic, aripiprazole. Aripiprazole is a partial dopamine agonist, meaning it partially activates dopamine receptors, and bipolar depressed patients on aripiprazole experience more akathisia than patients taking aripiprazole for mania or schizophrenia do.
Ziprasidone fully blocks dopamine receptors, and this may explain why its effects on dopamine turnover may, in contrast to aripiprazole, convey greater risk for extrapyramidal side effects in mania than in depression. This is unusual since most side effects tend to be more prominent during the depressive phases than manic phases of the illness. The reasons for this reversal with ziprasidone deserve further investigation and clarification.
New Atypical Antipsychotic Lurasidone Appears To Improve Schizophrenia Without Weight-Gain Side Effects
 A study by a research group that included Antony Loebel of pharmaceutical company Sunovion; Steven Potkin of the University of California, Irvine; and Herbert Meltzer from Vanderbilt University summarizes data on a new atypical antipsychotic FDA-approved for treatment of schizophrenia. This agent, lurasidone (Latuda), was studied in a double-blind, placebo-controlled six-week trial in patients with schizophrenia.
A study by a research group that included Antony Loebel of pharmaceutical company Sunovion; Steven Potkin of the University of California, Irvine; and Herbert Meltzer from Vanderbilt University summarizes data on a new atypical antipsychotic FDA-approved for treatment of schizophrenia. This agent, lurasidone (Latuda), was studied in a double-blind, placebo-controlled six-week trial in patients with schizophrenia.
The drug is a new psychotropic agent that has a high affinity for dopamine D2 receptors and serotonin 5HT2A, 5HT1A, and 5HT7 receptors. (New data suggest that antagonistic effects on 5HT7 receptors may be related to antidepressant efficacy.)
In the study, patients were randomized to receive lurasidone at 80mg/day, lurasidone at 160mg/day, quetiapine XR at 600mg/day, or placebo. Evening dosing was used. Both dose levels of lurasidone resulted in significant degrees of improvement compared with quetiapine XR and placebo.
The side effects profile for lurasidone was also promising; patients were no more likely to gain weight on lurasidone than on placebo, while there was a mean 2kg weight increase on quetiapine XR. In addition, total cholesterol and triglycerides on both doses of lurasidone were similar to that on placebo, in contrast to small but significant increases on quetiapine XR.
There were significant increases in levels of prolactin (a hormone related to lactation, sex function, and bone demineralization) on lurasidone at both 80mg (+ 0.8mg/dl) and 160mg (+ 3mg/dl), while small decreases in prolactin were observed on quetiapine XR (-0.3 mg/dl) and on placebo (-0.8 mg/dl).
The data suggest that lurasidone is effective in the treatment of patients with acute exacerbation of schizophrenia, with significant effects occurring as early as day 4. This study had a low rate of adverse events. Read more
Long-Term Treatment with Lithium, Valproate, or Carbamazepine: Lithium Best for Most Patients
 Shannon Stepan, Eric Peselow and Nunzio Pomara from Maimonides Medical Center in Brooklyn, NY, have analyzed naturalistic observations of long-term maintenance treatment of bipolar disorder with valproic acid, lithium, and carbamazepine and found that patients on lithium went much longer before experiencing an episode of mania or depression than patients taking carbamazepine or valproate.
Shannon Stepan, Eric Peselow and Nunzio Pomara from Maimonides Medical Center in Brooklyn, NY, have analyzed naturalistic observations of long-term maintenance treatment of bipolar disorder with valproic acid, lithium, and carbamazepine and found that patients on lithium went much longer before experiencing an episode of mania or depression than patients taking carbamazepine or valproate.
The team followed 225 outpatients for up to 124 months, or until they had a manic or depressive episode or dropped out of the study during a well phase. Ninety-eight patients took lithium, 78 took valproate, and 50 took carbamazepine. Fifty-two percent of the participants dropped out of the study during a well phase.
One hundred three patients (45.8%) had either a manic or depressive episode during the study. This included 36.7% of the patients taking lithium, 55% of patients taking valproate, and 50% of patients taking carbamazepine. Median time until a first episode was 45 months for the entire sample, 36 months for those patients on valproate, 42 months for those on carbamazepine, and 81 months for those on lithium. A statistical analysis known as a Cox regression model indicated that patients taking valproate had a significantly higher risk of having a manic or depressive episode than those taking lithium.
Editor’s note: These naturalistic data are highly consistent with a number of more controlled clinical studies. In particular, the BALANCE study by Geddes et al. (2010) reported that lithium was superior to valproate on most outcome measures in a two-year randomized study, and that the combination of lithium and valproate was significantly better than valproate alone. Read more
L-Methylfolate Augments the Antidepressant Effects of SSRIs in Treatment-Resistant Major Depression
The B vitamin folate has been shown to be a useful augmentation treatment for patients who are nonresponsive or only partially responsive to selective serotonin reuptake inhibitor (SSRI) antidepressants. Treatment with folate works even in those who are not folate-deficient at baseline.
When folate is broken down in the body by reductase enzymes, it turns into the active form L-methylfolate, and crosses the blood-brain barrier. Maurizio Fava and colleagues at Massachusetts General Hospital (MGH) performed two placebo-controlled, randomized studies of L-methylfolate for depression. There was significantly greater improvement when SSRIs were augmented with L-methylfolate than when they were augmented with placebo. The results were significant with the use of 15mg of L-methylfolate, but not with 7.5mg, suggesting dose-related effects. Read more
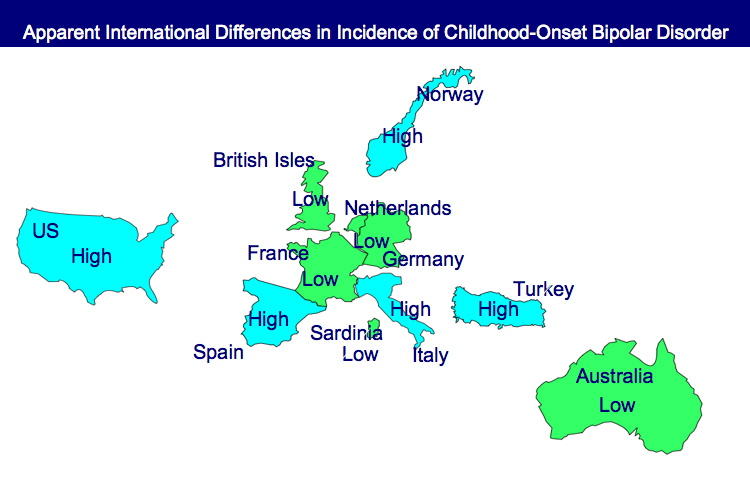
Bipolar Disorder Worse in US than Europe
New research shows that there are more early onsets of illness and more difficult courses of bipolar illness in the US than in the Netherlands or Germany.
This editor was invited to give a plenary presentation at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. The talk, titled “A greater incidence of early onset bipolar illness and poor prognosis factors in patients in the US compared with those in The Netherlands and Germany,” was based on studies in our Bipolar Collaborative Network.
We found that patients who were studied and treated at four sites in the US (Los Angeles, Dallas, Cincinnati, and Bethesda) had more poor-prognosis factors and indices of difficult courses of bipolar illness compared with patients studied in the same fashion at three sites in Utrecht, the Netherlands and Freiberg and Munich, Germany. We presented some of these data in a preliminary report in the British Journal of Psychiatry in 2008 and further analyzed these data for an article published last year in the Journal of Clinical Psychiatry. Read more
Almost 40% of Children with Bipolar Disorder May Not Receive Necessary Treatment
 An article by Geller et al. in Bipolar Disorders last year illustrates the crisis in the treatment of childhood-onset bipolar illness in the US. The article indicates that almost 40% of the children with a credible diagnosis of bipolar disorder in this study never received anything near the appropriate treatment for their illness.
An article by Geller et al. in Bipolar Disorders last year illustrates the crisis in the treatment of childhood-onset bipolar illness in the US. The article indicates that almost 40% of the children with a credible diagnosis of bipolar disorder in this study never received anything near the appropriate treatment for their illness.
It is unfortunate when children fail to receive appropriate treatment because of ambiguity about a diagnosis, but it is even more frustrating when one of the world’s experts makes a diagnosis, and a child still fails to receive treatment based on consensus guidelines.
Over 8 years of follow-up treatment in their communities, these very ill children not only did not receive helpful drugs such as atypical antipsychotics or mood stabilizers, but they often received treatments that can be counterproductive, such as antidepressants or psychomotor stimulants. Those children who did receive appropriate treatment with lithium fared better and recovered significantly earlier than the others. Read more
Treatment Guidelines for Two Hypothetical Cases in Children
There are no FDA-approved treatments for children under age 10 with bipolar disorder. For an article in Psychiatric Annals, this editor and Janet Wozniak asked experts how they would sequence treatment of a hypothetical case of a 6-year-old with extreme mood instability consistent with a diagnosis of BP -NOS (see Table I). We also asked how the experts would treat a different case of a 9-year-old with a full-blown psychotic BP-I mania (see Table II).
The results are presented and discussed in detail in the article, and are presented here to reinforce several points. The recommendations for children under 10 and for BP NOS are highly similar to consensus guidelines for older BP I children compiled by Kowatch et al.
Treatments in the face of non-response to option A or others are sequenced differently by different experts, but almost always involve an atypical antipsychotic (AA) or a mood stabilizer (MS) such as lithium, valproate, carbamazepine/oxcarbazepine, or rarely, lamotrigine. Revisions of atypical antipsychotics and mood stabilizers and use of combinations are the common next strategies.
Oxcarbazepine May Be Helpful In Pediatric Mania
Oxcarbazepine (OXC; Trileptal) is a close structural relative of carbamazepine (CBZ; Tegretol; Equetro), but unlike CBZ, OXC is not an enzyme inducer, nor does it have CBZ’s risks of rare agranulocytosis or aplastic anemia.
Wagner et al.’s report on OXC in the American Journal of Psychiatry in 2006 is typically cited as evidence the drug is ineffective for pediatric mania. But observe the figure:
While this was true of OXC’s efficacy in adolescents (due to a large placebo response—see rightmost column), OXC worked significantly better than placebo in children ages 7-12. These younger children often have more chronic presentations and BP-NOS. This may explain the low placebo response rate in the younger children.
Oxcarbazepine is considered helpful by many clinicians (See Post and Wozniak’s survey of expert treatment approaches to childhood illness, published in Psychiatric Annals in 2009) and should not be dismissed altogether.