Eat More Plants for Health
A long-term study of 130,000 nurses and other health professionals found that eating more plants lowered risk of death over several decades. A 3% increase in calories from plant protein was associated with a 10% lower risk of death during the study period.
The research, by Mingyang Song and colleagues in the journal JAMA Internal Medicine, found that the more animal protein consumed, the higher the risk of death from cardiovascular disease during the study. A 10% increase in the proportion of calories from animal protein was associated with a 2% increase in deaths. This association was worse for people who were obese or heavy drinkers.
Song and colleagues suggest that plants are a better source of calories than are animal products, and that fish or chicken are better choices than processed red meat.
Researcher Dariush Mozaffarian recommends eating plant-based foods like fruits, nuts, seeds, beans, and non-starchy vegetables, but avoiding those like French fries or white bread that have little nutritional value.
Inflammation Linked to Post-Stroke Depression
A 2016 study in the journal Psychoneuroendocrinology confirms that high levels of inflammatory cytokines in the blood are linked to higher risk of depression following a stroke.
The study, by Hee-Ju Kang and colleagues, followed 222 stroke sufferers for one year. Two weeks following the stroke, their levels of inflammatory cytokines IL-6 and IL-18 were measured. They were also assessed for depression both at the two-week point and one year later. The researchers also observed whether or not the participants were treated with statins, which are often prescribed to lower stroke risk and also have anti-inflammatory effects.
Those participants who had depression following their strokes (either at two weeks or at one year) tended to be older, to have a history of depression or stroke, to have a more severe stroke, and to have a stroke location toward the front of the brain.
Having any depression following the stroke was associated with higher levels of IL-6 and IL-18. This was particularly true of those participants who were not taking a statin. Among those taking statins, the statins may have interfered with the link between inflammatory cytokines and post-stroke depression. In the statin group, the only significant finding was a link between levels of IL-6 and depression at the two-week mark.
Depression Elevates Stroke Risk
Depression has been linked to increases in medical problems such as cardiovascular disease. A new study shows that depression is linked to increased risk of stroke, even when symptoms of depression are in remission.
The 2015 study, by Paola Gilsanz and colleagues in the Journal of the American Heart Association, focused on health and retirement. It included over 16,000 adults aged 50 and up who were interviewed every two years about their health history.
Previous studies have shown a link between depression and stroke risk. Like those studies, the study by Gilsanz and colleagues found that people who were depressed during two consecutive interviews were more than twice as likely to have a stroke in the subsequent two-year period than those who reported few depressive symptoms in the first two visits.
What is new is that in this study, people who were depressed in the first interview but not in the second interview were still at 66% greater risk for a stroke than those with no depression. Those who were depressed only during the second interview not at greater risk for a stroke, implying that depression takes more than two years to affect stroke risk.
Gilsanz and colleagues suggest that they don’t know how depression, remission, and stroke risk interact over the longer term. It is possible that stroke risk diminishes the longer a patient’s depression stays in remission.
It is not clear why depression increases strokes, though some have speculated that depression causes irregular heartbeats. There is not as yet any support for that theory, but high blood pressure, rigid veins, or sticky platelets may be other explanations.
Smoking Ban in New Jersey Jails Drastically Reduced Deaths of Inmates with Mental Illness
Policy changes by the New Jersey Department of Corrections drastically reduced the availability of tobacco products in New Jersey jails between 2005 and 2014. Prison commissaries reduced their stock of tobacco, prices increased, sales to minors were banned, and facilities were designated tobacco-free (including for staff and visitors).
Along with this reduction in the availability of tobacco products, the Department of Corrections also introduced smoking cessation programs, began offering nicotine replacement lozenges in commissaries, and increased treatment for tobacco use.
A surprise consequence of the decision to go tobacco-free was a drastic reduction of deaths among prison inmates with mental illness. The mortality rate for these inmates dropped by 48%. In contrast, the mortality rate for inmates without mental illness remained flat before and after the tobacco ban.
People with mental illness are at increased risk of mortality, particularly from cardiovascular illnesses. Now it seems that eliminating tobacco use can go a long way toward improving health and reducing mortality for these people.
Father’s Age, Behavior Linked to Birth Defects
For decades, researchers have known that a pregnant mother’s diet, hormone levels, and psychological state can affect her offspring’s development, altering organ structure, cellular response, and gene expression. It is now becoming clear that a father’s age and lifestyle at the time of conception can also shape health outcomes for his offspring.
Older fathers have offspring with more psychiatric disorders, possibly because of increased incidence of mutations in sperm.
A 2016 article by Joanna Kitlinska and colleagues in the American Journal of Stem Cells reviewed findings from human and animal studies about the links between fathers’ behaviors and their offspring’s development.
Father’s behavior can shape gene expression through a phenomenon described as epigenetics. Epigenetics refers to environmental influences on the way genes are transcribed. While a father’s behavior is not registered in his DNA sequences, it can influence the structure of his DNA or the way in which it is packaged.
Kitlinska suggests that these types of findings should eventually be organized into recommendations for prospective parents. More research is also needed into how maternal and paternal influences interact with each other.
Some findings from the article:
- A newborn can have fetal alcohol spectrum disorder even if the mother doesn’t drink. “Up to 75% of children with [the disorder] have biological fathers who are alcoholics,” says Kitlinska.
- Father’s alcohol use is linked to low birth weight, reduced brain size, and impaired cognition.
- Dad’s obesity is linked to enlarged fat cells, diabetes, obesity, and brain cancer in offspring.
- A limited diet in a father’s early life may reduce his children and grandchildren’s risk of death from cardiovascular causes.
- Dad’s advanced age is correlated with higher rates of schizophrenia, autism, and birth defects in his children.
- Psychosocial stress on dads can affect their children’s behavioral traits.
Bad Habits May Reduce Brain Volumes, May Cause Dementia
Smoking, alcohol use, obesity, and diabetes aren’t just harmful to the body. They may actually lead to dementia.
Behavioral risk factors for cardiovascular disease like those listed above have been linked to reduced volume in the brain as a whole and several brain regions, including the hippocampus, precuneous, and posterior cingulate cortex. A 2015 study by researcher Kevin King and colleagues found that these reduced brain volumes are early indicators of cognitive decline.
King and colleagues analyzed data on 1,629 participants in the long-term Dallas Heart Study. Their cardiovascular risk factors were assessed when they began the study, and their brain volume and cognitive function were measured seven years later.
Alcohol use and diabetes were associated with lower total brain volumes, while smoking and obesity were linked to low volumes in the posterior cingulate cortex.
Low hippocampal volume was linked to past alcohol use and smoking, while lower precuneous volume was linked to alcohol use, obesity, and blood glucose levels.King and colleagues suggested that subtle differences in brain volumes in midlife are the first sign of developing dementia in participants who were still younger than 50 years of age.
Inactivity in Young Adulthood May Worsen Cognition Later in Life
The couch potato lifestyle common in the US may have consequences later, in the form of deficits in memory, executive functioning (including planning and execution) and processing speed.
At the 2015 Alzheimer’s Association International Conference, researcher Kristine Yaffe and colleagues reported that low levels of physical activity and high rates of television viewing in young adulthood may reduce cognitive capabilities in midlife.
The Centers for Disease Control report that less than 50% of adults aged 18–64 get the recommended minimum of physical activity each week. The guidelines recommend at least 150 minutes of moderate intensity aerobic activity (such as walking briskly) and two or more days of muscle-strengthening activities that work all major muscle groups.
Yaffe says that physical activity can protect against cognitive decline or dementia later on.
Participants in the long-term study who reported burning fewer than 300 calories per 50-minute session three times per week during two-thirds of their followup visits had worse cognition at year 25 than those participants who were more active. Those who watched more than four hours of television per day also had reduced cognition in midlife.
Yaffe stresses that exercising regularly is not just important in keeping weight down and protecting the heart, but also in protecting the brain. Regular physical activity may even prevent illnesses such as Alzheimer’s disease.
Depression and Bipolar Disorder in Adolescence Linked to Early-Onset Cardiovascular Disease and Hardening of the Arteries
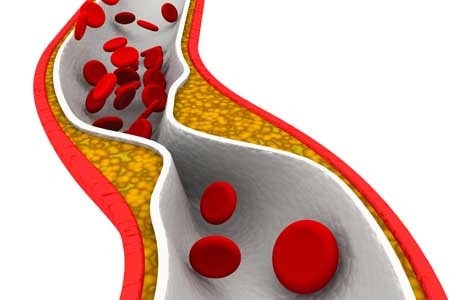
The link between mood disorders and cardiovascular illnesses has been clear for some time. Now there is evidence that this link begins early in life. In 2015, the American Heart Association issued a statement that adolescents with major depressive disorder and bipolar disorder are at increased risk for both accelerated atherosclerosis (narrowing and hardening of the arteries) and early-onset cardiovascular disease.
In the statement, the American Heart Association recommended that major depressive disorder and bipolar disorder be classified as “tier II” conditions (which also include HIV and chronic inflammatory disease) that confer a moderate risk of disease.
Until recently, it had been assumed that the increased risk of cardiovascular disease among people with depression or bipolar disorder was a result of behaviors linked to these illnesses, such as higher rates of smoking, obesity, or diabetes, which increases heart disease. Some psychiatric medication can also bring about risk factors for cardiovascular problems. It turns out that these types of factors could not fully explain the increased risk of atherosclerosis and cardiovascular disease among people who had depression or bipolar disorder in their teens.
It is not clear why depression and bipolar disorder make cardiovascular illness more likely, though it may be due to blood vessel damage resulting from inflammation or oxidative stress.
The American Heart Association recommends that pediatricians and cardiologists pay particular attention to this link by identifying and treating mental illness as early as possible and by making sure that their colleagues understand the role of mental illnesses in cardiovascular risk.
Repeated Sports Injuries Linked to Brain Inflammation
Professional football players face repeated mild traumatic brain injuries throughout their careers, and may face a variety of brain impairments, from depression to dementia, as a result.
A recent study by researcher Jennifer Coughlin and colleagues clarified how these impairments may be caused by repeated brain impacts. The researchers used positron emission tomography (PET) scans to observe the volume of translocator protein, a marker of brain injury and repair, in the brains of seven active or recently retired National Football League (NFL) players. Compared to healthy, athletic volunteers who were age-matched to the NFL players, the NFL players showed greater volume of translocator protein in several brain regions, including the left and right thalamus, the left and right temporal poles, and the brainstem.
It is not yet clear whether the increased volume of translocator protein is a sign of the brain’s attempts to repair itself, or whether it shows deterioration toward chronic traumatic encephalopathy. Translocator protein is also considered a marker of microglial activation, which occurs with inflammation.
High levels of translocator protein have also been seen in patients with depression and schizophrenia.
Low Vitamin D Linked to Small Hippocampus & Schizophrenia
Low levels of vitamin D have been linked to schizophrenia in several studies. In one, infants with low vitamin D were more likely to develop schizophrenia in adulthood, but supplementation reduced this risk. A 2015 article by Venkataram Shivakumar and colleagues in the journal Psychiatry Research: Neuroimaging found that among patients with schizophrenia who were not currently taking (or in some cases, had never taken) antipsychotic medication, low levels of vitamin D were linked to smaller gray matter volume in the right hippocampus, an area involved in schizophrenia.
Vitamin D has neuroprotective effects and is important to normal brain development and function. Vitamin D is essential to the production of brain-derived neurotrophic factor (BDNF), a protein that is important for learning and memory, and vitamin D also reduces oxidative stress. BDNF deficiency and oxidative stress have both been linked to schizophrenia, and they both can cause abnormalities in the hippocampus.