Increased Risk for Dementia in Bipolar Disorder

At the 2020 meeting of the International Society for Bipolar Disorders, researcher Flavio Kapczinski described a recent meta-analysis of 10 studies that found that bipolar disorder is a risk factor for dementia, and that lithium treatment can decrease the incidence of dementia in people with bipolar disorder.
The ten studies included a total of 6,859 participants with bipolar disorder and 487,966 healthy control participants. People with bipolar disorder were 2.96 times more likely to develop dementia than those without bipolar disorder. Five of the studies included information about treatment with lithium, which was found to decrease the risk of dementia among those with bipolar disorder by a little more than half (0.54).
Five studies also revealed that the risk of progression to dementia was higher among those with bipolar disorder than among those with major depressive disorder. In addition, one of the ten studies explored predictors of dementia in people with bipolar disorder and found that those who experienced more mood episodes had a higher risk of dementia.
Editor’s Note: It appears that the number of mood episodes a person experiences predicts dementia, and it has previously been found to predict the emergence of cognitive impairment. Prevention is the name of the game, and lithium is the best defense. My new mantra: “Prevent Episodes, Protect the Brain, Use More Lithium.”
Bipolar Disorder in Pregnancy and the Postpartum Period

At the 2020 meeting of the International Society for Bipolar Disorders, researcher Veerle Bergink reported several findings from a recent meta-analysis of articles on pregnancy and bipolar disorder. Bergink and colleagues found that pregnant women with bipolar disorder have a 37% risk of a postpartum relapse, more than twice the risk of postpartum mental disorders in the general population.
Using lithium as a treatment in the first trimester of pregnancy increased risk of congenital malformations in the fetus, but the risk was much smaller than previously thought and could be monitored by ultrasound.
Bergink and colleagues also reported that in a sample of 645 women with first-onset postpartum psychosis who received followup over a period of 7 to 25 years, 43% had no subsequent severe episodes outside of the postpartum period.
Another finding was that women with postpartum severe depression or mania had abnormalities in T cells, which are important in immune response.
Childbirth and Bipolar Disorder

In an abstract for virtual presentation at the 2020 meeting of the International Society for Bipolar Disorders, researcher Ian Jones presented evidence that childbirth may trigger onset of bipolar disorder.
Jones found that 15% of women who experience postpartum mood disorders shortly after childbirth will go on to develop bipolar disorder over time. A previous diagnosis of bipolar affective disorder is the biggest predictor that a woman will be readmitted for treatment of postpartum mental illness.
In addition, one of the biggest risk factors for postpartum mental disorders is a family history of bipolar disorder in first-degree relatives. The risk of postpartum mental disorders also increases when first-degree relatives have a psychiatric illness of any kind.
Editor’s Note: These data are consistent with research on sensitization/kindling, the idea that while early mood episodes may be triggered by psychosocial stress and other endocrine factors, later episodes may emerge more spontaneously. In this case, the stress associated with childbirth can lead to a subsequent bipolar diagnosis (with or without a precipitating stressor) in the future.
The psychosocial stress of childbirth and subsequent sleep deprivation can be severe, and those with a history of a mood disorder should seek additional support during such a time.
Cannabis Use in Adolescence Linked to Depression and Suicidality in Young Adulthood

In a meta-analysis published in the journal JAMA Psychiatry in 2019, researcher Gabriella Gobbi and colleagues analyzed findings from 11 studies including a total of 23,317 participants and found that cannabis use in adolescence (before age 18) was associated with a significantly increased risk of depression, suicidality, and suicide attempts in young adulthood (between 18 and 32 years of age).
The researchers did not find a link between cannabis use and anxiety.
Editor’s Note: Cannabis use is not as harmless as many teens may believe.
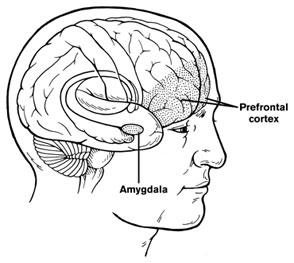
In Animal Model, Long-Term THC Exposure Interferes with Cortical Control of the Nucleus Accumbens

In an article in the journal Biological Psychiatry, researchers Eun-Kyung Hwang and Carl R. Lupica reported that in rats, long-term use of THC (tetrahydrocannabinol) weakens input from the cortex to the reward area of the brain, the nucleus accumbens (NAc). Long-term THC use also strengthens connections to the NAc from emotional control (limbic) regions, such as the basolateral amygdala and ventral hippocampus. Hwang and Lupica reason that this shift from cortical control of the NAc to limbic control likely contributes to the cognitive and psychiatric symptoms associated with cannabis use.
Editor’s Note: Street marijuana largely contains THC rather than CBD, the beneficial, anxiety-reducing component of cannabis. Cannabis products are being decriminalized, but it is important to remember that those with THC are linked to cannabis use disorder and increased susceptibility to psychiatric illness. Patients with bipolar disorder who use marijuana also have a more adverse course of illness than those who do not use it.
One Hit of THC Tied to Psychotic Symptoms in Adults with No History of Mental Illness

In a meta-analysis published in the journal Lancet Psychiatry, researcher Guy Hindley and colleagues reported that in otherwise healthy adults, a single dose of THC (equivalent to smoking one joint) produced transient psychotic symptoms.
The meta-analysis included 9 studies with a total of 196 participants. The researchers included studies in which participants took tetrahydrocannabinol (THC, the psychoactive component in marijuana) or placebo, and psychotic symptoms were measured.
The researchers also sought out studies in which cannabidiol or CBD was given in combination with THC, but there were not enough of these to derive significant results. CBD does not produce schizophrenia-like symptoms on its own, and some think it may have anti-psychotic effects, but findings on this topic have been mixed.
Taking THC had a large effect size on total psychotic symptoms and negative symptom severity (such as emotional flatness or avolition). It also had an effect on positive symptom severity (for example, hallucinations or delusions). The effects were larger with intravenous administration than with inhaled administration, and tobacco smokers had less severe positive symptoms.
Of four studies that included CBD, only one found that CBD reduced THC-induced psychotic symptoms.
Editor’s Note: Longer-term use of marijuana in adolescents and young adults doubles the risk of psychosis, and other data suggest that chronic use of marijuana at high doses can be associated with new onset of a diagnosis of bipolar disorder or schizophrenia. As cannabis products are being decriminalized around the US, it is worth noting some of the risks of marijuana use, particularly marijuana with a high level of THC.
Predicting Onset of Bipolar Disorder in Children at High Risk: Part I
 At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported.
At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported.
Symptom Progression
In offspring of parents with bipolar disorder, researcher Anne Cecilia Duffy found that symptoms in the children tended to progress in a typical sequence. Childhood sleep and anxiety disorders were first to appear, then depressive symptoms, then bipolar disorder.
Different Types of Illness May Respond Best to Different Medications
Duffy’s research also suggested links between illness features and a good response to specific medications. Those offspring who developed a psychotic spectrum disorder responded best to atypical antipsychotic medication. Those with classical episodic bipolar I disorder responded well to lithium, especially if there was a family history of lithium responsiveness. Those offspring with bipolar II (and anxiety and substance abuse) responded well to anticonvulsant medications.
If parents with bipolar disorder had experienced early onset of their illness, their children were more likely to receive a diagnosis of bipolar disorder.
The offspring of lithium-responsive parents tended to be gifted students, while those from lithium non-responders tended to be poorer students.
Comparing Risk Factors for Bipolar Disorder and Unipolar Depression
Researcher Martin Preisig and colleagues also showed that parental early onset of bipolar disorder (before age 21) was a risk factor for the offspring receiving a diagnosis of bipolar disorder. Parental oppositional defiant disorder (ODD) was also a risk factor for bipolar disorder in the offspring. The emergence of depression, conduct disorder, drug use, and sub-syndromal hypomanic symptoms also predicted the onset of mania during childhood.
Conversely, sexual abuse and witnessing violence were strong risk factors associated with a diagnosis of major (unipolar) depressive disorder. Being female and experiencing separation anxiety were also factors that predicted unipolar depression.
Predicting Conversion to Mania
Researcher Danella M. Hafeman reported that mood swings (referred to in the literature as “affective lability”), depression/anxiety, and having a parent who had an early onset of bipolar disorder were linked to later diagnoses of mania. Immediate risk factors that predicted an imminent onset of mania included affective lability, substance abuse, and the presence of sub-threshold manic symptoms.
Cannabis May Produce More Brain Changes in Teens with Bipolar Disorder than in Healthy Teens
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Benjamin Goldstein of Sunnybrook Research Institute in Toronto reported that adolescents with bipolar disorder who smoked marijuana had greater deficits in certain brain areas than did adolescents who did not have bipolar disorder. The areas affected included the dorsal lateral and rostral middle frontal cortex, and middle cortex. Goldstein concluded, “Adolescents with [bipolar disorder] may be particularly sensitive to the neurostructural effects of cannabis.”
Marijuana in general causes adverse changes in brain structure and cognition and vulnerability to paranoia and psychosis. Heavy use in adolescence is associated with an increased incidence of the onset of bipolar disorder and schizophrenia. The Goldstein data suggest several possible causal mechanisms. Those with bipolar disorder may already have brain abnormalities that are exacerbated by marijuana use. Alternatively, marijuana and bipolar disorder together may impact brain structure more than either factor alone would.
Alcohol Use Disorders That Begin Before Age 21 May Cause Lasting Changes to Amygdala
 In a 2019 article in the journal Translational Psychiatry, researcher John Peyton Bohnsack and colleagues report that people with alcohol use disorders that began before they were 21 years of age show amygdala changes that people with alcohol use disorders that began after the age of 21 do not appear to have.
In a 2019 article in the journal Translational Psychiatry, researcher John Peyton Bohnsack and colleagues report that people with alcohol use disorders that began before they were 21 years of age show amygdala changes that people with alcohol use disorders that began after the age of 21 do not appear to have.
The amygdalas of those who began abusing alcohol in adolescence showed greater expression of the long non-coding RNA known as BDNF-AS. The increased BDNF-AS was associated with decreased levels of brain-derived neurotrophic factor (BDNF) in the amygdala. BDNF protects neurons and is important for learning and memory.
According to Bohnsack and colleagues, “Adolescence is a critical period in brain development and adolescent drinking decreases orbitofrontal cortex activity and increases amygdala activity leading to less executive control, more emotional impulsivity, alterations in decision-making, and [a higher risk of engaging] in risky behaviors and develop[ing] mental health problems later in life.”
Psychiatric Risks in Offspring of Parents with Bipolar/Unipolar Disorders
 At the 2019 meeting of the International Society for Bipolar Disorders, researcher Martin Preisig and colleagues from Lausanne, Switzerland reported on a longitudinal study of mood disorders in offspring of parents with bipolar disorder, unipolar depression, or no history of psychiatric illness. The study included 446 children (with an average age of 10.1 years at the beginning of the study), who participated for an average of 11.9 years.
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Martin Preisig and colleagues from Lausanne, Switzerland reported on a longitudinal study of mood disorders in offspring of parents with bipolar disorder, unipolar depression, or no history of psychiatric illness. The study included 446 children (with an average age of 10.1 years at the beginning of the study), who participated for an average of 11.9 years.
Preisig and colleagues determined symptoms and other factors that preceded psychiatric illness. They found that bipolar disorder in the offspring was preceded by sub-threshold hypomania, major depression, and conduct disorder. Bipolar disorder in the offspring was also predicted by parental early-onset bipolar disorder.
Major depression was preceded by separation anxiety disorder, and witnessing violence or being a victim of sexual abuse.
Preisig and colleagues concluded that not only did bipolar disorder and major depressive disorder have different familial origins, they also had different antecedents and risk factors.


