Female Rodents Are More Sensitive to Defeat Stress and Its Cross-Sensitization to Cocaine
 Among rodents, being subjected to defeat stress (when an intruder mouse is threatened by a larger mouse defending its territory) can make an animal more susceptible to cocaine. This is referred to as cross-sensitization.
Among rodents, being subjected to defeat stress (when an intruder mouse is threatened by a larger mouse defending its territory) can make an animal more susceptible to cocaine. This is referred to as cross-sensitization.
Researcher Elizabeth Holly and colleagues have found that compared to males, female rodents are more sensitive to defeat stress and have greater reactions to cocaine and cocaine sensitization following this type of stress. This is probably related to a neuropeptide called corticotropin releasing factor (CRF), which is associated with cross-sensitization. When the mice were exposed to cocaine, there were increases in CRF in a part of the brain called the ventral tegmental area (VTA), which contains cell bodies of dopamine neurons that travel to the nucleus accumbens, the brain’s reward center. Blocking the CRF receptors in the VTA prevented the sensitization to cocaine from occurring in the mice.
Editor’s Note: These data in animals resemble clinical observations in humans that women are more sensitive to stress and are more prone to depression, and can have an exceedingly difficult time stopping cocaine use if they become addicted.
How Illness Progresses In The Recurrent Affective Disorders
This editor (RM Post) in collaboration with Jacqueline Fleming and Flavio Kapczinski published the article “Neurobiological mechanisms of illness progression in the recurrent affective disorders” in the Journal of Psychiatric Research this year. The article built on several themes about the progression of bipolar illness that had been explored in previous research.
These themes include:
- The likely acceleration of repeated episodes as a function of the number of prior episodes (episode sensitization)
- The increased responsivity of the illness to repeated stressors (stress sensitization)
- The increased behavioral reactivity to repeated use of psychomotor stimulants such as cocaine (stimulant-induced behavioral sensitization)
Not only are these observations well documented in the scientific literature, but recent observations also suggest that each type of sensitization can show cross-sensitization to the other two types. That is, individuals exposed to repeated stressors are more likely both to experience affective illness episodes and to adopt comorbid substance abuse. In a similar way, episodes of an affective disorder and stressors may also be associated with the relapse into drug administration in those who have been abstinent.
In addition to these mechanisms of illness progression in the recurrent affective disorders, the new article reviews the literature showing that the number of affective episodes or the duration of the illness appear to be associated with a variety of other clinical and neurobiological variables.
The number of affective episodes a patient experiences is associated with the degree of cognitive dysfunction present in their bipolar illness, and experiencing more than 4 episodes of unipolar or bipolar depression is a risk factor for dementia in late life. A relative lack of response to most treatments is also correlated with the number of prior episodes, and this holds true for response to naturalistic treatment in general. While most of these data are correlational and the direction of causality cannot be ascertained for certain, it is likely that the number of affective episodes and/or their duration could account for and drive difficulties with treatment and with cognitive function.
If this were the case, one would expect to see a variety of neurobiological correlates with the number of prior episodes or duration of illness, and in the article we summarize those that have been found in unipolar and bipolar disorder. Considerable data indicate that cortical volume and degrees of prefrontal cortical dysfunction can vary as a function of number of prior episodes. There is evidence that increased activity of the amygdala and the nucleus accumbens are also related to episodes or duration of illness. In those with unipolar depression, the volume of the hippocampus is decreased with longer duration of illness. Read more
Using the Memory Reconsolidation Window to Extinguish Drug Craving and Use
In last week’s article we discussed how fearful memories can be changed during the window in which they are reconsolidated (5 minutes to 1 hour after active recall of the long-term memory). Now the memory reconsolidation window has been used in animals and people to extinguish an addiction to cocaine or heroin. The results in humans were reported by Xue et al. in the journal Science in April 2012.
In a typical recovery scenario, a cocaine addict is repeatedly presented cocaine cues (such as paraphernalia) without the delivery of cocaine, and craving for cocaine becomes extinguished. While the patient stops craving the drug, some biological signs of the addiction remain, such as autonomic hyper-reactivity (e.g. changes in skin conductance, pulse, or blood pressure) in response to the cocaine cues. When the sober cocaine addict leaves the recovery program, he may believe he is no longer subject to cocaine craving even upon the sight of cocaine-related cues, but this craving can return spontaneously or be reactivated by cocaine-related environments or friends who were also users, and he typically relapses.
In order to make the extinction learning more powerful, it must be experienced during the reconsolidation window. In the animal experiments by Xue et al., rodents were trained to press a lever to receive an injection of cocaine or heroin. In the extinction process, the animals were returned for 15 minutes to the same environment where they had learned to press the lever and receive the drug. This was meant to activate memories associated with the drug. Then, after a 10-minute waiting period, a 180-minute extinction training was given. The process was repeated daily for 14 days and resulted in almost complete absence of relapse to drug use with passage of time (spontaneous recovery), exposure to the drug (reinstatement), or exposure to the drug-associated environment (renewal). Moreover, the expected changes in heart rate and blood pressure upon re-exposure to the drug cues were also fully extinguished. Extinction training that began one hour after activation of the memory was also successful.
When the same extinction training was given 6 hours after placing the animal in the drug administration environment, the animal remained prone to drug re-instatement and relapse in the same or different environments or spontaneously. It can be presumed that this occurred because the extinction training took place after the reconsolidation window had closed.
These well-controlled data with both cocaine and heroin self-administration in animals were then taken to the clinic to test their validity in humans.
The same procedure worked in humans addicted to heroin. Two consecutive days of sixty-minute extinction learning within the reconsolidation window, i.e. starting 10 minutes after a 5-minute retrieval of drug-associated memories by watching a video resulted in amelioration of drug craving for at least 184 days, and amazingly, as in the animals, also resulted in the loss of the unconscious biological reactivity in heart rate and to a lesser extent, blood pressure. Patients did not relapse during 6 months of followup. The same extinction process was unsuccessful when it occurred outside of the reconsolidation window, i.e. 6 hours after retrieving the drug-related memories.
Editor’s Note: These results could be of considerable potential therapeutic value in a variety of psychiatric illnesses. This process is conceptual breakthrough that has great promise for clinical use. Psychiatrists, psychologists, and patients should become familiar with these data and the principles of exploiting the reconsolidation window for potentially transformational results.
How quickly these principles can be incorporated into mainstream psychotherapeutic encounters remains to be seen. However, clinicians should begin to familiarize themselves with these data and concepts so that they can soon be put to use for more effective clinical treatment of psychiatric conditions involving pathological learning, conditioning, and habits.
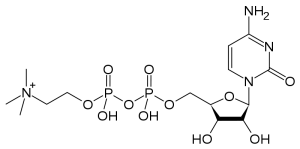
The Natural Substance Citicoline May Be Useful in Bipolar Disorder with Comorbid Stimulant Abuse
Sherwood Brown and colleagues from the University of Texas Southwestern Medical Center have completed a successful placebo-controlled trial of citicoline for bipolar and unipolar depression with comorbid methamphetamine dependence. Forty-eight participants with methamphetamine dependence and either unipolar or bipolar depression were randomized to either citicoline (2000 mg/day) or placebo for 12 weeks. Those receiving citicoline had significantly greater improvement in scores on the Inventory of Depressive Symptoms compared with those who received placebo, and patients receiving citicoline stayed in the study significantly longer, with completion rates of 41% on citicoline and 15% on placebo.
In 2007, the same team of investigators reported in the Journal of Clinical Psychopharmacology that citicoline had positive effects in bipolar patients with cocaine dependence, who experienced significant decreases in cocaine use and fewer cocaine-positive urine tests while taking citicoline.
Episodic vs. Continuous Social Stress Result in Different Rates of Cocaine Use
In a study of rodents exposed to stress (by being forced to enter another rodent’s territory) and given the opportunity to self-administer cocaine, those exposed to a few brief episodes of stress increased their cocaine use and engaged in binge-like episodes, while those exposed to stress chronically showed suppressed cocaine use.
At the American College of Neuropsychopharmacology meeting in December 2009, Klaus Miczek and colleagues from Tufts University in Boston presented a fascinating study indicating that the temporal aspects of the experience of social stress may have dramatic impact not only on defeat stress behaviors and the associated biochemistry, but also on the likelihood that an animal adopts cocaine self-administration. These investigators compared episodic versus chronic defeat stress in rodents.
Episodic social defeat stress consisted of four brief confrontations between an intruding animal and an aggressive resident rat over the course of a period of ten days. In contrast, chronic subordination stress involved the continuous exposure of the intruder rat to an aggressive resident over five weeks, during which time the intruder lived in a protective cage within the resident’s home cage.
The episodically defeated intruder rats showed increases in intravenous cocaine self-administration and prolonged binge-like episodes, along with increases in brain-derived neurotropic factor (BDNF), which is necessary for long-term learning and memory, in the midbrain ventral-tegmental area (VTA) and increased dopamine release in the nucleus accumbens, the reward area of the brain. In contrast, the continuously subordinate rats showed the opposite pattern of suppressed cocaine intake, suppression of dopamine release in the n. accumbens, and reduced BDNF in the VTA.
The N-acetylcysteine Story: A New Potential Therapy for Bipolar Illness and Substance Abuse
N-acetylcysteine (NAC), a readily available substance from health food stores, is able to reestablish glutamate homeostasis (regulation and balance) in the reward area of brain (the nucleus accumbens), reported Peter Kalivas of the University of South Carolina at the “Staging neuropsychiatric disorders: Implications for idiopathogenesis and treatment” meeting in Mojacar, Spain this past November. Kalivas reported that NAC appears to be effective across a spectrum of addictions, including cocaine, heroin, alcohol, cigarette smoking, and gambling.
Even more remarkably, NAC also appears to have positive effects in placebo-controlled studies in the treatment of patients with bipolar illness, report Mike Berk and colleagues, who are studying the same substance in Australia. Compared with placebo, patients taking adjunctive NAC showed improvement in all outcome measures, especially depression, after 3 and 6 months. In another article, also published in Biological Psychiatry in 2008, Berk’s research group demonstrated that NAC improved some negative symptoms of schizophrenia. NAC has also shown positive effects in trichotillomania and on nail-biting, suggesting that it has a variety of potential clinical uses in conditions associated with pathological compulsive behavioral patterns.