Efficacy of Direct Current Stimulation in Major Depression
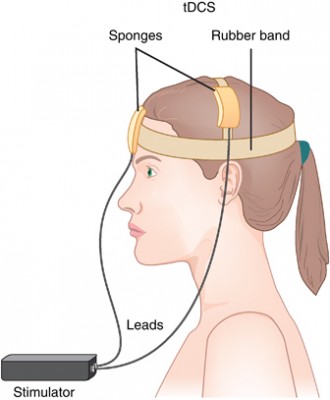 A new meta-analysis presented at the 2015 meeting of the Society of Biological Psychiatry has clarified the efficacy of transcranial direct current stimulation (tDCS) in major depression. TDCS is a treatment in which electrodes deliver a steady low level of electrical stimulation to the brain. The meta-analysis presented by Andre Brunoni and colleagues used individual patient data from six recent studies comparing tDCS treatment to a sham treatment, totaling 289 patients. TDCS treatment was superior to the sham control in terms of antidepressant response (34% to 19%), remission rates (23.1% to 12.7%), and improvement in depression.
A new meta-analysis presented at the 2015 meeting of the Society of Biological Psychiatry has clarified the efficacy of transcranial direct current stimulation (tDCS) in major depression. TDCS is a treatment in which electrodes deliver a steady low level of electrical stimulation to the brain. The meta-analysis presented by Andre Brunoni and colleagues used individual patient data from six recent studies comparing tDCS treatment to a sham treatment, totaling 289 patients. TDCS treatment was superior to the sham control in terms of antidepressant response (34% to 19%), remission rates (23.1% to 12.7%), and improvement in depression.
After adjusting for confounding factors, the researchers found that patients who had failed to respond to previous treatments were less likely to respond well to tDCS than other patients. They also found that higher doses of tDCS (in terms of current density, duration, and number of sessions) predicted a better response than lower doses.
RTMS for Depression Increases Volume of Specific Brain Regions
Repeated transcranial magnetic stimulation (rTMS) is a treatment for depression in which magnets placed near the skull stimulate electrical impulses in the brain. In a poster presented at the 2015 meeting of the Society of Biological Psychiatry, Martin Lan and colleagues presented results of the first study of structural changes in the brain following rTMS.
In the study, 27 patients in an episode of major depression underwent magnetic resonance brain scans before and after receiving rTMS treatment over their left prefrontal cortices. Lan and colleagues reported that several cortical regions related to cognitive appraisal, the subjective experience of emotion, and self-referential processing increased in volume following rTMS treatment: the anterior cingulate, the cingulate body, the precuneous, right insula, and gray matter in the medial frontal gyrus. The increases ranged from 5.3% to 15.7%, and no regions decreased in volume. More than 92% of the participants showed increased gray matter in all of these regions.
The brain changes were not correlated with antidepressant response to rTMS, but suggest a possible mechanism by which rTMS is effective in some people. Lan and colleagues concluded that rTMS likely had neuroplastic effects in areas of the brain that are important for emotion regulation.
Predictors of Bipolar Disorder in At-Risk Youth
A new longitudinal study of 391 youth at risk for bipolar disorder revealed some predictors of the disorder. The study by Danella M. Hafeman and colleagues was presented at the 2015 meeting of the Society of Biological Psychiatry. The participants were aged 6–18 and each had a parent with bipolar disorder. Over the course of the study, 40 developed an illness on the bipolar spectrum, including 21 who developed bipolar I or II. The participants were assessed for various descriptive characteristics and those who developed bipolar disorder were compared to those who developed major depressive disorder.
The most important predictors of bipolar disorder were parental assessment of internalizing symptoms of anxiety or depression, self-assessment of mood changeability, and self-assessment of hostility. A diagnosis of bipolar disorder not otherwise specified (BP-NOS) was the only predictor of a later diagnosis of bipolar I or II.
Editors Note: These data resemble findings from a 2015 study by David Axelson and colleagues in the American Journal of Psychiatry that used the same cohort of participants. The Axelson study indicated that a categorical diagnosis of a major psychiatric disorder occurred in 74% of the offspring of a bipolar parent compared to about 50% in a control group from the community. Depression, anxiety, attention deficit hyperactivity disorder (ADHD), and oppositional disorders were even more common than bipolar disorder in the at-risk population.
The presence of a major psychiatric diagnosis in about three-quarters of the offspring of a parent with bipolar disorder suggests the importance of early vigilance. One way to track symptoms of depression, anxiety, ADHD, oppositional behavior, and bipolar disorder is to join the Child Network, a secure online platform for rating children’s moods, medications, and side effects. These weekly ratings can be collected longitudinally and printed out to help parents and clinicians assess mood difficulties in their children.
Link Between Childhood Trauma and Difficult Course of Bipolar Disorder Clarified
A collaboration between Norwegian and French researchers led by Bruno Etain has clarified the pathway by which childhood trauma is linked to worse outcomes among people with bipolar disorder. The researchers, who presented their work in a poster at the 2015 meeting of the Society of Biological Psychiatry, replicated earlier findings by this editor (Robert Post) that patients who experienced trauma as a child had a more adverse course of bipolar disorder. Etain and colleagues found a link between childhood trauma and an earlier age of onset of bipolar disorder, rapid cycling, suicide attempts, and cannabis misuse.
The researchers identified more than 550 patients with bipolar disorder, who answered questionnaires about their history of bipolar disorder and childhood trauma. Their DNA was also analyzed, and the researchers found that the effect of childhood trauma on age of onset was mediated by the presence of common genetic variants in proteins related to stress (the serotonin transporter) and immune function (Toll-like receptors). They also found that the traits of mood lability (or moodiness) and impulsivity mediated the effects of trauma on clinical outcomes.
The lasting epigenetic effects of child maltreatment and adversity noted in the above abstract are consistent with a large literature showing more epigenetic effects in these individuals than in controls. While genetics are important, the impact of the environment is also substantial.
N-acetylcysteine Reduces Self-Harm, Restores Amygdala Connectivity in Young Women
 N-acetylcysteine (NAC) is an anti-oxidant nutritional supplement that has been found to reduce a wide range of habitual behaviors, including drug and alcohol use, smoking, trichotillomania (compulsive hair-pulling), and gambling. It also improves depression, anxiety, and obsessive behaviors in adults, as well as irritability and repeated movements in children with autism. A new study suggests NAC may also be able to reduce non-suicidal self-injury, often thought of as “cutting,” in girls aged 13–21.
N-acetylcysteine (NAC) is an anti-oxidant nutritional supplement that has been found to reduce a wide range of habitual behaviors, including drug and alcohol use, smoking, trichotillomania (compulsive hair-pulling), and gambling. It also improves depression, anxiety, and obsessive behaviors in adults, as well as irritability and repeated movements in children with autism. A new study suggests NAC may also be able to reduce non-suicidal self-injury, often thought of as “cutting,” in girls aged 13–21.
The open study, presented in a poster by researcher Kathryn Cullen at the 2015 meeting of the Society for Biological Psychiatry, compared magnetic resonance imaging (MRI) scans of 15 healthy adolescent girls to scans of 22 girls who had been engaging in self-injury, both before and after this latter group received eight weeks of treatment with N-acetylcysteine. Doses were 1200 mg/day for the first two weeks, 2400mg/day for the next two weeks, and 3600mg/day for the final four weeks. The girls also reported their self-injury behaviors.
Treatment with NAC reduced the girls’ self-injury behaviors. The brain scans showed that NAC also increased resting-state functional connectivity between the amygdala and the insula. Connectivity in this region helps people regulate their emotional responses. At baseline, the girls who engaged in self-harm had had deficient connectivity between the amygdala, the prefrontal cortex, insula, and the posterior cingulate cortices compared to the healthy girls, and this improved with the NAC treatment.
Midday Bright Light Therapy Effective in Bipolar Disorder
A recent study of 93 adults with bipolar disorder suggests that midday bright light therapy can be an effective adjunctive treatment for bipolar depression. The study by Dorothy Sit and colleagues was presented at the 2015 meeting of the Society for Biological Psychiatry. Participants had been diagnosed with bipolar I or II disorder, were in a current episode of depression, and were taking stable doses of mood stabilizing medication. They were randomized to receive either 7000-lux broad spectrum light for 45 to 60 minutes each day for six weeks or 50 lux dim red light. The comparison was dramatic: remission rates were 56.5% among those exposed to the 7000-lux light, and 14.3% among those who were exposed to the dim light. Those who received the bright light also reported better sleep quality and less suicidality.
Editor’s Note: These results are striking and raise the issue of whether midday bright light is more effective than early morning bright light, the usual recommendation for seasonal affective disorder (SAD) and other forms of depression. Until comparative studies are available, using midday light may be the way to go.
Maternal Infection During Pregnancy May Increase Risk of Schizophrenia in Offspring
 There is mounting evidence from animal studies and epidemiological research that an infection during pregnancy may increase the risk of schizophrenia in the offspring. A recent study by Alan Brown and colleagues presented at the 2015 meeting of the Society of Biological Psychiatry used a large dataset from the Finnish Prenatal Study of Schizophrenia to compare medical data from the mothers of 777 people with schizophrenia (630 with schizophrenia and 147 with schizoaffective disorder) to data from the mothers of 777 healthy people.
There is mounting evidence from animal studies and epidemiological research that an infection during pregnancy may increase the risk of schizophrenia in the offspring. A recent study by Alan Brown and colleagues presented at the 2015 meeting of the Society of Biological Psychiatry used a large dataset from the Finnish Prenatal Study of Schizophrenia to compare medical data from the mothers of 777 people with schizophrenia (630 with schizophrenia and 147 with schizoaffective disorder) to data from the mothers of 777 healthy people.
The study’s biobank contained blood samples taken from the mothers in early to mid-pregnancy, which the researchers used to determine the mothers’ levels of C-reactive protein (CRP), an indicator of inflammation. Higher levels of CRP were associated with increased risk of schizophrenia in the offspring. When the researchers analyzed the findings by sex of the offspring, the link between prenatal infection and schizophrenia risk was significant in males, but not females. The effect was also stronger among offspring born after their due date than those born at or before their due date.
Maternal Infection in Mice Leads to Three Generations of Behavioral Changes
Epigenetics is the process by which environmental factors affect the way a person’s genes are transcribed. These changes, which may include the addition or subtraction of methyl groups from DNA, change the DNA’s structure (how tightly it is wound around the histones that give it shape) but not its sequence. These structural changes, which affect how easily the DNA is transcribed, can then be passed on to future generations. A new study by Ulrike Stadlbauer and colleagues presented at the Society of Biological Psychiatry explored a particular pathway by which an infection in a pregnant mouse can lead to behavioral changes in three following generations of mice.
Pregnant mice were given injections that produced an infection. A first generation of offspring were interbred to create a second generation of offspring, and these were interbred to create a third generation of offspring. The first generation of offspring had epigenetic changes in methylation and hydroxymethylation to promoter regions of two enzymes that regulate synthesis of the neurotransmitter GABA, and these epigenetic changes were associated with reduced mRNA expression of these two genes.
All three generations of offspring had deficits in social interaction, short-term memory, and cued fear conditioning. Interestingly, the second and third offspring generations also exhibited depression-like behavior that had not been present in the original mothers or the first generation of offspring.
Editor’s Note: This is another fascinating demonstration of how environmental occurrences, which can include stressors, exposure to drugs, and now immune challenges, can have effects across generations, likely through epigenetic changes that persist in ova or sperm. Amazingly, it turns out that the environment can change traits in future generations, not by inducing changes to gene sequences, but through epigenetic changes to the structure of DNA or histones that persist across generations.
Early Experiences Have Lasting Effects on DNA
It is well established that certain early experiences can affect a person’s risk of developing a mental illness. Adversity in childhood, including abuse or the loss of a parent, is a risk factor not only for diagnosis of a mood disorder, but also for a more difficult course of illness. This may occur through epigenetic means. Epigenetics refers to a process by which environmental factors can change the way that DNA is transcribed, for example through the addition of methyl groups to strands of DNA. This tends to inhibit DNA from being transcribed and producing protein growth factors and other neurochemicals that are important for development.
A study by Kieran J. O’Donnell and colleagues presented at the 2015 meeting of the Society of Biological Psychiatry investigated whether epigenetics play a role in the success of a parenting intervention called the Nurse Family Partnership. Participants were 27-year-olds born to women who had received the intervention or a control intervention. Genome-wide DNA methylation was measured in the 188 participants’ blood.
Analysis of the blood revealed that the Nurse Family Partnership intervention was associated with DNA methylation at 1015 sites across 593 genes. Some of these sites were enriched for certain neurodevelopmental processes. Maltreatment in childhood was also associated with methylation at 1552 sites across 878 genes.
Editor’s Note: The take-home message of this landmark study is that maltreatment in childhood exerts lasting effects on the genome via epigenetic mechanisms, but early positive intervention also exerts lasting epigenetic effects, which likely have a normalizing impact.
Primates Shed Light on the Neurobiology of Anxiety Disorders in Children
Studies of primates suggest that the amygdala plays an important role in the development of anxiety disorders. Researcher Ned Kalin suggested at the 2015 meeting of the Society of Biological Psychiatry that the pathology of anxiety begins early in life. When a child with anxiety faces uncertainty, the brain increases activity in the amygdala, the insula, and the prefrontal cortex. Children with an anxious temperament, who are sensitive to new social experiences, are at almost sevenfold risk of developing a social anxiety disorder, and later experiencing depression or substance abuse.
A study by Patrick H. Roseboom and colleagues presented at the meeting was based on the finding that corticotropin-releasing hormone (CRH) plays a role in stress and is found in the central nucleus of the amygdala (as well as in the hypothalamus). The researchers used viral vectors to increase CRH in the central nucleus of the amygdala in young rhesus monkeys, hoping to determine what impact increased CRH has on a young brain. Rhesus monkeys and humans share similar genetic and neural structures that allow for complex social and emotional functioning.
Roseboom and colleagues compared the temperaments of five monkeys who received injections increasing the CRH in their amygdala region to five monkeys who received control injections. As expected, the monkeys with increased CRH showed increases in anxious temperament. Brain scans also revealed increases in metabolism not only in the central nucleus of the amygdala, but also in other parts of the brain that have been linked to anxiety, including the orbitofrontal cortex, the hippocampus, and the brainstem, in the affected monkeys. The degree of increase in amygdala metabolism was directly proportional to the increase in anxious temperament in the monkeys, further linking CRH’s effects in the amygdala to anxiety.