Adolescence is a Sensitive Period for Fear Learning
Adolescence can be a time of vulnerability to illness. Anxiety disorders increase during this period, and three-quarters of adults with anxiety disorders trace the illness back to their childhood or adolescence. The most common treatments for anxiety disorder are based on the idea of fear extinction. A certain stimulus, like a social situation or seeing a spider, provokes a fear reaction in the brain. Through gradually increasing exposure to the stimulus and extinction training, the person becomes desensitized to the stimulus. New research on rodents presented by Francis S. Lee at the 2015 meeting of the Society for Biological Psychiatry suggests that the extinction process is diminished during adolescence.
At specific stages of maturation, neural circuits related to particular abilities can become flexible. Brain and behavior become sensitive to and are increasingly shaped by experience. Studies of rodents and humans have shown that adolescence is a time when the neural circuitry for fear extinction is in flux. In mice, this period falls around their 29th day of life. Lee reported that around this time, the mice begin to exhibit resistance to extinction of fear learning.
In adolescent rodents, there is a surge of contextual fear learning and retrieval that is mediated by hyper-connectivity of the ventral hippocampus and the amygdala to the prelimbic part of the prefrontal cortex. In contrast, the pathway from the amygdala to the infralimbic cortex mediates the extinction of this type of learning. Because the prelimbic pathway for fear learning is overactive, the infralimbic pathway for extinction learning is less effective.
Adolescent mice temporarily lose their ability to retrieve memories related to cue-dependent (as opposed to context-dependent) fear learning. Remarkably, when these animals proceed into adulthood, the fear learning associated with cues returns and becomes accessible again.
This could help explain how teenagers can lose fear conditioning to cues (for example, speeding through a red light) they learned in childhood. The fear is forgotten (or becomes inaccessible) in adolescence, but then what had been learned is again “remembered” (retrieved) in adulthood. Read more
Ketamine: Equal Efficacy When Given With Lithium Or Valproate
Studies of rodents with depression-like behaviors revealed that the combination of low (sub-therapeutic) doses of lithium and infusions of ketamine produced antidepressant-like effects. Researchers believed this might mean that in humans, lithium might have a unique effect potentiating the effects of ketamine.
In a small study by Mark J. Niciu presented at the 2015 meeting of the Society for Biological Psychiatry, patients with bipolar depression taking lithium or valproate mood stabilizers were given ketamine infusions or control infusions. In the 23 patients taking lithium and the 13 taking valproate, ketamine’s antidepressant effects were significantly better than placebo, but there was no difference between lithium and valproate with regard to these antidepressant effects. These preliminary data in a small number of subjects do not support the proposition that lithium augments the effects of ketamine in depression.
Ketamine Temporarily Reduces Suicidal Thoughts
Intravenous ketamine can bring about rapid improvement in depressive symptoms among people with treatment-resistant depression. Because of its rapid effects, which can appear after only two hours, ketamine is being investigated as a treatment for people with suicidal thoughts.
At the 2015 meeting of the Society of Biological Psychiatry, Laili Soleimani and colleagues presented a poster about their recent double blind, randomized, controlled pilot study of ketamine inpatients and outpatients who scored highly on a measure of suicidal ideation. The 24 participants were randomized to receive either a single intravenous infusion of ketamine (0.5mg/kg) or a single infusion of midazolam (0.045 mg/kg), which shares ketamine’s anxiety-reducing effects but does not have antidepressant effects. They reported suicidal thoughts at 24 hours post-infusion, 48 hours, 72 hours, and 7 days. At 48 hours, those who received ketamine reported significantly reduced suicidal ideation compared to those who received midazolam, but this effect was no longer significant at the 72-hour mark.
The findings show that ketamine can briefly reduce suicidal ideation, and that the treatment is safe and tolerable for patients. This pilot study paves the way for further study of ketamine to reduce suicidal thinking in people who are at high risk for suicidal behavior.
Ketamine Improves Sleep and Reduces Suicidal Thoughts in Certain Patients
Intravenous ketamine is known for its fast-acting antidepressant effects, which can appear within two hours of an infusion. Researchers are now investigating its use for the reduction of suicidal thoughts. In a study presented in a poster at the 2015 meeting of the Society of Biological Psychiatry, Jennifer L. Vande Voort and colleagues compared the sleep of patients whose suicidal thoughts decreased after a single ketamine infusion (0.5 mg/kg over 40 minutes) to those whose suicidal thoughts remained.
Study participants whose suicidal thoughts diminished after one infusion of ketamine had better sleep quality the following night, with fewer disruptions in sleep than among those who did not have an anti-suicidal response to ketamine. The participants who responded well to ketamine had sleep quality similar to that of healthy controls.
Vande Voort and colleagues hope that these new findings about ketamine’s effect on sleep may provide clues to the biological mechanism behind ketamine’s effect on suicidal ideation.
A PANS Case Study, Immune Treatment Reduced Psychiatric Symptoms
Pediatric acute neuropsychiatric syndrome (PANS) is a little-known syndrome in which a child has an acute onset of psychiatric symptoms following a bacterial or viral infection, when the antibodies generated to fight the infection instead attack neurons in the brain. The behavioral alterations can be severe and resistant to the usual psychotropic drug treatments. PANS often requires antibiotics and immune-targeted therapies.
The following is a case report of a real child who had a sudden onset of depression and violence after getting sick with the flu, pneumonia, and a strep infection at the age of 4. (Names have been changed for privacy.)
Anne contacted this editor (Robert M. Post) seeking a consultation on her 6-year-old son, Jake. Two years earlier, he had suddenly become difficult—depressed, angry, and even violent. This coincided with the emergence of obsessive compulsive symptoms and urinary incontinence. He went from being able to read short sentences in pre-kindergarten, to being cognitively dull and not even able to recognize letters of the alphabet. He had been diagnosed with a mood disorder, and Anne was told it was probably bipolar disorder. But he didn’t respond to any of the typical medications, and suffered side effects including hallucinations, nightmares, bowel accidents, and worsening depression.
The best results came with the atypical antipsychotic risperidone. While it didn’t reduce all of Jake’s symptoms, Anne described it as “heaven” compared to earlier treatments. But Jake’s levels of prolactin started to increase, and he lost bladder control, so he had to stop taking risperidone. Jake’s doctor tried 18 different medication regimens with 8 different medications in less than a year without finding one that worked well. Jake had a horrible time in school, and Anne fretted about the lack of an effective, stable medication, saying, “He’s actually worse than I’ve ever seen him.”
Dr. Post recommended that they consider using high doses of quetiapine and valproate for Jake’s aggression and behavioral dyscontrol, along with the antioxidant N-acetylcysteine and vitamin D3. However, given that Jake’s symptoms were severe, involved cognitive and neurological abnormalities, and had begun after a flu-like illness, and was unresponsive to conventional treatment, Dr. Post suggested that Anne get Jake checked out for PANS and start charting Jake’s mood on a daily basis.
Jake began taking higher doses of quetiapine and valproate, and improved to the point that Anne said they restrained him only once a day, rather than four times per day. But his behavioral dyscontrol continued. In one memorable incident, after feeling picked on by other children at a baseball game, he lashed out at Anne, kicking her in the face with his cleats and punching her glasses off her face.
Anne told Dr. Post that the family had visited a neurologist, who said that she had never heard of PANS and suggested that Anne would have to travel across several states to see Dr. Post if she wanted to pursue that diagnosis.
Dr. Post encouraged Anne to keep looking for a doctor who would take the PANS idea seriously. He sent her a comprehensive review article about PANS by Dr. Kiki Chang and colleagues published in the Journal of Child and Adolescent Psychopharmacology in 2014.
This past June, Anne found a doctor who understood PANS and was willing to run the appropriate tests on Jake. The tests revealed that Jake had at one time been infected with the bacteria mycoplasma. Read more
Molecular Biology of Depression
 Dysregulation of the brain in early life can have lasting effects, and the effects of stress and depression can also accumulate. At the 2015 meeting of the Society of Biological Psychiatry, researcher Huda Akil explained that behavioral pathology can “take on a life of its own, leading to deteriorating course of illness and treatment resistance.” She illustrated how preclinical work in animals can help clarify the molecular biology of depression and develop new targets for therapeutics.
Dysregulation of the brain in early life can have lasting effects, and the effects of stress and depression can also accumulate. At the 2015 meeting of the Society of Biological Psychiatry, researcher Huda Akil explained that behavioral pathology can “take on a life of its own, leading to deteriorating course of illness and treatment resistance.” She illustrated how preclinical work in animals can help clarify the molecular biology of depression and develop new targets for therapeutics.
Early Life Experiences are Key
Akil discuss studies of rodents in which she used new molecular genetic techniques to increase the number of glucocorticoid receptors in the hippocampus early in life (prior to weaning). Glucocorticoid receptors mediate the effects of the stress hormone cortisol in people and corticosterone in rodents. More receptors help shut off cortisol secretion after a stressful event. People with post-traumatic stress disorder (PTSD) have high levels of glucocorticoid receptors while people with depression have low levels, leading to over-secretion of cortisol in depression.
The increased glucocorticoid receptors led to a long-term increase in anxiety behaviors and response to stimulants. When Akil carried out the same manipulation on rats that had already been weaned, it had no long-lasting effects, showing that there is a vulnerability window for some long-lasting effects on behavior.
CLOCK Genes and Circadian Rhythms
Akil also studied CLOCK genes in rodents. These genes, including BMAL-1, Per 1, Per 2, and Per3, play a role in circadian rhythms, and their transcription induces these 24-hour cycles. In rodents who were induced into a depression-like state, the CLOCK genes were dysregulated and did not correspond to normal circadian rhythms. These data show that depressive states can induce changes in CLOCK genes and circadian rhythms. Others have shown the converse, that abnormal CLOCK genes can induce behavioral abnormalities including mania-like behaviors.
Fibroblast Growth Factor
Levels of fibroblast growth factor 2 (FGF2) in the hippocampus are low in people with depression. In rodents, FGF2 inhibits anxiety. Decreases in FGF2 are seen in the hippocampus of animals in a depression-like state following repeated defeat by a larger animal. It appears that FGF2 is an endogenous antidepressant (i.e. one that is produced by the brain). When the rodent brain is manipulated to eliminate FGF2, the animals become anxious.
In addition, animals bred to have high stress, low social responsivity, and resistance to new learning also have low FGF2. Treatment with FGF2 reversed these behavioral abnormalities and also increased the production of new neurons. For the stressed rats, receiving FGF2 on their second day of life increased new neuron production, decreased anxiety, decreased proneness to social defeat stress and increased the bonding hormone oxytocin in the amygdala into adulthood.
FGF2 had no effect on rats bred for low stress and high social responsivity, indicating that it only worked for the rats that needed it. Akil compared FGF2 to “personalized medicine for rats.”
Defeat stress affects the way genes are transcribed, and FGF2 was able to reverse one of these specific transcriptional effects, suggesting it could potentially ameliorate some of the long-lasting effects of stress and depression.
The Human Brain
Akil also studied the brains of people who had died of depression, bipolar disorder, or schizophrenia. In bipolar disorder, the nucleus accumbens, the reward center of the brain, was enlarged.
In contrast, Akil described the brains of those people who had died with depression as being “low on fertilizer.” That is, they showed less cell growth, less production of new neurons, more abnormalities in cell shape, and more cell death. Akil said that by the time someone is severely ill, the pathology is all over the brain. The changes Akil saw in the brains of people who were depressed are also consistent with data indicating that several neuroprotective factors, including BDNF and VEG-F, are low in the frontal cortex and the hippocampus of depressed people (while BDNF is high in the nucleus accumbens).
Diabetes Complicates Bipolar Disorder
People with bipolar disorder are three times more likely than the general population to develop type 2 diabetes. Type 2 diabetes typically occurs in adulthood and is associated with insulin resistance, as opposed to type 1, which is usually diagnosed in childhood and is associated with insulin deficiency.
In a talk at the 2015 meeting of the Society of Biological Psychiatry, researcher Tomas Hajek reported that in a large group of bipolar patients, 13% reported a history of type 2 diabetes, 21% were diagnosed with type 2 diabetes upon laboratory evaluation, and 32.2% had pre-diabetes without realizing it. Thus, about half of these patients with bipolar disorder were either affected by diabetes or at risk for it, many without knowing it.
The Bad News
Diabetes complicates the course of bipolar illness. Type 2 diabetes is associated with poorer response to treatment, atrophy of the hippocampus, cognitive impairment, and higher rates of conversion from mild cognitive impairment to full-blown dementia.
The main effect of type 2 diabetes is insulin resistance. The body produces enough insulin, but insulin’s effects at its receptors are impaired. Diabetes also causes deficits in growth factors, increases in the enzyme GSK3B, decreases in mitochondria and brain-derived neurotrophic factor (BDNF, which protects neurons), and glucose toxicity.
Recent research by Hajek and colleagues shows that diabetes has several other detrimental effects on the brain in bipolar disorder. On magnetic resonance spectroscopy (MRS) scans, people with type 2 diabetes had lower levels of NAA, a marker of neuronal integrity, in the prefrontal cortex. This can indicate impaired functioning. People with type 2 diabetes also had lower levels of creatine, indicating impaired energy metabolism. In addition, hippocampal volume decreases with aging, and type 2 diabetes accelerated this age-related decline.
Some of diabetes’ effects on the brain are mediated by other health factors, including obesity, cerebral blood vessel disease (which affects white matter integrity), and side effects from medications.
What You Can Do
Start early with a good diet and exercise, and have regular checkups with a doctor, who can tell you if you have diabetes or are at risk for it. If so, start long-term preventative treatment with the most effective and easy-to-tolerate medications, and periodically have your fasting blood sugar tested. If these tests are abnormal, have your hemoglobin A1c (HbA1c) checked. This is a measure of good glucose control, and should be under 6. If it creeps upward toward 6 (a sign of pre-diabetes), the drug metformin may be able to prevent the onset of type 2 diabetes. If you have type 2 diabetes, there are several types of effective medications that can minimize its effects.
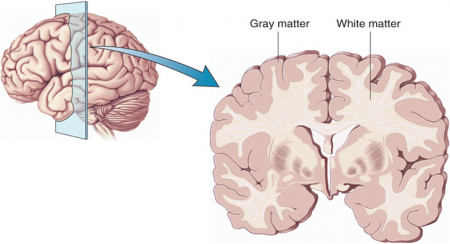
Atypical Antipsychotics May Slow Loss of Gray Matter in Schizophrenia
Progressive losses in gray matter have been observed in the cortex of people with schizophrenia, and those at high risk for the illness. In the past, studies have shown that the amount of antipsychotics a patient is exposed to is correlated with the extent of their deficits in gray matter, suggesting that antipsychotic treatment could exacerbate gray matter loss.
A new meta-analysis by Antotonio Vita and colleagues in the journal Biological Psychiatry shows that first-generation antipsychotics were associated with greater losses in gray matter compared with atypical antipsychotics, which seemed to slow the loss of gray matter.
The meta-analysis analyzed data from 18 longitudinal studies comparing a total of 1155 patients with schizophrenia to 911 healthy control participants. Magnetic resonance imaging (MRI) scans showed that over time, patients with schizophrenia lost more cortical gray matter volume. The patients’ cumulative intake of any kind of antipsychotic between MRI scans was associated with gray matter losses. But when Vita and colleagues drilled down to find differences between patients taking first-generation antipsychotics and those taking second-generation atypical antipsychotics, they found that patients with higher average daily intake of first-generation antipsychotics had greater losses in gray matter, while patients with higher average daily intake of atypical antipsychotics had less progressive losses in gray matter.
This study is the first to compare the effects of first-generation antipsychotics, which were developed in the 1960s, with those of atypical antipsychotics, which came into frequent use in the late 1980s, on cortical gray matter loss in schizophrenia. While first-generation antipsychotics are associated with the side effect of tardive dyskinesia, involuntary movements of the face and jaw, atypical antipsychotics are most commonly associated with weight gain.
Three studies have randomly assigned patients with schizophrenia to receive either first-generation or atypical antipsychotics. In these studies as well, second-generation antipsychotics were associated with smaller losses in gray matter.
The authors speculate that either second-generation antipsychotics may have neuroprotective effects, or first-generation antipsychotics may have neurotoxic effects. They also suggest that first-generation antipsychotics may not have the capacity to interfere with the natural progression of schizophrenia in terms of gray matter losses.
Future studies may investigate differences between specific antipsychotic medications’ effects on gray matter volume. Vita and colleagues reported that in the analysis, the atypical antipsychotic clozapine was associated with the least loss of gray matter of any medication in the included studies.
Editor’s Note: This study is important because it adds to findings questioning the conclusions of a large National Institute of Mental Health–sponsored study known as CATIE and a meta-analysis by John Geddes published in the journal BMJ in 2000, in which he wrote that “There is no clear evidence that atypical antipsychotics are more effective or better tolerated than conventional (first generation) antipsychotics.” Read more
Nutritional Supplement Minimizes Stress After a Natural Disaster
Certain nutritional supplements may help people cope following natural disasters. Following a 7.1 magnitude earthquake in Christchurch, New Zealand, in 2010, researchers there who were working on a clinical trial of a broad spectrum mineral and vitamin formula for ADHD realized that they could compare participants who had been taking the nutritional supplements at the time of the earthquake with those who had either already completed the trial or had not yet begun it. Two weeks after the quake, those who had been taking the multivitamin at the time of the quake were less anxious and stressed than those who hadn’t been taking the formula.
When another large earthquake struck five months later, the researchers implemented a randomized trial comparing two doses of the same broad spectrum supplement with a B Complex vitamin formula that had previously shown efficacy for stress and anxiety. Those participants taking any supplement showed fewer symptoms of post-traumatic stress disorder (PTSD) a month after the second quake compared to controls, and those taking the higher dose of the broad spectrum formula had greater improvements in mood and anxiety than those taking the B Complex supplement.
More recently, in Alberta, Canada, flooding forced many people from their homes. Researchers there who were studying the effects of micronutrients on stress and anxiety realized they had the opportunity to replicate the research from New Zealand in a different type of environmental disaster.
Researcher Bonnie J. Kaplan and colleagues recruited adults who had been affected by the flood, and randomized the participants to receive different types of supplements: vitamin D (1 pill/day); a B complex vitamin containing B6, B12, and several other nutrients (1 pill/day); or a broad spectrum supplement containing 24 vitamins and minerals and several botanical extracts (4 pills/day). No placebo was used—it was considered unethical to deny participants access to a potentially helpful treatment.
In a 2015 article in the journal Psychiatry Research, the Alberta team reported that while all of the nutrient supplements minimized stress after the flood, patients randomized to the B complex vitamin or the broad spectrum formula had less stress and anxiety following the flood than those randomized to vitamin D.
We have previously described a broad spectrum vitamin preparation called EMPowerplus, used by psychiatrist Charles Popper and psychologist Mary A. Fristad to treat children with treatment-resistant bipolar disorder. This may be the same formula used in the Alberta study. We await larger trials of this preparation in children with bipolar disorder.
Preliminary Evidence That Anti-Inflammatory Celecoxib Helps in Bipolar Depression
A study currently in progress indicates that the anti-inflammatory COX-2 inhibitor celecoxib (better known as the arthritis treatment Celebrex) may aid in the treatment of bipolar depression. In a panel session on inflammation at the 2015 meeting of the Society of Biological Psychiatry, researcher Angelos Halaris reported results from the first 26 participants.
Participants were taking mood stabilizers for bipolar disorder and became depressed. They received either 20mg/day of the selective serotonin reuptake inhibitor antidepressant escitalopram (Lexapro) plus either 200mg twice a day of celecoxib or placebo for a total of eight weeks. Those participants who received celecoxib showed greater and more rapid reductions in depression symptoms than those who received placebo.
The study will continue, and Halaris and colleagues will also observe whether measures of inflammation in patients’ blood are correlated with the patients’ responsiveness to the combined treatment with escitalopram and celecoxib.