Low Oxytocin Linked to Depression in Moms
At a panel at the 2015 meeting of the Society of Biological Psychiatry, researcher Andrea Gonzales described her team’s study of mechanisms related to postpartum depression and the bonding hormone oxytocin. In the study of 26 women at eight months postpartum, the team examined whether there were connections between a mother’s levels of oxytocin at baseline and after interacting with her child, her mood symptoms, and whether she was mistreated in childhood.
Those women who scored low on a history of maltreatment in childhood had bigger increases in oxytocin in their blood and saliva after interacting with their children. Those with high trauma scores but low levels of depression also saw big boosts in oxytocin after seeing their children. Those women who had both a history of trauma in childhood and current depressive symptoms did not get as big a boost of oxytocin after interacting with their children.
Gonzales and colleagues concluded that postpartum depression is linked to dysregulation of oxytocin levels, and that a history of trauma in the mother’s childhood can make this worse.
The researchers hope that these findings may make it easier to identify which women are at risk for postpartum depression, and that they may point to possible treatments in the future.
Postpartum depression is a problem for about 13% of mothers in the year after they give birth, and mother-child bonding may be disturbed if a mother is depressed. One way to foster better bonding between a depressed mother and her newborn is to use video feedback. A mother views video of herself interacting with her child while a trained professional helps her identify opportunities for greater physical contact.
Omega-3 Fatty Acids Prevent Conversion to Psychosis
 A new long-term study of omega-3 polyunsaturated fatty acids for psychosis prevention shows that almost seven years after a 3-month stint of receiving these dietary supplements daily, adolescents and young adults at high risk for psychosis showed fewer symptoms of conversion to full-blown psychosis than those who received placebo during the same period.
A new long-term study of omega-3 polyunsaturated fatty acids for psychosis prevention shows that almost seven years after a 3-month stint of receiving these dietary supplements daily, adolescents and young adults at high risk for psychosis showed fewer symptoms of conversion to full-blown psychosis than those who received placebo during the same period.
The research team, led by Paul Amminger, originally found that among 81 youth (mean age 16.5) at high risk of developing psychosis due to their family histories, the 41 who received 12 weeks of daily supplementation with 700mg of eicosapentaenoic acid (EPA) omega-3s and 480 mg of docosahexaenoic acid (DHA) omega-3s showed reduced likelihood of conversion to psychosis one year later than the 40 who received placebo.
The team followed up an average of 6.7 years later with 71 of the original 81 participants. Among those who had received the omega-3 intervention, 9.8% had developed psychosis. Among the placebo group, 40% had developed psychosis, and they had done so earlier.
In addition, the omega-3 participants were better functioning, they had required less antipsychotic medication, and they had lower rates of any psychiatric disorder than the placebo group.
Amminger wrote in the journal Nature Communications, “Unlike antipsychotics, fish oil tablets have no side effects and arent’s stigmatizing to patients.”
Editor’s Note: Because of their lack of side effects, a good case can be made for omega-3 fatty acids for patients at high risk for psychosis. The novel thing about this study is that short-term treatment with omega-3 fatty acids had preventive effects almost 7 years later.
Blood and Now Brain Inflammation Linked to Depression
 There is growing evidence of a link between inflammation of depression. At the 2015 meeting of the Society of Biological Psychiatry, researcher Jeff Meyer summarized past studies on inflammatory markers. These are measurements, for example of certain proteins in the blood, that indicate the presence of inflammation in the body.
There is growing evidence of a link between inflammation of depression. At the 2015 meeting of the Society of Biological Psychiatry, researcher Jeff Meyer summarized past studies on inflammatory markers. These are measurements, for example of certain proteins in the blood, that indicate the presence of inflammation in the body.
Common inflammatory markers that have been linked to depression include IL-6, TNF-alpha, and c-reactive protein. At the meeting, Meyer reviewed the findings on each of these. Twelve studies showed that IL-6 levels are elevated in the blood of patients with depression. Four studies had non-significant results of link between IL-6 and depression, and Meyer found no studies indicating that IL-6 levels were lower in those with depression. Similarly, for TNF-alpha, Meyer found 11 studies linking elevated TNF-alpha with depression, four with non-significant results, and none showing a negative relationship between TNF-alpha and depression. For c-reactive protein, six studies showed that c-reactive protein was elevated in people with depression, six had non-significant results, and none indicated that c-reactive protein was lower in depressed patients.
Most studies that have linked inflammation to depression have done so by measuring inflammatory markers in the blood. It is more difficult to measure inflammation in the brain of living people, but Meyer has taken advantage of new developments in positron emission tomography (PET) scans to measure translocator protein binding, which illustrates when microglia are activated. Microglial activation is a sign of inflammation. Translocator protein binding was elevated by about 30% in the prefrontal cortex, anterior cingulate cortex, and insula in study participants who showed symptoms of a major depressive episode compared to healthy control participants. The implication is that the depressed people with elevated translocator protein binding have more brain inflammation, probably via microglial activation.
The antibiotic minocycline reduces microglial activation. It would be interesting to see if minocycline might have antidepressant effects in people with depression symptoms and elevated translocator protein binding.
Autopsy Studies Show Brain Inflammation in Unipolar Depression, Bipolar Disorder, and Suicide
 Depression and bipolar disorder have been linked to high levels of inflammatory proteins in the blood (namely CRP, IL-1, IL-6, and TNF-alpha), but the relationship between these illnesses and inflammation in the brain has not been well-characterized.
Depression and bipolar disorder have been linked to high levels of inflammatory proteins in the blood (namely CRP, IL-1, IL-6, and TNF-alpha), but the relationship between these illnesses and inflammation in the brain has not been well-characterized.
At the 2015 meeting of the Society for Biological Psychiatry, researcher Ghanshyan Pandey discussed findings from autopsy studies of people who died with a diagnosis of unipolar depression or bipolar disorder, and teens who died of suicide. The studies compare data from these ill people with those of controls who are matched for demographic characteristics.
Pandey found that the brains of those who died of unipolar depression and bipolar disorder showed more signs of inflammation compared to the controls. This included elevated levels of the inflammatory proteins IL-1B, IL-6, and TNF-alpha, in addition to elevated levels of the mRNA that leads to their production. Pandey also found that those with depression and bipolar disorder had higher levels of mRNA for the receptors to which TNF-alpha and other inflammatory proteins attach themselves.
Pandey performed similar autopsy studies of teens who died of suicide, the second leading cause of death for this age group, compared to teens who died of other causes. There were more signs of inflammation in the prefrontal cortices of teens who died of suicide. These included mRNA and proteins for IL-1B and TNF-alpha, and IL-6 proteins. In contrast to the ill adults, the teens who died of suicide had lower levels of the receptors for inflammatory proteins than controls. Another type of receptor known as toll-like receptors was higher in the ill teens, particularly the mRNA and proteins TLR3 and TLR4.
US Lags Behind Canada in Access to RTMS
At the 2015 meeting of the Transcranial Magnetic Stimulation Society, Linda Carpenter, an American researcher who specializes in repeated transcranial magnetic stimulation (rTMS), a method of treating depression by using a magnetic coil placed near the scalp to stimulate neurons, compared notes with Jeff Daskalakis, a Canadian researcher who also studies rTMS.
Carpenter described the limited approval rTMS enjoys in the US. RTMS has been approved by the Federal Drug Administration for the treatment of unipolar depression under very limited parameters (only at a frequency of 10Hz). RTMS has limited availability in the US, and many healthcare companies do not cover it. Providers face scrutiny of study recruitment practices and recordkeeping by insurers and the Joint Commission (formerly the Joint Commission of Accreditation of Healthcare Organizations), which assesses healthcare quality.
In contrast, Daskalakis and his Canadian colleagues can and do use rTMS to treat a broader range of illnesses including bipolar disorder. In Canada rTMS is used to treat unipolar depression, schizophrenia, post-traumatic stress disorder (PTSD), and obsessive-compulsive disorder (OCD), and clinicians can adjust the parameters to treat adolescents and the elderly.
The situation in the US is unfair. Because rTMS has not been approved for the treatment of bipolar disorder, Carpenter and other clinicians in the US are unable to treat bipolar depression even though a wide range of experts and published studies report that rTMS is as effective (or possibly even more so) for patients with bipolar depression than for those with unipolar depression.
Few treatments are available for bipolar depression. The discrepancy is even sadder when one considers that there are already more than 20 FDA-approved antidepressants that can be used to treat unipolar depression, but only three approved medications for bipolar depression. Bipolar depression is an orphan illness, which lacks a powerful voice advocating for more treatment research about optimal therapeutic strategies. Read more
RTMS in the Elderly and After ECT
At the 2015 meeting of the Society of Biological Psychiatry in May, researcher Daniel Blumberger reported to this editor (Robert M. Post) that he has found repeated transcranial magnetic stimulation (rTMS) to be effective for depression in late life. Blumberger noted that it may be necessary to use higher intensity stimulation (i.e. at 120% of motor threshold instead of the usual 110% of motor threshold) in the elderly in order to overcome the gap between the skull and the brain, which can grow with age due to brain atrophy.
Blumberger has also successfully used rTMS as a followup treatment to a successful course of electroconvulsive therapy (ECT), administering rTMS twice a week for up to 66 treatments in a given patient in order to maintain remission of their depression.
Deep TMS May Reduce OCD Symptoms
Obsessive compulsive disorder (OCD) occurs in about 2% of the population worldwide. Selective serotonin reuptake inhibitor (SSRI) antidepressants are the most commonly used treatment for OCD, but not all patients respond adequately to them.
At the 2015 meeting of the Transcranial Magnetic Stimulation Society, researcher Joseph Zohar presented evidence that deep transcranial magnetic stimulation (deep TMS) targeted over the medial prefrontal cortex may reduce OCD symptoms. In TMS treatment, an electromagnetic coil is placed against the patient’s head and magnetic pulses that can penetrate the scalp are converted into small electrical currents that stimulate neurons in the brain. In Zohar’s study, patients with OCD were randomized to receive deep TMS at frequencies of either 20 Hz or 1 Hz, or a sham procedure. The 20 Hz deep TMS resulted in a 28% reduction in OCD symptoms compared to the other two groups, indicating that the 20 Hz treatment had a large effect size.
In addition to the deep TMS procedures, all patients also received cognitive behavioral therapy, high doses of SSRIs, and relapse prevention training.
Editor’s Note: It is interesting that 20 Hz deep TMS, which activates the prefrontal cortex, was more effective than 1 Hz, which decreases activity there. Other attempts to treat OCD have focused on suppressing frontal-striatal-thalamic circuits, which are overactive in the disorder. Since the medial prefrontal cortex is an important area for the new learning required for the extinction of anxiety symptoms in a variety of disorders, increasing activity in this medial prefrontal target area with 20 Hz may activate that extinction process allowing new learning rather than nonspecifically suppressing hyperactive frontal-striatal-thalamic circuits as 1 Hz TMS would do.
Studies of Medications and RTMS in Children Lacking
At the 2015 meeting of the Transcranial Magnetic Stimulation Society in May, researcher Stephanie Ameis discussed the dearth of medication studies in children, particularly for depression but also for schizophrenia and autism spectrum disorders, which share the symptom of impaired executive functioning, which can include skills such as planning and problem solving.
Ameis noted that in a literature review, there were a total of 1046 controlled pharmacological treatment studies in adults compared to only 106 in children, which reflects a relative absence of treatment knowledge, especially for depression (where there were 303 studies in adults versus only 17 in children) and bipolar disorder (where there were 174 studies of adults and 24 of children).
Ameis then reviewed the few studies of rTMS for depression in young people. She identified several series with only a total of 33 children and adolescents who had been treated with rTMS. She is beginning to study rTMS in patients with high-functioning autism (40 patients aged 16 to 25 have been randomized in her study). Ameis also described a 2013 study of rTMS in which patients with schizophrenia showed improved performance on a test of working memory published by Mera S. Barr and colleagues in the journal Biological Psychiatry. Ameis cited this as a rationale for studying rTMS’s effect on cognitive performance in people with autism.
Bloomberg Covers Ketamine as a Depression Treatment
Over the years, we’ve tried to keep readers updated about ketamine‘s use as a fast-acting antidepressant. Bloomberg Business recently covered how the drug is being used by some to treat depression.
RTMS Study Identifies Glutamate as a Biomarker for Depression Treatment
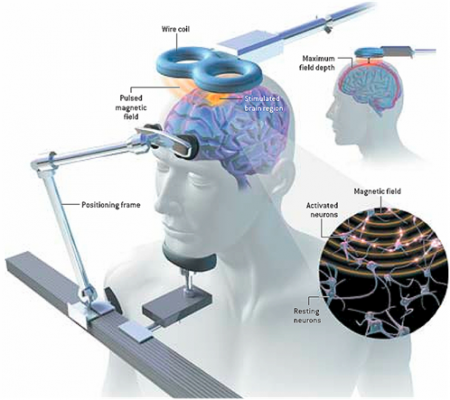 At the 3rd Annual Meeting of the Transcranial Magnetic Stimulation Society, Canadian researcher Frank MacMaster discussed his study of repeated transcranial magnetic stimulation (rTMS) in 50 children with depression. RTMS is a non-invasive procedure in which an electromagnetic coil is placed against the side of the forehead and magnetic pulses that can penetrate the scalp are converted into small electrical currents that stimulate neurons in the brain. The study was designed to identify biomarkers, or characteristics that might indicate which patients were likely to respond to the treatment. All of the patients received rTMS at a frequency of 10 Hz. Using magnetic resonance spectroscopy (MRS) technology, MacMaster found that children who responded well to rTMS treatment had low levels of the neurotransmitter glutamate at the beginning of the study, but their glutamate levels increased as their depression improved. Children who didn’t improve had higher glutamate levels at the beginning of the study, and these fell during the rTMS treatment.
At the 3rd Annual Meeting of the Transcranial Magnetic Stimulation Society, Canadian researcher Frank MacMaster discussed his study of repeated transcranial magnetic stimulation (rTMS) in 50 children with depression. RTMS is a non-invasive procedure in which an electromagnetic coil is placed against the side of the forehead and magnetic pulses that can penetrate the scalp are converted into small electrical currents that stimulate neurons in the brain. The study was designed to identify biomarkers, or characteristics that might indicate which patients were likely to respond to the treatment. All of the patients received rTMS at a frequency of 10 Hz. Using magnetic resonance spectroscopy (MRS) technology, MacMaster found that children who responded well to rTMS treatment had low levels of the neurotransmitter glutamate at the beginning of the study, but their glutamate levels increased as their depression improved. Children who didn’t improve had higher glutamate levels at the beginning of the study, and these fell during the rTMS treatment.
MacMaster hopes that glutamate levels and other biological indicators such as inflammation will eventually pinpoint which treatments are likely to work best for children with depression. At the meeting, MacMaster said that in Canada, only a quarter of the 1,200,000 children with depression receive appropriate treatment for it. Very little funding is devoted to research on children’s mental health, a serious deficit when one considers that most depression, anxiety, attention deficit hyperactivity disorder (ADHD), bipolar disorder, oppositional behavior, conduct disorder, and substance abuse begins in childhood and adolescence, and early onset of these illnesses has been repeatedly linked to poorer outcomes.
Editor’s Note: The strategy of identifying biomarkers is an important one. MacMaster noted that this type of research is possible due to the phenomenal improvements in brain imaging techniques that have occurred over the past several decades. These techniques include magnetic resonance imaging (MRI) to a resolution of 1 mm; functional MRI; diffusion tensor imaging (DTI), which can depict the connectivity of white matter tracts; and spectroscopy, which can be used to identify chemical markers of neuronal health and inhibitory and excitatory neurotransmitters, and analyze membrane integrity and metabolic changes. These methods provide exquisite views of the living brain, the most complicated structure in the universe. The biomarkers these techniques may identify will allow clinicians to predict how a patient will respond to a given treatment, to choose treatments more rapidly, and to treat patients more effectively.






