CRP, A Readily Available Marker of Inflammation, Predicts Response To Two Antidepressants
C-reactive protein, or CRP, is a protein found in blood plasma, the levels of which rise in response to inflammation. In a recent study, levels of CRP were able to predict which of two antidepressants a patient was more likely to respond to.
The 2014 article by Rudolph Uher et al. in the American Journal of Psychiatry reported that low levels of CRP (<1 mg/L) predicted a good response to the selective serotonin reuptake inhibitor (SSRI) escitalopram (Lexapro) while higher levels of CRP predicted a good response to the tricyclic antidepressant nortriptyline, a blocker of norepinephrine reuptake.
The research was part of the Genome-Based Therapeutic Drugs for Depression (GENDEP) study, a multicenter open-label randomized clinical trial. CRP was measured in the blood of 241 adult men and women with major depressive disorder. In the article the researchers say that CRP and its interaction with medication explained more than 10% of the individual variance in response to the two antidepressants.
If these findings can be replicated with these and similarly acting drugs, it would be a very large step in the direction of personalized medicine and the ability to predict individual response to medications.
Another promising open study of minocycline in bipolar depression
Joanna Soczynska in Roger McIntyre’s lab at the University of Toronto presented a poster at the 2014 meeting of the International College of Neuropsychopharmacology (CINP) on the anti-inflammatory and neuroprotective antibiotic minocycline.
Twenty-seven patients with a major depression received minocycline in addition to the medications they were already being prescribed. Dosage was 100mg twice a day. Treatment with adjunctive minocycline was associated with significant improvement on several scales that measure depression severity.
Editor’s Note: What was particularly interesting was that a subset of patients achieved complete remission, raising the question whether these patients might have markers of inflammation that would predict this excellent response. The authors concluded that the “results provide a rationale for testing minocycline’s efficacy in a larger randomized, placebo-controlled trial.”
Exactly this type of study was proposed a year ago by researcher Andy Nierenberg and given the best marks by a National Institute of Mental Health review committee but was turned down for funding because the National Institute of Mental Health has implemented a new initiative, Research Domain Criteria (RDoC), that lays out new criteria for research, limiting funding to those studies that focus on a molecular target that spans several diagnoses.)
Digestion of Wheat and Milk Releases Peptides that Might Cause Inflammation
Some people have found that gluten-free or casein-free diets have improved their intestinal, autoimmune, or neurological symptoms. (Casein is a protein found in mammals’ milk. Cow milk is high in casein while human milk proteins are 20–45% casein.) One explanation for the good effects of these diets is that peptides that are released during digestion of these foods can create epigenetic changes in gene expression, adding methyl groups to DNA strands that increase inflammation.
As infants transition from getting all of their nutrition from the placenta to using their gastrointestinal tract, their diet may lead to epigenetic modifications that affect their health later in life. Epigenetics refers to changes in genes that do not affect the inherited sequence of DNA, but affect how easily the DNA is transcribed to produce proteins. Methyl or acetyl groups can be added to DNA or the histones around which it is wound.
When a person digests casein (from either human or animal milk) or gliaden (a protein derived from wheat), peptides are released that activate opioid receptors, modulating the uptake of the amino acid cysteine in neurons and in the gastrointestinal tract. This decrease in cysteine uptake is associated with drop in the antioxidant glutathione and a methyl donor (a molecule with a reactive methyl group that can easily become part of another molecule) called S-Adenosyl methionine.
In addition to decreasing cysteine uptake, the peptides also increase DNA methylation and create epigenetic changes in genes involved in redox (changes in oxidation) and methylation homeostasis.
These processes are described in a 2014 article by Malav S.Trivedi et al. in the Journal of Nutritional Biology. Trivedi et al. conclude that milk and wheat can change antioxidant activity and gene expression. Differences in the peptides in human and cow milk may explain developmental differences between children who are breastfed and those who receive formula.
The decrease in antioxidants caused by peptides from wheat and milk can predispose people to inflammation and oxidation, explaining why wheat- or casein-free diets might be useful.
Inflammation Predicts Depression Persistence
Links between inflammation and depression continue to be identified in new research. Researcher N. Vogelzangs et al. reported in a 2014 article in Neuropharmacology that inflammatory and metabolic dysregulation in antidepressant users predicted an outcome of depression two years later. Elevated levels of the marker of inflammation Il-6, low HDL (or “good”) cholesterol, high triglycerides, and high blood sugar were associated with poor response to medication and chronicity of depression. Of 315 people treated with antidepressants (average age 43), 138 were in remission at 2 years, while 177 (56.2%) were still depressed. People with four or more types of inflammatory or metabolic dysregulations had a 90% chance of still being depressed at 2 years.
Among inflammatory markers including CRP and TNF-alpha, IL-6 alone was associated with chronic depression. Il-6 can cross the blood-brain barrier. We have previously reported that researcher Scott Russo found that in rats in a depression-like state known as defeat stress (brought about by repeated defeat by a larger rodent), blocking Il-6 can prevent depressive behaviors such as social avoidance or loss of preference for sucrose.
Like inflammation, metabolic abnormalities also complicate depression. Lipid dysregulation and hyperglycemia are associated not only with depression persistence, but also with the new onset of depression in humans.
Vogelzangs et al. conclude that these data “ suggest that inflammatory and metabolic dysregulation worsens depression course owing to reduced [antidepressant] response and that alternative intervention treatments may be needed for depressed persons with inflammatory and metabolic dysregulation.”
It is noteworthy that a 2014 meta-analysis of the anti-inflammatory drug celecoxib (Celebrex) published by Farhad Faridhosseini et al. in Human Psychopharmacology, showed that the drug, often prescribed for arthritis, is effective for unipolar depression when added to patients’ regular treatment.
It remains to be ascertained whether celecoxib’s effects are seen in depression in general, or if they pertain only to the 30% of depressed patients who show inflammation at baseline. Typical markers of inflammation include Il-6, CRP, TNFa, and Il-1.
Statins, prescribed to lower cholesterol, also have anti-inflammatory effects, and are also effective in preventing depression.
Determining treatment approaches for those patients showing signs of inflammation or metabolic irregularities remains a high priority for study. The preliminary data noted here suggest that treating these dysregulations in those with depression may be useful.
Inflammation Occurs During Both Depression And Mania
There is increasing evidence of a link between mood disorders and inflammation in the body.
At the 2014 meeting of the International Society for Bipolar Disorders, Shang-Ying Tsai discussed increases in measures of inflammation that occur in bipolar disorder as a function of the clinical state of depression, mania, or euthymia (remission). He found that in both mania and depression, there were elevations in various markers of inflammation: STNF-R1, CRP, IL-Ira and SLR-2r. However, SLR-2r showed some particularly interesting results. In mania, elevation of SLR-2r, a marker of cell-mediated inflammation, was state-related, meaning it increased during an episode of mania and remained normal during euthymia. In depression, SLR-2r elevation was trait-related, or persistently elevated (even in remission).
Editor’s Note: This study adds to a growing list of studies that confirm the presence of inflammation in patients with bipolar disorder compared to normal controls, including a 2012 article by Tsai in the Journal of Affective Disorders. How elevations in inflammatory markers in a given individual should direct specific types of treatment intervention remains to be further clarified.
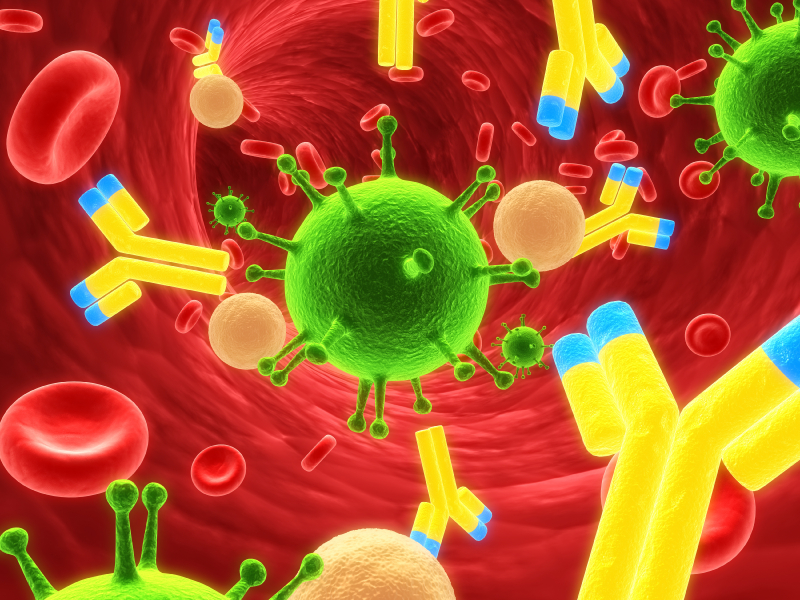
Immune Response in Mania
While the reasons why one person develops bipolar disorder and another does not remain mysterious, the current thinking is that genes contribute some risk while immunological abnormalities contribute other risks. Researchers have identified certain antibodies whose levels spike during an episode of mania, as if the patient is having an immune reaction. These are referred to as biomarkers or inflammatory markers.
While various biomarkers for mania have been identified, until recently their effects had only been examined independently. A 2013 article by Dickerson et al. published in the journal PLOS ONE examined four biomarkers in combination. Each was a type of antibody: to the NR peptide of the NMDA receptor, to gliadin (a protein derived from gluten), to Toxoplasma gondii (a parasitic protozoan), and to Mason-Pfizer Monkey Virus. Measures of these four types of antibodies made up a combined inflammation score for participants in the study.
The study compared 57 patients presenting with a manic episode with 207 non-psychiatric controls and 330 patients who had had recent onset of psychosis, schizophrenia, or bipolar depression. The combined inflammation score of the mania group was significantly higher than the other groups at the time of hospital admission and at the time of evaluation several days later. It had returned to normal (i.e. not different from the other groups) at followup six months later, although those with the highest combined inflammation scores were at risk for re-hospitalization during that period.
The findings of this study suggest that hospitalization for mania is associated with immune activation, and the level of this activation predicts subsequent re-hospitalization. Treatments for mania that target this inflammatory response should be investigated.
Inflammatory and Metabolic Abnormalities Predict Poor Response to Antidepressants
 There is mounting evidence that inflammation and metabolic problems are related to depression. A recent study by Vogelzangs et al. in the journal Neuropsychopharmacology examined 313 patients being treated for depression to see whether levels of inflammatory markers in the blood and metabolic factors such as cholesterol, blood pressure, and waist circumference predicted whether those patients would still (or again) be diagnosable with depression two years later.
There is mounting evidence that inflammation and metabolic problems are related to depression. A recent study by Vogelzangs et al. in the journal Neuropsychopharmacology examined 313 patients being treated for depression to see whether levels of inflammatory markers in the blood and metabolic factors such as cholesterol, blood pressure, and waist circumference predicted whether those patients would still (or again) be diagnosable with depression two years later.
Several factors predicted later depression, including high levels of the inflammatory marker interleukin-6, low HDL (“good”) cholesterol, higher than normal triglycerides, and high blood glucose (hyperglycemia).
People who had four or more types of inflammatory or metabolic abnormalities had almost twice the odds of having chronic depression. Among those study participants who had only recently begun taking antidepressant medication, having four or more of these risk factors made them almost 7 times more likely to be depressed during follow-up.
One explanation for the connection between inflammatory and metabolic dysregulation and depression is that inflammation and metabolic problems worsen and complicate a patient’s depression and reduce the patient’s responsiveness to traditional antidepressants. Alternative ways of treating these patients aimed at their inflammation and metabolism may be necessary.
How Inflammation Increases Glutamate Overexcitation And Neurotoxicity
Research has shown a link between inflammation and mental illness. Inflammation leads to a series of chemical changes that can overexcite neurons and interfere with the protection of neurons.
Inflammation increases the production of indoleamine-pyrrole 2,3-dioxygenase (IDO), an enzyme that breaks down the amino acid tryptophan into kynurenic acid and quinolinic acid. They in turn increase glutamate, the main excitatory neurotransmitter, and decrease brain-derived neurotrophic factor (BDNF), which keeps neurons healthy.
Kynurenic acid stimulates microglia, which clean up the central nervous system as a form of immune defense, to produce inflammatory cytokine proteins.
Quinolinic acid directly stimulates glutamate receptors and encourages glutamate release from astrocytes. Quinolinic acid also blocks glutamate removal that would normally occur through reuptake into the astrocytes, leading to more stimulation of extrasynaptic glutamate receptors and decreases in BDNF.
Quinolinic acid’s effects are opposite to those of the antidepressant ketamine, which blocks glutamate NMDA receptors and increases BDNF. When people are given interferon protein for the treatment of cancers, quinolinic acid increases in cerebrospinal fluid, inducing depression. The severity of depression induced is correlated with the patient’s levels of quinolinic acid.
It appears that ketamine has indirect anti-inflammatory effects through its ability to block glutamate receptors and increase BDNF.
Finding Treatments That Work For Each Patient
At a recent scientific meeting, researcher Andrew H. Miller presented data on infliximab, an inhibitor of the inflammatory cytokine TNF alpha that is used to treat rheumatoid arthritis and is being explored for the treatment of depression. As previously reported in BNN Volume 16, Issue 2 from 2012, the drug was not effective overall among the depressed patients, but in a subgroup of patients with high levels of the inflammatory marker CRP, infliximab was highly effective. Miller emphasized that patients do not fail to respond to treatments; it is doctors who fail, or drugs that fail. He explained that there is tremendous heterogeneity in people’s illnesses, and doctors must get better at sorting out what treatments will work for each patient, striving toward personalized therapeutics.
There are many clinical correlates or predictors of nonresponse to antidepressants used in unipolar depression. These include inflammation, obesity, stress in childhood, anxiety disorder comorbidity, substance abuse comorbidity, and medical comorbidity.
Editor’s Note: How do we doctors target these clinical correlates of illness for better therapeutic effects? We are just starting to learn, and until we identify good markers for predicting illness, the best we can do is carry out carefully sequenced clinical trials of medications and therapies with different mechanisms of action.
Patients can assist their physicians and clinicians by engaging in precise, preferably nightly charting of their mood, functioning, medications, life events, side effects, and other symptoms such as anxiety on a personal calendar. Several of these are available for free download, and there are other longitudinal screening instruments, such as the website and app What’s My M3.
A good personal response to a novel treatment or a poor response to an Federal Drug Administration–approved treatment trumps anything that is written in the research literature. The best way to achieve the best outcome is to engage in excellent monitoring of symptoms and side effects that can guide the next steps in therapeutics.
Depression May Not Be All in Your Head
 Repeated social defeat stress (when an intruder mouse is repeatedly threatened by a larger mouse defending its home territory) is often used as a model to study human depression. Animals repeatedly exposed to social defeat stress start to exhibit depression-like behaviors such as social avoidance and loss of interest in sucrose. Georgia Hodes, a researcher at Mount Sinai School of Medicine, reported at a recent scientific meeting that repeated defeat stress–induced behavior was blocked when IL-6, an inflammatory cytokine released by white blood cells in the blood, was inhibited. The central nervous system did not appear to be involved.
Repeated social defeat stress (when an intruder mouse is repeatedly threatened by a larger mouse defending its home territory) is often used as a model to study human depression. Animals repeatedly exposed to social defeat stress start to exhibit depression-like behaviors such as social avoidance and loss of interest in sucrose. Georgia Hodes, a researcher at Mount Sinai School of Medicine, reported at a recent scientific meeting that repeated defeat stress–induced behavior was blocked when IL-6, an inflammatory cytokine released by white blood cells in the blood, was inhibited. The central nervous system did not appear to be involved.
Interestingly, mice with more white blood cells and more IL-6 release at baseline (prior to the social defeat stress) were more likely to show the defeat-stress depressive behaviors.
Editor’s Note: The higher number and greater reactivity of white blood cells seen in these mice could be a clinical marker of vulnerability to defeat stress, and such findings are worthy of study in human depression. White blood cells are critical to fighting infection and sometimes their overactivity can contribute to inflammation. In meta-analyses, a subgroup of depressed patients consistently show elevated inflammatory markers (including IL-1, IL-6, TNF alpha, and CRP), and it remains to be seen whether these markers of inflammation are generated in the central nervous system or come from white blood cells in the blood, and whether their targeted suppression could be a new route to antidepressant effects (as in the study of defeat stress in mice).