Anxiety, Depression, Unstable Mood, and Low-Level Mania Best Predictors of Bipolar Disorder
Researchers are looking for better ways of predicting whether children at risk for bipolar disorder will go on to develop the illness. A 2015 study by David Axelson and colleagues in the American Journal of Psychiatry reported that in the offspring of parents with bipolar disorder, diagnoses of sub-threshold mania, depression, and disruptive behavior disorders were associated with subsequent diagnosis of full-blown Bipolar I or Bipolar II disorders six to seven years later.
More recently, in an article by Danella M. Hafeman and colleagues in the American Journal of Psychiatry, the same group of investigators has examined how symptoms (rather than categorical diagnoses, as in the earlier study) predict the development of bipolar disorder. In children and adolescents at high risk for bipolar disorder (because they have a parent with the disorder) three types of symptoms were the best predictors of later bipolar disorder: anxiety/depression at the time participants entered the study, unstable mood or irritability both when entering the study and shortly before a bipolar diagnosis, and low-level manic symptoms observed shortly before diagnosis.
The earlier the age at which a parent was diagnosed with a mood disorder, the greater the risk that the offspring would also be diagnosed with bipolar disorder. Youth with all four risk factors (anxiety or depression, mood changes, low-level mania, and a parent who was diagnosed with a mood disorder at an early age) had a 49 percent chance of developing bipolar disorder, compared to a 2 percent chance among those without those risk factors.
Childhood onset of bipolar disorder and long delays until first treatment for depression or mania are both significant predictors of a poor outcome in adulthood compared to adult onsets and shorter delays to treatment. Read more
Vitamin D3 Reduces Symptoms of Bipolar Spectrum Disorders
 Vitamin D3 tends to be low in children and adolescents with mania, but supplements may help. In a small open study published in the Journal of Child and Adolescent Psychopharmacology in 2015, Elif M. Sikoglu and colleagues administered 2000 IU of vitamin D3 per day to youth aged 6–17 for eight weeks. Sixteen of the participants had bipolar spectrum disorders (including subthreshold symptoms) and were exhibiting symptoms of mania. Nineteen participants were typically developing youth.
Vitamin D3 tends to be low in children and adolescents with mania, but supplements may help. In a small open study published in the Journal of Child and Adolescent Psychopharmacology in 2015, Elif M. Sikoglu and colleagues administered 2000 IU of vitamin D3 per day to youth aged 6–17 for eight weeks. Sixteen of the participants had bipolar spectrum disorders (including subthreshold symptoms) and were exhibiting symptoms of mania. Nineteen participants were typically developing youth.
At the beginning of the study, the youth with bipolar spectrum disorders had lower levels of the neurotransmitter GABA in the anterior cingulate cortex than did the typically developing youth. Following the eight weeks of vitamin D3 supplementation, mania and depression symptoms both decreased in the youth with bipolar spectrum disorders, and GABA in the anterior cingulate cortex increased in these participants.
Editor’s Note: GABA dysfunction has been implicated in the manic phase of bipolar disorder. While larger controlled studies of vitamin D supplementation are needed, given the high incidence of vitamin D deficiency in youth in the US, testing and treating these deficiencies is important, especially among kids with symptoms of bipolar illness.
Successful Double-Blind Placebo-Controlled Study of Lithium for Acute Mania in Kids 7–17
Lithium is the treatment of choice for adults with bipolar disorder, but has rarely been studied in children or adolescents. One of the first double-blind placebo-controlled trials of lithium for the treatment of mania in children and teens aged 7–17 showed that the drug produced greater improvement in mania than did placebo. Side effects included blurred vision, abdominal pain, diarrhea, nausea, vomiting, fatigue, thirst, increased thyroid-stimulating hormone, decreased appetite, dizziness, sedation, tremor, increased urination, and rash.
In the study by researcher Adelaide S. Robb and colleagues, which was presented at the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, doses began at 300mg twice a day, were based on each child’s weight, and were slowly increased.
At the same meeting, researcher Russell Scheffer presented data on 41 children who continued lithium treatment for 16 weeks with good results. The mean dose was 27.8 +/- 6.7 mg/kg per day.
Omega-3 Fatty Acids Associated with Small Improvement in Depression in Children Aged 7–14
At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Mary A. Fristad reported that omega-3 fatty acid supplements had a small beneficial effect on depression in children aged 7–14. The supplements did not noticeably improve bipolar disorder not otherwise specified (NOS) or mania. The supplements consisted of several types of omega-3 fatty acids, including 1400mg of EPA, 200mg of DHA, and 400mg of others per day. The children were also undergoing psychotherapy during the study.
Children at Risk for Bipolar Disorder May Have Adverse Reactions to Antidepressants
 At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Jeffrey R. Strawn reported that among children at high risk for bipolar disorder (because of a family history of the disorder) who are prescribed antidepressants for depression and anxiety, adverse reactions are common. These reactions include irritability, aggression, impulsivity, and hyperactivity, and often lead to discontinuation of the antidepressant treatment.
At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Jeffrey R. Strawn reported that among children at high risk for bipolar disorder (because of a family history of the disorder) who are prescribed antidepressants for depression and anxiety, adverse reactions are common. These reactions include irritability, aggression, impulsivity, and hyperactivity, and often lead to discontinuation of the antidepressant treatment.
Younger patients at risk for bipolar disorder were more likely to have an adverse reaction to antidepressants. Risk of an adverse reaction decreased 27% with each year of age.
RTMS Improves Executive Function in Kids with Schizophrenia and Autism
 Researcher Stephanie Ameis reported at the 2015 meeting of the American Academy of Child and Adolescent Psychiatry that following repeated transcranial magnetic stimulation (rTMS), a treatment in which a magnetic coil placed over the scalp delivers electric pulses to the brain, children with schizophrenia and autism spectrum disorders showed improvements in executive function, including working memory. The rTMS treatment targeted the left dorsolateral prefrontal cortex.
Researcher Stephanie Ameis reported at the 2015 meeting of the American Academy of Child and Adolescent Psychiatry that following repeated transcranial magnetic stimulation (rTMS), a treatment in which a magnetic coil placed over the scalp delivers electric pulses to the brain, children with schizophrenia and autism spectrum disorders showed improvements in executive function, including working memory. The rTMS treatment targeted the left dorsolateral prefrontal cortex.
Offspring of Bipolar Parents at High Risk for Psychiatric Disorders
Researcher Juan David Palacio reported at the 2015 meeting of the American Academy of Child and Adolescent Psychiatry that compared to offspring of non-ill parents, children of parents with bipolar I disorder are at high risk for psychiatric disorders, particularly bipolar spectrum disorders and substance use disorders. They were also at risk for symptoms of anxiety disorders and conduct disorder. Palacio’s findings from Colombia mirror those from other studies of familial risk and suggest the importance of vigilance to detect these disorders early and provide appropriate treatment. Our Child Network may help.
Diagnosing Childhood Bipolar Disorder: Mom Knows Best
In a talk at the 2015 meeting of the International Society for Bipolar Disorders, researcher Eric Youngstrom showed that mothers’ evaluation of their children’s psychiatric symptoms was more valid than both teacher ratings and the children’s own evaluations. Parents were better at detecting irritability, while children were better at assessing their energy levels and the quality of their sleep.
Youngstrom reported that about 2% of children worldwide are diagnosed with bipolar disorder. However, when bipolar disorder not otherwise specified (BP NOS), a diagnosis given when symptoms do not meet the diagnostic criteria for Bipolar I or II, is included in the statistics, rates of bipolar disorder among children in the US reach about 6%.
Youngstrom mentioned that an epidemiological study by Kathleen Merikangas found that among children in the US with a bipolar spectrum diagnosis, only 22% were in treatment, compared to 38% of those with depression and 60% of those with ADHD.
Parents of children (aged 2–12) with mood, anxiety, and behavioral disorders are invited to join the Child Network, our program for tracking weekly symptoms which can then be printed out longitudinally to share with the child’s doctor.
Reduced Cognitive Function and Other Abnormalities in Pediatric Bipolar Disorder
 At the 2015 meeting of the International Society for Bipolar Disorders, Ben Goldstein described a study of cognitive dysfunction in pediatric bipolar disorder. Children with bipolar disorder were three years behind in executive functioning (which covers abilities such as planning and problem-solving) and verbal memory.
At the 2015 meeting of the International Society for Bipolar Disorders, Ben Goldstein described a study of cognitive dysfunction in pediatric bipolar disorder. Children with bipolar disorder were three years behind in executive functioning (which covers abilities such as planning and problem-solving) and verbal memory.
There were other abnormalities. Youth with bipolar disorder had smaller amygdalas, and those with larger amygdalas recovered better. Perception of facial emotion was another area of weakness for children (and adults) with bipolar disorder. Studies show increased activity of the amygdala during facial emotion recognition tasks.
Goldstein reported that nine studies show that youth with bipolar disorder have reduced white matter integrity. This has also been observed in their relatives without bipolar disorder, suggesting that it is a sign of vulnerability to bipolar illness. This could identify children who could benefit from preemptive treatment because they are at high risk for developing bipolar disorder due to a family history of the illness.
There are some indications of increased inflammation in pediatric bipolar disorder. CRP, a protein that is a marker of inflammation, is elevated to a level equivalent to those in kids with juvenile rheumatoid arthritis before treatment (about 3 mg/L). CRP levels may be able to predict onset of depression or mania in those with minor symptoms, and is also associated with depression duration and severity. Goldstein reported that TNF-alpha, another inflammatory marker, may be elevated in children with psychosis.
Goldstein noted a study by Ghanshyam Pandey that showed that improvement in pediatric bipolar disorder was related to increases in BDNF, a protein that protects neurons. Cognitive flexibility interacted with CRP and BDNF—those with low BDNF had more cognitive impairment as their CRP increased than did those with high BDNF.
Offspring of Parents with Psychiatric Disorders At Increased Risk for Disorders of Their Own
At a symposium at the 2015 meeting of the International Society for Bipolar Disorder, researcher Rudolph Uher discussed FORBOW, his study of families at high risk for mood disorders. Offspring of parents with bipolar disorder and severe depression are at higher risk for a variety of illnesses than offspring of healthy parents.
Uher’s data came from a 2014 meta-analysis by Daniel Rasic and colleagues (including Uher) that was published in the journal Schizophrenia Bulletin. The article described the risks of developing mental illnesses for 3,863 offspring of parents with schizophrenia, bipolar disorder, or major depression compared to offspring of parents without such disorders.
Previous literature had indicated that offspring of parents with severe mental illness had a 1-in-10 likelihood of developing a severe mental illness of their own by adulthood. Rasic and colleagues suggested that the risk may actually be higher—1-in-3 for the risk of developing a psychotic or major mood disorder, and 1-in-2 for the risk of developing any mental disorder. An adult child may end up being diagnosed with a different illness than his or her parents.
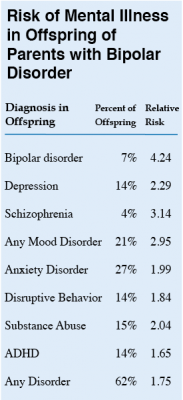 At the symposium, Uher focused on families in which a parent had bipolar disorder. These families made up 1,492 of the offspring in the Rasic study. The table at right shows the risk of an illness among the offspring of bipolar parents compared to that risk among offspring of healthy parents, otherwise known as relative risk. (For example, offspring of parents with bipolar disorder are 4.24 times more likely to be diagnosed with bipolar disorder themselves than are offspring of non-bipolar parents.) The table also shows the percentage of offspring of parents with bipolar disorder who have each type of disorder.
At the symposium, Uher focused on families in which a parent had bipolar disorder. These families made up 1,492 of the offspring in the Rasic study. The table at right shows the risk of an illness among the offspring of bipolar parents compared to that risk among offspring of healthy parents, otherwise known as relative risk. (For example, offspring of parents with bipolar disorder are 4.24 times more likely to be diagnosed with bipolar disorder themselves than are offspring of non-bipolar parents.) The table also shows the percentage of offspring of parents with bipolar disorder who have each type of disorder.
Editor’s Note: These data emphasize the importance of vigilance for problems in children who are at increased risk for mental disorders because they have a family history of mental disorders. One way for parents to better track mood and behavioral symptoms is to join our Child Network.







