Omega-3-Fatty Acids Promising For At-Risk Kids with Depression
 Several studies in adults and children suggest that omega-3 fatty acid supplementation may have antidepressant effects. At the 2013 meeting of the American Academy of Child and Adolescent Psychiatry in October, Melissa DelBello, a professor at the University of Cincinnati, reported on a new study of omega-3 fatty acids in depressed children who had a parent with bipolar disorder. The children taking omega-3 fatty acids were more likely to improve than those taking a placebo, but the findings were only of marginal significance.
Several studies in adults and children suggest that omega-3 fatty acid supplementation may have antidepressant effects. At the 2013 meeting of the American Academy of Child and Adolescent Psychiatry in October, Melissa DelBello, a professor at the University of Cincinnati, reported on a new study of omega-3 fatty acids in depressed children who had a parent with bipolar disorder. The children taking omega-3 fatty acids were more likely to improve than those taking a placebo, but the findings were only of marginal significance.
Cold-water fish are a good source of omega-3 fatty acids, and DelBello said salmon is by far the best in this regard. People who live in countries where fish is consumed in greater quantities are less likely to suffer from depression. Other sources of omega-3 fatty acids include shellfish, plant and nut oils, English walnuts, flaxseed, algae oils, and fortified foods.
The omega-3 fatty acids from fish are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), while the omega-3 fatty acids from plants are alpha-linolenic acid (ALA), which breaks down into EPA and DHA. All of these are anti-inflammatory, though one must consume much greater quantities of ALA to match the benefits of EPA and DHA. In contrast, omega-6 fatty acids, which are much more common in the typical American diet, are pro-inflammatory.
In DelBello’s study of 56 depressed children of a parent with bipolar disorder, the participants were randomized to either 1.8 g of omega-3 fatty acids (1.2 g of EPA and 0.6 g of DHA) or placebo (olive oil). Those who received the omega-3 fatty acids had a 55.6% rate of remission versus 34.5% for those who received placebo, but while the odds ratio of 2.4 favored the omega-3 fatty acids, the difference in remission rates was not statistically significant, likely because of the small size of the study. However, improvement on the Children’s Depression Rating Scale was significantly different across the two groups, with children taking omega-3s improving more. Omega-3 fatty acids are known to have an anticoagulant effect (preventing the clotting of blood), and four children in the study did have prolonged clotting times (but no clinical problems with bleeding).
Editor’s Note: Given the existing literature on omega-3 fatty acids and the trend in this study, omega-3s are worthy of consideration for the treatment and potentially for the prevention of depression in children. This later possibility is further suggested by findings from Australia that, when compared to placebo, omega-3 fatty acids significantly reduced the rate of conversion from prodromal (preliminary) psychotic symptoms to a full-blown diagnosis of schizophrenia.
Loss of Appetite or Weight in Depressed Parents Predicts Depression in Children
 Depression in a parent is one of the factors that best predicts whether a young person will develop depression. Since depression symptoms can vary greatly from person to person and some symptoms are known to be more heritable than others, new research is investigating whether a parent’s profile of symptoms affects their child’s likelihood of developing the illness. A 2013 study by Mars et al. in the Journal of Clinical Psychiatry suggests that loss of appetite or weight in a parent with depression is the symptom that most strongly predicts new onset of depression and depressive symptoms in their offspring.
Depression in a parent is one of the factors that best predicts whether a young person will develop depression. Since depression symptoms can vary greatly from person to person and some symptoms are known to be more heritable than others, new research is investigating whether a parent’s profile of symptoms affects their child’s likelihood of developing the illness. A 2013 study by Mars et al. in the Journal of Clinical Psychiatry suggests that loss of appetite or weight in a parent with depression is the symptom that most strongly predicts new onset of depression and depressive symptoms in their offspring.
The study observed 337 parent-child pairs. The parents (mostly mothers), who had a history of recurrent unipolar depression, ranged in age from 25–55 years, and their children ranged from 9–17 years. The study lasted four years, during which the families participated in three assessments. Parents’ symptoms were recorded and children were also assessed for symptoms or new development of depression. Thirty percent of the offspring whose parents reported weight loss or low appetite were found to have new onset of depression at followup, compared to nine percent of the offspring whose parents did not have these symptoms.
There are nine symptoms used to diagnose depression in the Diagnostic and Statistical Manual for Mental Disorders: low mood, loss of interest (anhedonia), loss of energy, change in appetite or weight, change in sleep, low self-esteem or guilt, suicidality, psychomotor slowing (retardation), and loss of concentration or indecisiveness. Of these, parental loss of appetite or weight was the only symptom that predicted depression in a child. Interestingly, the severity of parental depression or the presence of other health problems in the parent did not account for the emergence of illness in the children.
Suggestions for Physicians Treating Parents with Bipolar Disorder
- Support Pregnant Women with Bipolar Disorder
A. Depression during pregnancy is more common among women with bipolar disorder than among controls–consider cognitive behavioral therapy, omega-3 fatty acids, folate, & rTMS
B. 52% incidence of post-partum depression (3x higher than controls)–Monitor closely and treat accordingly - Ask Your Affectively Ill Patients About Their Children
- Encourage Good Diet and Exercise in These Children
- Encourage Watchful Waiting in Families with Children at High Risk
- If a Child becomes Symptomatic, Suggest:
A. Family Focused Therapy (FFT), or other Family-Based Treatment
B. Low-Risk Interventions Like Nutrition and Sleep Hygiene - If a Child Develops BP-NOS, Encourage:
A. Mainstream Pharmacotherapy
B. Increased Social Support (Family, Friends, Advocacy) - If a Child Develops BP-I, Encourage Ongoing Monitoring & Medication
- If an Adolescent Becomes Manic, Educate About Substance Abuse and Attempt Primary Prevention of a Substance Abuse Disorder
Youth at High Risk for Bipolar Disorder Show White Matter Tract Abnormalities
 At a recent scientific conference, researcher Donna Roybal presented research showing that children at high risk of developing bipolar disorder due to a positive family history of the illness had some abnormalities in important white matter tracts in the brain. Prior to illness onset, there was increased fractional anisotropy (FA), a sign of white matter integrity, but following the onset of full-blown bipolar illness there were decreases in FA.
At a recent scientific conference, researcher Donna Roybal presented research showing that children at high risk of developing bipolar disorder due to a positive family history of the illness had some abnormalities in important white matter tracts in the brain. Prior to illness onset, there was increased fractional anisotropy (FA), a sign of white matter integrity, but following the onset of full-blown bipolar illness there were decreases in FA.
Roybal postulated that these findings show an increased connectivity of brain areas prior to illness onset, but some erosion of the white matter tracts with illness progression.
Editor’s Note: It will be critical to replicate these findings in order to better define who is at highest risk for bipolar disorder so that attempts at prevention can be explored.
Lithium Reduces Suicide Rate and Increases Longevity
 Suicide is an unfortunate consequence of bipolar disorder in 10-15% of patients. A study by Manchia et al. examined suicidal behavior in 737 families of bipolar patients, including 4,919 first-degree relatives. Suicidal behavior ran in families and was more prevalent in those with an early age of onset and a shorter duration of illness. The good news: lithium treatment decreased suicide risk independent of its degree of effectiveness in treating bipolar disorder. Those on lithium also had a longer median age of survival (73 versus 65 years).
Suicide is an unfortunate consequence of bipolar disorder in 10-15% of patients. A study by Manchia et al. examined suicidal behavior in 737 families of bipolar patients, including 4,919 first-degree relatives. Suicidal behavior ran in families and was more prevalent in those with an early age of onset and a shorter duration of illness. The good news: lithium treatment decreased suicide risk independent of its degree of effectiveness in treating bipolar disorder. Those on lithium also had a longer median age of survival (73 versus 65 years).
Editor’s Note: These data are consistent with a variety of other studies and raise the question why lithium is used less frequently in the US than in many European countries and Canada. Given its neuroprotective effects, its prevention of suicide and dementia, and its positive effects on longevity, it is hard to see why lithium is not included in the treatment regimens of more patients (at whatever dosage is well-tolerated), even if it alone is not sufficient for treating their manic and depressive episodes.
Research (by this editor Robert Post and colleagues) shows that bipolar disorder is a more pernicious illness in almost all respects in the US compared to the Netherlands and Germany (International Journal of Neuropsychopharmacology, 2011). Whether bipolar illness would be less severe in the US if it were more often treated with lithium is an unanswered question. The field cannot provide an answer with systematic prospective controlled data, as most study designs would be unethical (i.e. would deny useful treatment to suffering patients), although one large randomized comparative study called BALANCE did show the superiority of lithium over valproate. However, individual patients in consultation with their physician could evaluate the evidence and request that lithium be considered in their treatment regimen.
If a patient has some clinical predictors of a likely good response to lithium, the decision to include lithium should be a slam-dunk. Some of these include: a positive family history of mood disorder, especially bipolar disorder; a classic course with distinct episodes and clear periods of wellness; manic episodes that are euphoric as opposed to dysphoric (i.e. anxious/irritable); lack of an anxiety disorder or substance abuse comorbidity; the absence of mood-incongruent delusions; and a sequence of episodes of mania followed by a depression and then a well interval (MDI) rather than the sequence of DMI.
Family History Of Alcoholism Predicts Positive Response To Ketamine
 The drug ketamine can bring about antidepressant effects rapidly when given intravenously, but these effects last only a few days. In a recent study, bipolar depressed patients with alcoholism or a family history of alcoholism in first-degree relatives had a more extended positive antidepressant response to IV ketamine than those without this history, and fewer adverse effects from the treatment. The study, published by David Luckenbaugh et al. from the National Institute of Mental Health in the journal Bipolar Disorders in December 2012, replicates similar findings in patients with unipolar depression, where positive family history of alcoholism also predicted better response and fewer adverse effects from IV ketamine.
The drug ketamine can bring about antidepressant effects rapidly when given intravenously, but these effects last only a few days. In a recent study, bipolar depressed patients with alcoholism or a family history of alcoholism in first-degree relatives had a more extended positive antidepressant response to IV ketamine than those without this history, and fewer adverse effects from the treatment. The study, published by David Luckenbaugh et al. from the National Institute of Mental Health in the journal Bipolar Disorders in December 2012, replicates similar findings in patients with unipolar depression, where positive family history of alcoholism also predicted better response and fewer adverse effects from IV ketamine.
Alcohol and ketamine have a common mechanism of action. They are both antagonists of the glutamate NMDA receptor, meaning they limit the effects of glutamate, the major excitatory neurotransmitter in the brain. This suggests a theoretical explanation for why a history of alcoholism might relate to ketamine response.
Editor’s Note: Family history appears to be linked to how patients respond to different mood stabilizers. Lithium works best in those patients with a positive family history of mood disorders (especially bipolar disorder). Carbamazepine works best in those without a family history of bipolar disorder among first-degree relatives. Lamotrigine works best in those with a positive family history of anxiety disorders or alcoholism.
Drugs that are effective in patients with a family history of alcoholism all target glutamate in the brain. Lamotrigine decreases glutamate release, while ketamine reduces glutamate’s effects at the receptor. Both decrease glutamate function or activity. Like lamotrigine, carbamazepine also decreases glutamate release and has good effects in those with a history of alcoholism.
Memantine is another mood-stabilizing drug that is an antagonist of the NMDA receptor, like ketamine and alcohol. It will be interesting to see whether memantine will also be successful in those with a personal or family history of alcoholism.
Anxiety and Depressive Disorders Often Precede the Onset of Bipolar Disorder in Those At High Risk Due to Family History
At the 2012 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) meeting, Anne Duffy and Gabrielle A. Carlson sponsored a symposium on the association between anxiety and minor mood disorders and subsequent bipolar disorder in those at high risk. Researchers presenting at the symposium consistently found that there is a sequence in which young people at high risk for bipolar disorder develop increasingly severe illnesses: first anxiety, then mood disorders, then bipolar illness.
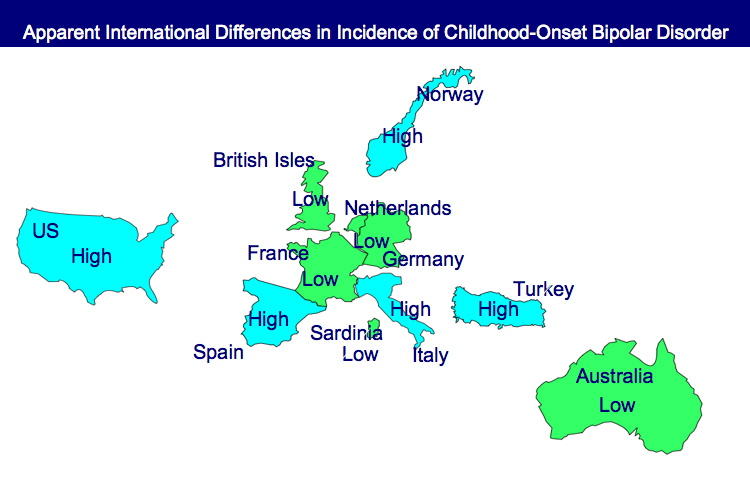
One difference: the incidence of childhood-onset bipolar disorders in those at high risk because a parent has the disorder was lower in Canada, Switzerland, and the Netherlands than it was in the US.
Duffy, a professor of psychiatry in Calgary, noted that bipolar disorder is highly heritable even though most adults with bipolar illness do not have a family history of bipolar illness among their first-degree relatives. She shared estimates that if one parent has bipolar disorder their offspring have a 5% lifetime risk of developing bipolar disorder. If both parents have bipolar disorder their offspring have a 25% risk of developing bipolar disorder and a 35% incidence of developing any affective disorder (although other data by Lapalme et al. suggest it may be as high as 60%).
Duffy found that when parents responded well to lithium, their children tended to do the same. Lithium-responsive patients tended to be those without anxiety disorder and substance abuse and who had classic bipolar episodes and clear well intervals between episodes. Read more
Long Delays to First Treatment Are Crippling Many with Bipolar Disorder: What You Can Do
An article published by N. Drancourt et al. in the journal Acta Psychiatra Scandinavica this year examined the duration of the period between a first mood episode and treatment with a mood stabilizer among 501 patients with bipolar disorder. The time between a first episode of depression, mania, or hypomania and first treatment averaged 9.7 years. The authors conclude that more screening, better recognition of the early stages of the illness, and greater awareness are needed to decrease this long delay.
Editor’s Note: The article by Dancourt et al. replicates earlier findings of an average treatment delay of 10 years among bipolar patients from the treatment network in which this editor (Robert Post) is an investigator (formerly the Stanley Foundation Bipolar Network, now called the Bipolar Collaborative Network). The duration of the untreated interval (DUP) for patients with bipolar disorder is unacceptably long and carries a heavy price.
Those with the earliest age of onset experience the longest delay to first treatment. Early onset is associated with poor outcome compared to adult onset bipolar disorder, and the duration of time untreated adds a separate, independent risk of a worse outcome in adulthood, especially more frequent and severe depression, more episodes, and less time well.
What patients and doctors can do to shorten this interval to first treatment: Know the risk factors for early onset bipolar disorder so you can seek evaluation and advise treatment as appropriate. Read more
Genetic Basis for Childhood Onset of Bipolar Illness
 Eric Mick of Massachusetts General Hospital reviewed the latest genetics data on bipolar disorder and reported at the 57th Annual Meeting of the American Academy of Child and Adolescent Psychiatry that 20% of people with childhood-onset bipolar illness have a first-degree relative with bipolar disorder, while only 10% of those with adult-onset bipolar disorder have a first-degree relative with bipolar disorder. These data are consistent with others that indicate that there is an increased genetic/familial risk for bipolar disorder in childhood- compared with adult-onset illness.
Eric Mick of Massachusetts General Hospital reviewed the latest genetics data on bipolar disorder and reported at the 57th Annual Meeting of the American Academy of Child and Adolescent Psychiatry that 20% of people with childhood-onset bipolar illness have a first-degree relative with bipolar disorder, while only 10% of those with adult-onset bipolar disorder have a first-degree relative with bipolar disorder. These data are consistent with others that indicate that there is an increased genetic/familial risk for bipolar disorder in childhood- compared with adult-onset illness.
Mick reviewed a number of findings that suggest that alterations in genes involved in intracellular signaling and in the development and maintenance of long-term memory may also be implicated in bipolar disorder. Classical genome-wide association studies (GWAS), in which a link between any human gene and bipolar disorder is sought, have not found any genes with a large effect or a high predictive value for bipolar illness. In the meantime, other strategies for finding genetic links to bipolar disorder are being pursued, including studying rare gene variants. There is some evidence that these variants occur more frequently in children with early onset bipolar illness.
Bipolar Disorder Worse in US than Europe
New research shows that there are more early onsets of illness and more difficult courses of bipolar illness in the US than in the Netherlands or Germany.
This editor was invited to give a plenary presentation at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. The talk, titled “A greater incidence of early onset bipolar illness and poor prognosis factors in patients in the US compared with those in The Netherlands and Germany,” was based on studies in our Bipolar Collaborative Network.
We found that patients who were studied and treated at four sites in the US (Los Angeles, Dallas, Cincinnati, and Bethesda) had more poor-prognosis factors and indices of difficult courses of bipolar illness compared with patients studied in the same fashion at three sites in Utrecht, the Netherlands and Freiberg and Munich, Germany. We presented some of these data in a preliminary report in the British Journal of Psychiatry in 2008 and further analyzed these data for an article published last year in the Journal of Clinical Psychiatry. Read more