Antipsychotic Use During Pregnancy Most Likely Safe
A new study suggests that women can continue using antipsychotic medications during the first trimester of pregnancy without meaningfully increasing the risk of birth defects in their offspring.
The study, by Krista F. Huybrechts and colleagues in the journal JAMA Psychiatry, looked at Medicaid users who filled at least one prescription for an antipsychotic medication during their first trimester of pregnancy, when an embryo’s vital organs are formed, and went on to have a live birth. Birth defects, including cardiac malformations, in these children were identified in the first 90 days after delivery and compared to the number of such abnormalities in the children of women on Medicaid who did not receive a prescription for an antipsychotic drug during the first trimester of pregnancy. The number of abnormalities was slightly higher in the children of women who had received atypical antipsychotics than in those who had not, and slightly lower in the children of women who had received a typical antipsychotic than in those who had not.
Huybrechts and colleagues concluded that taking an antipsychotic medication during the first trimester of pregnancy does not meaningfully increase the risk of birth defects in the offspring.
The children of women who took the antipsychotic risperidone did have a small increased risk of birth defects, including cardiac malformations. The researchers called for additional study of risperidone use during pregnancy.
Study Shows FDA Drug Safety Warning on Citalopram Backfired
In August 2011, the US Food and Drug Administration issued a warning that doses of the selective serotonin reuptake inhibitor (SSRI) antidepressant citalopram (Celexa) that exceeded 40mg/day could prolong the QT interval, a measure of heart rate used to diagnose abnormal heart rhythms. A study of records from the Veterans Health Administration showed that 35,848 veterans whose dose of citalopram was reduced from an average of 64mg/day to under 40mg/day faced increased deaths, hospitalizations for any cause, and hospitalizations for depression specifically after the reductions.
The FDA warning meant to prevent heart problems had the unintended consequence of increasing hospitalizations and deaths among the veterans affected. These findings by Thomas S. Rector and colleagues were published in the American Journal of Psychiatry in 2016.
Editor’s Note: There are some similarities between this case and findings by researchers Andrew Nierenberg and Andrew Stoll, who noticed that patients taking 40mg/day of fluoxetine (Prozac) had better long-term outcomes than those taking 20mg/day, even though those taking 40mg were more ill and more likely to relapse at the start of the study.
Researchers Ellen Frank and David Kupfer found that 90% of unipolar depressed patients relapsed when their antidepressant doses were halved, even though they had been stable for 5 years before the change.
These and the findings from Rector and colleagues lead this editor to believe that reducing the dosage of effective treatments should not be done without reason—that is, in the absence of side effects, or simply to achieve the minimal effective dose. Dose reductions without cause not only may increase the risk of relapse, but may also put the patient at increased risk of developing tolerance to the medication, for example hastening the onset of ‘Prozac poop-out.’
When long-term maintenance drug therapy is going well, it may be best to be conservative and stay the course. Conversely, in the absence of a good long-term response, be as active and creative as possible to achieve mood stabilization.
Mouse Study Shows That Ketamine Metabolite May Treat Depression with Fewer Side Effects
The drug ketamine has been used intravenously for years to rapidly treat depression, because it can take effect within hours. Unfortunately, its antidepressant effects fade in 3–5 days, and it has some unpleasant side effects. In larger doses ketamine is used as an anesthetic and sometimes as a club drug, for its ability to induce hallucinations and dissociation. It can be addictive as well.
A 2016 animal study by Todd Gould and colleagues published in the journal Nature identified a byproduct of ketamine that may be able to provide the drug’s benefits without its side effects.
When the body breaks down ketamine, it produces several chemicals that are known as ketamine metabolites. The researchers found that one of these, called hydroxynorketamine, reversed a depression-like state in mice, without producing the side effects that would be expected of ketamine.
Gould and colleagues also determined that blocking the transformation of ketamine into hydroxynorketamine prevented ketamine’s antidepressant effects.
Ketamine’s unpleasant anesthetic and dissociative effects result from the blockade of a particular receptor for the neurotransmitter glutamate (the NMDA glutamate receptor). Researchers originally thought that the NMDA blockade was linked to ketamine’s antidepressant effects, but this appears not to be the case. Instead, hydroxynorketamine seems to activate a different type of glutamate receptor, the AMPA receptor.
Gould and colleagues plan to test hydroxynorketamine in humans soon. Because it has already been present in the human body following ketamine administration, they expect it to be safe.
Multiple Risks of Benzodiazepine Use
Benzodiazepines are a class of drugs that became widely used in the 1970s for their ability to reduce panic, anxiety, and insomnia. Some also functioned as anticonvulsants, reducing seizures. They are considered “downers,” with sedating qualities.
New research shows that benzodiazepine use, particularly long-term use, comes with risks such as increased mortality and mood instability.
At a 2015 scientific meeting, researcher Jari Tiihonen reported that among 21,492 patients with schizophrenia in Sweden, benzodiazepine use was associated with increased mortality, while antidepressant and antipsychotic use decreased mortality.
At the same meeting, researcher Cristina Albott reported that benzodiazepines may interfere with the rapid onset of antidepressant effects usually brought about by intravenous treatment with the drug ketamine.
In 2010, researcher Roy Perlis reported in the Journal of Clinical Psychiatry that in STEP-BD, a large study of people with bipolar disorder, benzodiazepine use was associated with an increased risk of recurrence of mood episodes.
Editor’s Note: Benzodiazepines can also exacerbate symptoms of post-traumatic stress disorder (PTSD) and regular use can lead to a decrease in lifespan. It now seems as though there are many reasons to exercise caution in the use of these drugs.
Clarifying the Effects of a Diabetes Drug that Improves Bipolar Depression
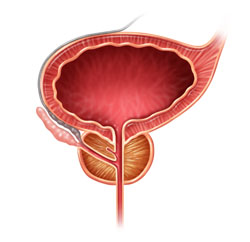
Research continues on pioglitazone, a drug typically used to treat diabetes but with other positive effects on depression and stroke risk. Some researchers are working on determining whether the drug increases the risk of developing certain cancers, including bladder, prostate, and pancreatic cancers. A recent study by James D. Lewis and colleagues in the journal JAMA found no statistically significant increase in risk of bladder cancer among patients taking the drug, but the researchers said they also couldn’t rule out that the drug may increase this risk, as has been seen in previous studies. The study by Lewis did show an increase in pancreatic and prostate cancers in patients taking pioglitazone, but the researchers did not determine whether this was caused by the drug.
Another recent study by Walter N. Kernan and colleagues in the New England Journal of Medicine reported that pioglitazone reduced the incidence of stroke and heart attack in patients with a history of stroke or blocked blood vessels in the brain but without a diagnosis of diabetes. Patients who received pioglitazone also experienced side effects including weight gain, edema (an increase in fluids in the body’s tissues) and serious bone fractures.
Pioglitazone has had positive effects in bipolar depression and may one day be used as a treatment for bipolar disorder. For now, it may be worthy of consideration for the treatment of diabetes in patients who also have bipolar depression.
Children at Risk for Bipolar Disorder May Have Adverse Reactions to Antidepressants
 At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Jeffrey R. Strawn reported that among children at high risk for bipolar disorder (because of a family history of the disorder) who are prescribed antidepressants for depression and anxiety, adverse reactions are common. These reactions include irritability, aggression, impulsivity, and hyperactivity, and often lead to discontinuation of the antidepressant treatment.
At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Jeffrey R. Strawn reported that among children at high risk for bipolar disorder (because of a family history of the disorder) who are prescribed antidepressants for depression and anxiety, adverse reactions are common. These reactions include irritability, aggression, impulsivity, and hyperactivity, and often lead to discontinuation of the antidepressant treatment.
Younger patients at risk for bipolar disorder were more likely to have an adverse reaction to antidepressants. Risk of an adverse reaction decreased 27% with each year of age.
Lithium Has Minimal Effects On Renal Function: Results Of Two New Large Controlled Studies
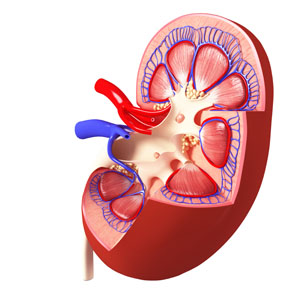 Earlier this year we described a 2015 study by Harald Aiff and colleagues that suggested that long-term lithium use was associated with a risk of kidney failure. That study, published in the Journal of Psychopharmacology, included 630 patients who had taken lithium for at least 10 years. One-third of these patients had evidence of kidney dysfunction, and in 5%, the impairment was severe. Two new studies provide some data that suggest these risks may not be lithium-specific and are comparable to risks that come with taking other medications.
Earlier this year we described a 2015 study by Harald Aiff and colleagues that suggested that long-term lithium use was associated with a risk of kidney failure. That study, published in the Journal of Psychopharmacology, included 630 patients who had taken lithium for at least 10 years. One-third of these patients had evidence of kidney dysfunction, and in 5%, the impairment was severe. Two new studies provide some data that suggest these risks may not be lithium-specific and are comparable to risks that come with taking other medications.
The first, by Stefan Clos et al. in The Lancet Psychiatry, included 1,120 patients followed for up to 12 years. On average, these patients had been exposed to lithium for a little over 4.5 years. Clos and colleagues determined patients’ estimated glomerular filtration rate (eGFR), a measure of how well the blood is filtered by the kidneys. The researchers concluded that there was “no effect of stable lithium maintenance therapy on the rate of change of eGFR over time” compared to other drugs such as quetiapine, olanzapine, or valproate.
The second new study, by Lars Vedel Kessing and colleagues in the journal JAMA Psychiatry, included 26,731 patients exposed to lithium and 420,959 exposed to anticonvulsants. Kessing and colleagues concluded that both exposure to lithium and exposure to an anticonvulsant were associated with an increased rate of chronic kidney disease, but lithium was not associated with end-stage kidney disease (the kind that requires dialysis or renal transplantation).
The three studies taken together suggest the following: Taking lithium for an average of 4–5 years does not affect kidney functioning, and longer exposure may not harm kidney function any more than other medications (such as anticonvulsants) would. However, kidney functioning (in terms of eGFR) does decline with age, and is also lower among those with higher baseline eGRF, those with other illnesses, those taking other drugs that affect the kidneys, and those who experience an episode of lithium toxicity. Read more
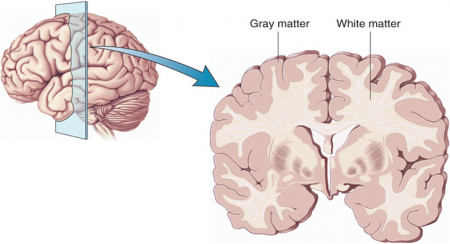
Atypical Antipsychotics May Slow Loss of Gray Matter in Schizophrenia
Progressive losses in gray matter have been observed in the cortex of people with schizophrenia, and those at high risk for the illness. In the past, studies have shown that the amount of antipsychotics a patient is exposed to is correlated with the extent of their deficits in gray matter, suggesting that antipsychotic treatment could exacerbate gray matter loss.
A new meta-analysis by Antotonio Vita and colleagues in the journal Biological Psychiatry shows that first-generation antipsychotics were associated with greater losses in gray matter compared with atypical antipsychotics, which seemed to slow the loss of gray matter.
The meta-analysis analyzed data from 18 longitudinal studies comparing a total of 1155 patients with schizophrenia to 911 healthy control participants. Magnetic resonance imaging (MRI) scans showed that over time, patients with schizophrenia lost more cortical gray matter volume. The patients’ cumulative intake of any kind of antipsychotic between MRI scans was associated with gray matter losses. But when Vita and colleagues drilled down to find differences between patients taking first-generation antipsychotics and those taking second-generation atypical antipsychotics, they found that patients with higher average daily intake of first-generation antipsychotics had greater losses in gray matter, while patients with higher average daily intake of atypical antipsychotics had less progressive losses in gray matter.
This study is the first to compare the effects of first-generation antipsychotics, which were developed in the 1960s, with those of atypical antipsychotics, which came into frequent use in the late 1980s, on cortical gray matter loss in schizophrenia. While first-generation antipsychotics are associated with the side effect of tardive dyskinesia, involuntary movements of the face and jaw, atypical antipsychotics are most commonly associated with weight gain.
Three studies have randomly assigned patients with schizophrenia to receive either first-generation or atypical antipsychotics. In these studies as well, second-generation antipsychotics were associated with smaller losses in gray matter.
The authors speculate that either second-generation antipsychotics may have neuroprotective effects, or first-generation antipsychotics may have neurotoxic effects. They also suggest that first-generation antipsychotics may not have the capacity to interfere with the natural progression of schizophrenia in terms of gray matter losses.
Future studies may investigate differences between specific antipsychotic medications’ effects on gray matter volume. Vita and colleagues reported that in the analysis, the atypical antipsychotic clozapine was associated with the least loss of gray matter of any medication in the included studies.
Editor’s Note: This study is important because it adds to findings questioning the conclusions of a large National Institute of Mental Health–sponsored study known as CATIE and a meta-analysis by John Geddes published in the journal BMJ in 2000, in which he wrote that “There is no clear evidence that atypical antipsychotics are more effective or better tolerated than conventional (first generation) antipsychotics.” Read more
Clozapine-Induced Myocarditis More Common Than Thought
 New research indicates that myocarditis, inflammation of the middle layer of the heart wall, occurs in about 3% of patients who begin taking clozapine (Clozaril). Researcher Kathlyn J. Ronaldson and colleagues recently published research to this effect in the journal Acta Psychiatrica Scandinavica. Many cases of myocarditis, which can be fatal, begin with fever. Other symptoms include rapid or abnormal heart rhythms, shortness of breath, fluid retention, and fatigue. Because the illness resembles a viral infection, it may be misdiagnosed.
New research indicates that myocarditis, inflammation of the middle layer of the heart wall, occurs in about 3% of patients who begin taking clozapine (Clozaril). Researcher Kathlyn J. Ronaldson and colleagues recently published research to this effect in the journal Acta Psychiatrica Scandinavica. Many cases of myocarditis, which can be fatal, begin with fever. Other symptoms include rapid or abnormal heart rhythms, shortness of breath, fluid retention, and fatigue. Because the illness resembles a viral infection, it may be misdiagnosed.
In 2010 Ronaldson and colleagues reported in the Journal of Clinical Psychiatry that tachycardia (rapid resting heart rate) and elevated levels of a group of proteins knows as troponin in the blood are almost always present during the first 45 days of treatment in patients who develop myocarditis. The researchers found that the time to onset of myocarditis was 14 to 22 days in almost all cases. Eosinophilia (high levels of a certain type of white blood cell) may occur in the week after peak troponin levels, and high levels of the inflammatory protein CRP (above 100mg/L) occurred in 79% of cases.
Ronaldson and colleagues suggest that patients who are prescribed clozapine be monitored for myocarditis during the first four weeks of treatment, particularly during the third week.
Long-Term Lithium Treatment Has Risks for Kidney Function, Even with Precautions
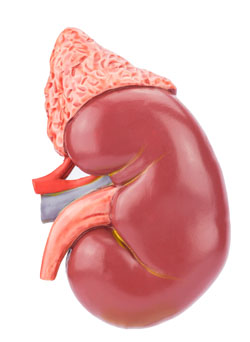 Long-term lithium use has long been associated with decreased renal function. But some Swedish researchers noticed that most long-term studies of patients with renal failure had begun in the 1960s and 1970s. In the 1980s, when it became clear that lithium could reduce renal function, doctors began to institute new safety measures for lithium users, including monitoring of blood levels of the drug and of creatinine, a substance that is excreted by the kidneys as part of normal muscle metabolism. So the researchers undertook a new study to examine whether the protocols instituted in the 1980s had reduced the renal risks of long-term lithium use. Unfortunately, they found that some reduced renal function is still common among people who use lithium for longer than 10 years, and this risk does not necessarily decrease when patients stop taking lithium.
Long-term lithium use has long been associated with decreased renal function. But some Swedish researchers noticed that most long-term studies of patients with renal failure had begun in the 1960s and 1970s. In the 1980s, when it became clear that lithium could reduce renal function, doctors began to institute new safety measures for lithium users, including monitoring of blood levels of the drug and of creatinine, a substance that is excreted by the kidneys as part of normal muscle metabolism. So the researchers undertook a new study to examine whether the protocols instituted in the 1980s had reduced the renal risks of long-term lithium use. Unfortunately, they found that some reduced renal function is still common among people who use lithium for longer than 10 years, and this risk does not necessarily decrease when patients stop taking lithium.
The researchers, led by Harald Aiff, published the study in the Journal of Psychopharmacology in 2015. They identified 4,879 patients who had been prescribed lithium, and narrowed this list down to 630 adult patients who had taken lithium for at least 10 cumulative years, who had normal levels of creatinine when they began taking lithium, and on whom good data existed. About one-third of these patients had evidence of chronic renal impairment, and in 5% of these the impairment was severe or very severe.
Aiff and colleagues’ findings show that lithium treatment requires careful monitoring, especially over the long term. Patients must consider the risk/benefit ratio of lithium treatment. Since prevention of mood episodes can preserve an average ten years of life expectancy, and lithium has the best data for efficacy in preventing manic and depressive episodes, patients must weigh the risks of insufficiently treated bipolar illness against the possibility for long-term decreases in kidney function.