Lithium Lengthens Telomeres
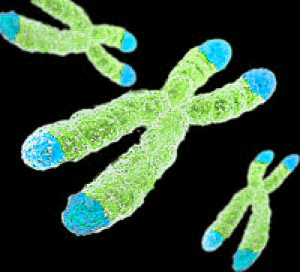 Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect the DNA as it is replicated. Depressive episodes and age can reduce the length of telomeres. Lithium treatment increases telomere length. At the 2016 meeting of the Society of Biological Psychiatry, researcher Martin Schalling reported that the longer a patient takes lithium, the more their telomere length increases.
Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect the DNA as it is replicated. Depressive episodes and age can reduce the length of telomeres. Lithium treatment increases telomere length. At the 2016 meeting of the Society of Biological Psychiatry, researcher Martin Schalling reported that the longer a patient takes lithium, the more their telomere length increases.
According to Schalling, people who respond well to lithium treatment show greater increases in telomere length than those who respond poorly to lithium.
While some cancers are associated with long telomeres, lithium use has not been found to increase cancer risk. In fact, lithium treatment can decrease the risk of certain cancers of the gastrointestinal, respiratory, and endocrine systems.
Meta-Analysis Shows Anti-Inflammatory Treatments Improve Bipolar Depression
 It has been clear for some time that depression and inflammation are linked. This has led researchers to explore a variety of anti-inflammatory agents to treat depression. A meta-analysis of studies examining anti-inflammatory treatments for bipolar depression was published in the journal Bipolar Disorders in 2016.
It has been clear for some time that depression and inflammation are linked. This has led researchers to explore a variety of anti-inflammatory agents to treat depression. A meta-analysis of studies examining anti-inflammatory treatments for bipolar depression was published in the journal Bipolar Disorders in 2016.
Researcher Joshua D. Rosenblat and colleagues identified eight randomized controlled trials that met their criteria for anti-inflammatory treatments of bipolar disorder. These treatments included nonsteroidal anti-inflammatory drugs (NSAIDs such as ibuprofen and aspirin), omega-3 fatty acids, the antioxidant N-acetylcysteine, and pioglitazone (used to treat diabetes). Overall, the anti-inflammatory treatments had a moderate and statistically significant antidepressant effects. No serious side effects were reported, and the anti-inflammatory treatments did not cause a switch into mania in any of the participants.
The diversity of the anti-inflammatory treatments reviewed in this meta-analysis limit the extent to which it can be interpreted, but it is clear that more research on anti-inflammatory treatments for bipolar depression is needed. An open question is whether patients with particularly elevated levels of inflammatory markers in their blood would respond better to these anti-inflammatory treatments.
Galantamine Did Not Improve Cognitive Deficits in People with Bipolar Disorder
In a recent study by researcher Dan V. Iosifescu and colleagues, the drug galantamine, which is used to treat dementia, did not improve cognitive function in euthymic people with bipolar disorder. The drug had done so in earlier studies. Seventy-two participants with bipolar disorder that was in remission were randomized to receive either a placebo or galantamine extended release for a period of two weeks. Doses of galantamine ranged from 8 to 24 mg/day.
The participants took several tests of attention and memory over the course of the study. After 16 weeks of treatment, those taking galantamine did not show significant improvements in functioning compared to those who received placebo.
This research was presented at the 2016 meeting of the Society of Biological Psychiatry.
Inflammation Linked to Non-Response to Antidepressants
In a symposium on inflammation’s role in psychiatric disorders at the 2016 meeting of the Society of Biological Psychiatry, researcher Carmine Pariante reviewed the considerable literature indicating that major depression is often associated with measures of inflammation. Depression has been linked to elevated blood levels of the inflammatory proteins interleukin-1, interleukin-6, TNF alpha, and c-reactive protein, with about one-third of depressed patients having an elevated level of at least one of these proteins. People with elevated inflammatory markers are also less likely to respond to traditional antidepressants such as selective serotonin reuptake inhibitors (SSRIs).
Pariante reported that in depressed people, interleukin-6 is also elevated in cerebrospinal fluid in addition to blood, suggesting that inflammation in depression extends to the central nervous system. Increased secretion of interleukin-6 has been linked to depressive behaviors in mice exposed to stress.
There is some hope that anti-inflammatory treatments can help patients who do not respond to traditional antidepressant treatment. Some anti-inflammatory medications that may eventually be used to treat depression with inflammation include the COX-1 inhibitor aspirin, the COX-2 inhibitor celecoxib (Celebrex), or the antibiotic minocycline. Each of these approaches gained some support in preliminary clinical trials, but it has not yet been established that these anti-inflammatory treatments produce a better response in people with elevated inflammatory markers.
Mindfulness-Based Cognitive Therapy May Improve Depression More Than Fitness Intervention
In a study by researcher Stuart Eisendrath and colleagues, people with treatment-resistant unipolar depression responded better to an intervention that combined mindfulness training with cognitive therapy than to one that included exercise, nutrition counseling, and music therapy.
The 173 participants had failed to respond to at least two different antidepressant medications. During the study period, all participants were taking an antidepressant, but none were receiving other types of therapy.
After eight weeks, the mindfulness-based cognitive therapy (MBCT) group showed greater improvement in their depression symptoms than the exercise and nutrition group. Of the MBCT group, 29.58% had a large reduction in symptoms, while 17.19% of the comparison group showed a similarly large reduction in symptoms.
A subgroup of the participants also received functional magnetic resonance imaging (fMRI) as part of the study. While completing a task related to emotional working memory, the MBCT group showed enhanced activation of the dorsal lateral prefrontal cortex (to levels seen in non-depressed people). This area is related to executive control of depression and memory functions. The MBCT group also showed reduced activation of the ventral lateral prefrontal cortex compared to the comparison group. Members of the MBCT whose depression symptoms had improved also showed better regulation of the amygdala during the task compared to the exercise and nutrition group.
The research was presented at the 2016 meeting of the American Psychiatric Association.
SSRI Use During Pregnancy Linked to Adolescent Depression in Offspring
A 2016 article by Heli Malm and colleagues in the Journal of the American Academy of Child and Adolescent Psychiatry suggests that in utero exposure to selective serotonin reuptake inhibitor (SSRI) antidepressants may increase the risk of depression in adolescence. However, the study included potentially confounding factors. It is possible that women who took SSRIs during pregnancy had more severe depression than those who went unmedicated during pregnancy. The mothers in the study who took SSRIs also had more comorbid conditions such as substance abuse.
Editor’s Note: Women should balance the risks and benefits of antidepressant use during pregnancy, since depression itself can have adverse effects on both mother and fetus. It has recently been established that SSRI use during pregnancy does not cause birth defects, so women with depression that has not responded to non-pharmaceutical interventions such as psychotherapy, omega-3 fatty acid supplementation, exercise, mindfulness, and repeated transcranial magnetic stimulation (rTMS) may still want to consider SSRIs.
Antipsychotic Use During Pregnancy Most Likely Safe
A new study suggests that women can continue using antipsychotic medications during the first trimester of pregnancy without meaningfully increasing the risk of birth defects in their offspring.
The study, by Krista F. Huybrechts and colleagues in the journal JAMA Psychiatry, looked at Medicaid users who filled at least one prescription for an antipsychotic medication during their first trimester of pregnancy, when an embryo’s vital organs are formed, and went on to have a live birth. Birth defects, including cardiac malformations, in these children were identified in the first 90 days after delivery and compared to the number of such abnormalities in the children of women on Medicaid who did not receive a prescription for an antipsychotic drug during the first trimester of pregnancy. The number of abnormalities was slightly higher in the children of women who had received atypical antipsychotics than in those who had not, and slightly lower in the children of women who had received a typical antipsychotic than in those who had not.
Huybrechts and colleagues concluded that taking an antipsychotic medication during the first trimester of pregnancy does not meaningfully increase the risk of birth defects in the offspring.
The children of women who took the antipsychotic risperidone did have a small increased risk of birth defects, including cardiac malformations. The researchers called for additional study of risperidone use during pregnancy.
Study Shows FDA Drug Safety Warning on Citalopram Backfired
In August 2011, the US Food and Drug Administration issued a warning that doses of the selective serotonin reuptake inhibitor (SSRI) antidepressant citalopram (Celexa) that exceeded 40mg/day could prolong the QT interval, a measure of heart rate used to diagnose abnormal heart rhythms. A study of records from the Veterans Health Administration showed that 35,848 veterans whose dose of citalopram was reduced from an average of 64mg/day to under 40mg/day faced increased deaths, hospitalizations for any cause, and hospitalizations for depression specifically after the reductions.
The FDA warning meant to prevent heart problems had the unintended consequence of increasing hospitalizations and deaths among the veterans affected. These findings by Thomas S. Rector and colleagues were published in the American Journal of Psychiatry in 2016.
Editor’s Note: There are some similarities between this case and findings by researchers Andrew Nierenberg and Andrew Stoll, who noticed that patients taking 40mg/day of fluoxetine (Prozac) had better long-term outcomes than those taking 20mg/day, even though those taking 40mg were more ill and more likely to relapse at the start of the study.
Researchers Ellen Frank and David Kupfer found that 90% of unipolar depressed patients relapsed when their antidepressant doses were halved, even though they had been stable for 5 years before the change.
These and the findings from Rector and colleagues lead this editor to believe that reducing the dosage of effective treatments should not be done without reason—that is, in the absence of side effects, or simply to achieve the minimal effective dose. Dose reductions without cause not only may increase the risk of relapse, but may also put the patient at increased risk of developing tolerance to the medication, for example hastening the onset of ‘Prozac poop-out.’
When long-term maintenance drug therapy is going well, it may be best to be conservative and stay the course. Conversely, in the absence of a good long-term response, be as active and creative as possible to achieve mood stabilization.
Antidepressant Brintellix Renamed Trintellix
You may notice the label on your prescription bottle changing. As of June, the antidepressant vortioxetine (formerly Brintellix) is now called Trintellix. The US Food and Drug Administration approved the change to reduce any possible confusion of the antidepressant with a blood-thinning medication called Brilinta.
Weight Gain is a Common Issue with Antidepressants, But Buproprion is an Exception
A 2016 study by researcher David Arterburn and colleagues in the Journal of Clinical Medicine suggests that taking an antidepressant for two years is associated with an increase in body weight. Luckily, bupropion (trade name Wellbutrin) is an exception that may be a good choice for obese or overweight patients.
The researchers analyzed links between which antidepressants patients in a large health system in Washington State were prescribed and their body weight two years later.
The researchers used fluoxetine (Prozac) as a reference. Most antidepressants did not differ significantly from fluoxetine in terms of the weight gain experienced by people taking the drug.
There were a few exceptions. Compared to non-smoking fluoxetine users, who gained an average of 4.6 pounds in two years, non-smoking bupropion users actually lost weight—an average of 2.4 pounds. (Smokers taking bupropion still gained an average of 6.9 pounds.)
Sertraline (Zoloft) was another exception. Sertraline users gained more than users of other antidepressants—an average of 10.5 pounds over two years.