Faster, Better Response to Risperidone than Valproate in Adolescents with Bipolar Disorder
An article by Pavuluri et al. published in Bipolar Disorders in September reported that both divalproex sodium (valproate, or Depakote) and risperidone (Risperdol) were effective in youth with bipolar disorder, but improvements appeared more quickly with risperidone. Risperidone also produced higher response rates, higher remission rates, and fewer dropouts from side effects.
A presentation by the research group at an earlier conference suggested that it was particularly among those with comorbid disruptive behavioral disorders (DBD), which include attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), and conduct disorder (CD), that risperidone worked faster and produced greater early results than divalproex.
 In the study, 66 children with type I bipolar disorder and a mean age of 11 years were assessed. Treatment with risperidone was initiated at 0.5 mg/day and titrated to 2 mg, while divalproex was initiated at 60 micrograms/mL and titrated up to 120 micrograms.
In the study, 66 children with type I bipolar disorder and a mean age of 11 years were assessed. Treatment with risperidone was initiated at 0.5 mg/day and titrated to 2 mg, while divalproex was initiated at 60 micrograms/mL and titrated up to 120 micrograms.
Editor’s Note: The possibility that children with different comorbid disorders respond differently to different antimanic agents suggests that more studies are needed to determine which subgroups of patients are most responsive to typical treatments.
Inflammation and Oxidative Stress in Bipolar Disorder
A number of studies presented at the 4th Biennial Conference of the International Society for Bipolar Disorders conference in Sao Paulo, Brazil in March reported new data relevant to inflammation and oxidative stress. Both inflammation and oxidative stress increase risk of cardiovascular disorders, and patients with inadequately treated mood disorders lose 10 or more years of life expectancy from cardiovascular disorders compared to the general population. Inflammation and oxidative stress may also contribute to the symptoms, evolution, and progression of the mood disorders themselves.
It is possible that these two processes could become new targets for therapeutic intervention in addition to more traditional psychopharmacological drugs that primarily target the neurotransmitters dopamine, norepinephrine, serotonin, and the neurotrophic factor BDNF. Read more
Preventing Recurrent Mood Episodes
Psychotherapy and psychoeducational approaches, long-term psychopharmacology, and combination therapy all play a role in preventing recurrent mood episodes.
Psychotherapeutic and Psychoeducational Approaches Are Critical
A number of studies presented at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March indicated that cognitive-behavioral therapy (CBT) and individual and group psychoeducational approaches enhance both short- and long-term outcomes for patients with bipolar illness. These studies add to an already substantial literature that shows that focused psychotherapies (such as cognitive/behavioral, interpersonal, and social rhythms therapies) and psychoeducation are superior to treatment as usual.
These therapies can provide a variety of approaches to stress management and reduction, and can enhance family and interpersonal communication. Another way these focused psychotherapeutic approaches help patients is by demonstrating the benefits of effective long-term preventive treatment and encouraging its consistent use.
Without consistent prophylactic treatment, patients are at high risk for recurrences and their subsequent psychosocial and neurobiological consequences. Greater number of prior episodes is associated with an increased risk of psychosocial dysfunction, treatment resistance, cognitive dysfunction, medical comorbidities, and even dementia in old age.
After the jump: preventive psychopharmacology and combination therapy. Read more
Thyroid Augmentation Helps Depression (And Bipolar Disorder in Women)
Low dose thyroid replacement treatment with T3 (Cytomel) (25-37.5 µg) is typically recommended for acute antidepressant augmentation in unipolar and bipolar depression. This approach has few side effects and works even in those with normal thyroid function at baseline.
Some data also supports the use of relatively high (supraphysiological) doses of T4 (Synthroid) late in the treatment of highly treatment-resistant patients with unipolar and bipolar disorder. These supra-physiological doses of T4 typically ranged from 300-500 µg/day, producing a free thyroxine index of 150% of normal. This is usually moderately well tolerated, although minor degrees of sweating, tachycardia (fast heartbeat), and other signs of hyperthyroidism can accompany this regimen. If this approach is employed, it is particularly important to increase the dose of T4 (Synthroid) very slowly because of its relatively long half-life—about 12 days. (That is, if a patient takes a high dose of T4 and then stops their medication completely, 12 days later blood levels will only have decreased to half of what they originally were.)
Findings about high-dose T4 for women with treatment-resistant bipolar illness after the jump. Read more
Smoking Multiplies Risks for Bipolar Patients
Smoking is associated with a less successful outcome in the naturalistic treatment of bipolar patients, reported Seetal Dodd and colleagues at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. Nicotine dependence has also been found to be a risk factor for depressive symptoms, as reported in a recent article in the British Journal of Psychiatry.
In addition to these direct effects on mental health, smoking is also a major risk factor for cardiovascular disease when combined with the presence of any three of the five primary risk factors that constitute the metabolic syndrome. (These five factors are: increased waist circumference, high blood pressure, increased cholesterol, increased triglycerides, and insulin resistance or elevated fasting blood glucose.) Cardiovascular disease co-occurs with bipolar disorder at a high rate and is one of the major causes of decreased life expectancy in those with inadequately treated illness.
Because smoking is a powerful risk factor for comorbid illnesses such as heart attack and stroke and is itself associated with a poor clinical outcome in the treatment of bipolar disorder, every effort should be made to help patients with smoking cessation. Suggestions after the jump. Read more
Dialectical Behavior Therapy Effective for Adolescents with Bipolar Disorder
As we posted yesterday, therapeutic approaches appear necessary for childhood-onset bipolar disorder. In a poster at the Pediatric Bipolar Conference in Cambridge, Massachusetts in March, Tina Goldstein of Western Psychiatric Institute in Pittsburgh presented an open study indicating that dialectical behavior therapy (DBT) was effective for adolescents with bipolar disorder. This is the second study that has produced these results. In DBT, patients are taught coping skills and mindfulness in order to break the cycle of responding to dysregulated emotions with problematic behaviors.
Psychotherapy Necessary for Bipolar Disorder and Severe Mood Dysregulation in Children
 Dr. Janet Wozniak of Massachusetts General Hospital initiated a survey, both at MGH and in the field, to ascertain practitioners’ experience with individual and family psychotherapeutic and educational approaches to childhood-onset bipolar illness. These types of approaches appear fundamental to treating children or families in which there is bipolar illness.
Dr. Janet Wozniak of Massachusetts General Hospital initiated a survey, both at MGH and in the field, to ascertain practitioners’ experience with individual and family psychotherapeutic and educational approaches to childhood-onset bipolar illness. These types of approaches appear fundamental to treating children or families in which there is bipolar illness.
It was the view of Wozniak, her survey, and many other investigators in attendance at the Pediatric Bipolar Conference in Cambridge, Massachusetts in March that such psychotherapeutic approaches are needed, and often recommended, but the availability of effective treatment and of therapists skilled in administering any of these psychotherapies in children is often lacking.
One Expert’s Personal Treatment Algorithm for Bipolar Disorder in Young Children
EDITOR’S NOTE: Dr. Gagin Joshi of Massachusetts General Hospital, who presented the work on carbamazepine and lamotrigine on page 1 provided us with his own general treatment algorithm for youngsters with bipolar disorder.

Omega-3 Fatty Acids (photo from ironmagazine.com)
Joshi typically starts with 0.5 to 2 gms of omega-3 fatty acids because of their benign side-effects profile, the many studies suggesting they are effective in adult mood disorders, and a recent article indicating that they were effective in preventing the conversion of prodromal schizophrenia into full-blown illness in a randomized double-blind controlled study in Australia.
After the omega-3 fatty acids, Joshi’s second choice is typically the atypical antipsychotic aripiprazole (Abilify) because of its lesser degree of weight gain compared to atypicals quetiapine (Seroquel) or risperidone (Risperidol). Risperidone can be a third option if aripiprazole is not effective or tolerated.
Brain Stimulation for Treatment-Resistant Depression
There are many methods of stimulating the brain directly, ranging from the very invasive to the non-invasive. Below we discuss deep brain stimulation, frontal lobe and vagal nerve stimulation, repeated transcranial magnetic stimulation, electroconvulstive therapy (in particular the new right unilateral ultra-brief pulse method), and low level magnetic fields.
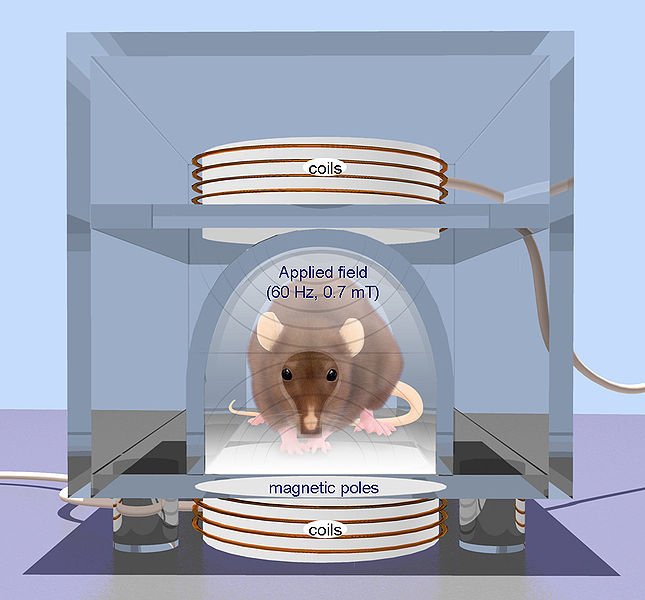
- Repetitive transcranial magnetic stimulation (rTMS) is a technique for noninvasive stimulation of the adult brain. Stimulation is produced by generating a brief, high-intensity magnetic field by passing a brief electric current through a magnetic coil. Compared with the growing number of clinical trial with rTMS, there are surprisingly few animal studies on its basic mechanisms of action, constraining the ability to perform hypothesis-driven clinical studies.
This is an Open Access image distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. From: Arias-Carrión International Archives of Medicine 2008 1:2 doi:10.1186/1755-7682-1-2
Deep Brain Stimulation
At the American Psyciatric Association meeting in San Francisco in May 2009, Giacobbe et al. reported on the results of deep brain stimulation of an anterior-ventral part of the prefrontal cortex called the subgenual cingulate cortex in patients with refractory major depressive disorder. In deep brain stimulation, electrodes are inserted directly into the brain. Twenty-one patients received this treatment in an open study at sites in Canada at McGill University, the University of British Columbia, and the University of Toronto. This multi-center trial replicated results reported by Mayberg et al. (2005) with stimulation of what is also called Broadman’s area 25, or the part of the prefrontal cortex just under the anterior part of the corpus callosum (which carries fiber tracts between the left and right sides of the brain).
Read more
Quetiapine is Effective Across a Spectrum of Illnesses
The atypical antipsychotic quetiapine (Seroquel or Seroquel XR) has a range of efficacy in a number of illnesses, depending on the size of the dose given. Read about some of its uses below, including as an adjunct to antidepressants in unipolar depression; as a treatment for generalized anxiety disorder (GAD) and post-traumatic stress disorder (PTSD); and, at higher doses, as a treatment for mania and depression. Some of its potential mechanisms of action are described as well.
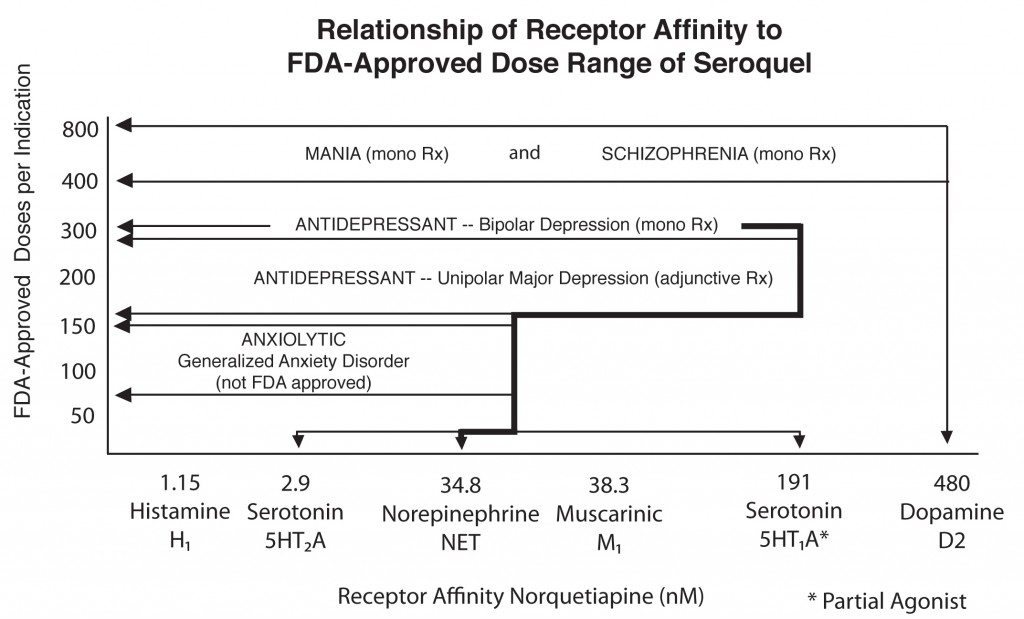
Quetiapine's actions on various receptors in the brain (bottom axis) are responsible for its effects in different illnesses
Quetiapine as an adjunct to antidepressants in unipolar depression
Posters at the American Psychiatric Association meeting in San Francisco in May 2009 showed new data from a series of studies of quetiapine in unipolar depression that showed the drug in monotherapy (at 150mg & 300mg) was significantly more effective than placebo. Studies were also positive when quetiapine was used as an adjunct compared with placebo for patients showing inadequate or incomplete responses to antidepressants such as selective serotonin reuptake inhibitors (SSRIs).
Read more




