Depression More Likely Among Perimenopausal Women with Bipolar Disorder
Researchers found that among women with bipolar disorder, those in the menopausal transition period were significantly more likely to be depressed than premenopausal women in the sample, and that the increased proclivity for depression continued in post-menopausal women as well. Wendy Marsh, Terrence Ketter, Sybil Crawford, Julia Johnson and Anthony Rothschild studied 521 women of reproductive age, 107 women in the menopausal transition period, and 145 post-menopausal women in a multi-site treatment enhancement program for bipolar disorder (STEP-BD).
The women of reproductive age ranged from 28-38 years old, and the women in the menopausal transition period averaged 42 years old and 365 days past their last menstrual period.
Women in the menopausal transition were less likely to experience a manic episode compared with reproductive aged women, and those who were post-menopausal had the least likelihood of experiencing a manic episode. These data are consistent with others in the literature that suggest that the menopausal transition may be associated with an increased proclivity to depressive episodes.
These data also raise the question of whether hormone replacement therapy in the late menopausal transition phase may be a useful adjunct for treatment-resistant depression.
The Role of Calcium in Genetic Vulnerability, Pathophysiology, and Treatment Of Bipolar Illness
One of the most consistent findings in biological psychiatry is that levels of intracellular calcium in blood elements (platelets and white cells) are higher than normal in patients with mood disorders, particularly bipolar disorder. These data are now supported by genome-wide association studies that have identified a relationship between alterations in a calcium channel and vulnerability to bipolar illness. The specific alteration is in the alpha-IC subunit of the L-type calcium channels, otherwise referred to as CACNA1C. These findings were initially reported by one group funded by the Welcome Trust, a charitable organization that funds health research, in a series of studies that included thousands of patients and controls. Investigator Pamela Sklar later replicated these findings in another large independent sample.
At the 65th Annual Scientific Convention of the Society of Biological Psychiatry, investigator Tyson Tragon reported that there were higher levels of CACNA1C in the cingulate cortex in autopsy specimens of those with bipolar illness than in controls. In a study of mice, some of which had the gene for the glutamate receptor subunit GLuR6 knocked out (i.e. production of the gene was artificially limited), the researchers found that the L-type dihydropyridine calcium channel blocker nimodipine decreased hyperactivity, amphetamine super-sensitivity, risk-taking behavior, and aggression in those with the gene removed. The dihydropyridine-type drugs like nimodipine also decreased stress-related immobilization in the wild type (the animal with normal genes) but not the knockout animals (the ones lacking GLuR6). These data suggest that alterations in a subunit of the dihydropyridine-responsive L-type calcium channel are a risk factor for bipolar illness, a brain abnormality in those who have the illness, and relevant to behavioral/pharmacological models.
Several research groups have noted that treatment with the L-type calcium channel blocker nimodipine (Nimotop) can sometimes have positive effects in mania and depression in those poorly responsive to lithium carbonate. This has been documented by Pazzaglia and Post in double blind off-on-off-on clinical trials (i.e. during off trials patients received placebo and during on trials patients received nimodipine, but the raters were unaware which pill the patient had received). In several instances, a positive response continued when the patient was switched from nimodipine to another dihydropyridine, isradapine (DynaCirc), but not when patients were switched to a different L-type calcium channel blocker, the phenylalkylamine verapamil (sold under the names Calan, Covera, Isoptin, and Verelan), which acts at a slightly different site on the channel. Read more
Schizophrenia v. Bipolar Disorder: Different Risk Factors
 Robin Murray gave a plenary presentation at the 65th Annual Scientific Convention of the Society of Biological Psychiatry this year, in which he indicated that the genetic risk for schizophrenia and other major mental disorders may be overestimated. He suggested that even in identical twins there are considerable differences in incidence of major psychiatric illnesses, and sharing an environment could further inflate the appearance of genetic risk.
Robin Murray gave a plenary presentation at the 65th Annual Scientific Convention of the Society of Biological Psychiatry this year, in which he indicated that the genetic risk for schizophrenia and other major mental disorders may be overestimated. He suggested that even in identical twins there are considerable differences in incidence of major psychiatric illnesses, and sharing an environment could further inflate the appearance of genetic risk.
Evidence of some genetic vulnerability factors, such as neuregulin, disbindin, DISC-1, zinc finger transcription factors, and neurexin, has been replicated. However, these genes appear to contribute only about 1% of the vulnerability to schizophrenia or bipolar illness. Copy number variations (CNVs, extra or missing copies of a gene, which may alter its activity) and gene micro-deletions (in which small bits of DNA are missing) have been found in about 5% of patients with schizophrenia, in some patients with autism and mental disabilities, but not in those with bipolar illness.
Murray emphasized the importance of psychosocial and neuromotor markers of neural development in determining risk of subsequent major psychiatric illness, rather than the relatively weak genetic effects. He cited the work of MacCabe (2009), who collected information from 907,000 individuals in Sweden. Their scholastic achievement at age 15?16 was rated, and hospitalizations for psychosis were recorded from age 17?31. Of the 315,000 followed for the long term, 493 developed schizophrenia and 208 developed bipolar disorder.
Predictors of cognitive and motor development in these two major psychiatric illnesses appeared to differ. In those who went on to develop schizophrenia, there was a slower rate of motor development, receptive language, and overall IQ in adolescence, while in those who went on to develop bipolar disorder, there was a faster rate of motor development, more language facility, and higher IQ in adolescence.
Early Life Stressors Linked to Persistent Inflammation and Endocrine Abnormalities
Epigenetics is a relatively new area of study that examines changes in DNA regulation and structure that can come about as a result of environmental events, as opposed to the genetic inheritance (DNA sequence) people receive through their parents’ genes. Epigenetic effects occur when an environmental stressor or chemical causes methyl or acetyl groups to attach to DNA or to histones (around which DNA are wound). These epigenetic changes determine how difficult it is to turn on genes coded in the DNA (see here for more information about the way the environment produces these epigenetic effects).
After the jump: Several studies presented at the 65th Annual Scientific Convention of the Society of Biological Psychiatry earlier this year suggested a link between environmental stress and both inflammation and abnormalities in DNA.
 Read more
Read more
Uric Acid Increases During Mania
At the 65th Annual Scientific Convention of the Society of Biological Psychiatry this year, Giacomo Salvadore reported that significantly higher levels of uric acid are found in patients with mania compared with normal controls.
Editor’s note: This study was particularly interesting because there was a highly significant difference between patients and controls, with very few values overlapping. The data suggest the possibility that uric acid may be a useful biological marker for mania, and is one that should be studied in childhood-onset bipolar illness to determine whether uric acid is a marker for mania in children as well.
Allopurinol, a widely used treatment for gout that reduces levels of uric acid in the blood, is an effective antimanic agent (based on data from two placebo-controlled studies, one by Machado-Vieira et al. and one by Akhondzadeh et al.). The new data on uric acid raise the possibility that high levels of uric acid may be a specific predictor of responsiveness to Allopurinol, although this hypothesis has not yet been explored.
In an article by Chung et al. just published in Psychiatry Research, it was reported that in a very large epidemiological study in Taiwan, patients with bipolar disorder have increased risk of gout.
Bipolar Disorder Worse in US than Europe
New research shows that there are more early onsets of illness and more difficult courses of bipolar illness in the US than in the Netherlands or Germany.
This editor was invited to give a plenary presentation at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. The talk, titled “A greater incidence of early onset bipolar illness and poor prognosis factors in patients in the US compared with those in The Netherlands and Germany,” was based on studies in our Bipolar Collaborative Network.
We found that patients who were studied and treated at four sites in the US (Los Angeles, Dallas, Cincinnati, and Bethesda) had more poor-prognosis factors and indices of difficult courses of bipolar illness compared with patients studied in the same fashion at three sites in Utrecht, the Netherlands and Freiberg and Munich, Germany. We presented some of these data in a preliminary report in the British Journal of Psychiatry in 2008 and further analyzed these data for an article published last year in the Journal of Clinical Psychiatry. Read more
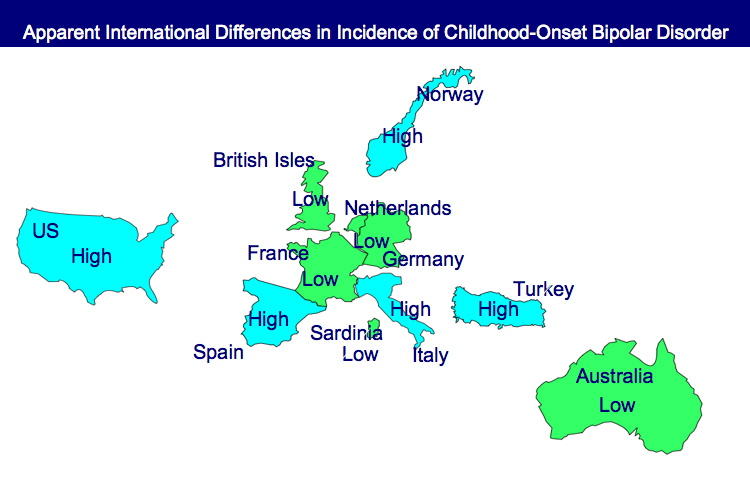
Incidence of Childhood Onset Bipolar Disorder Varies Geographically: More in US than Europe
A poster by Aditya Sharma of Newcastle University and colleagues at the Pediatric Bipolar Conference assessed the incidence of childhood-onset bipolar illness based on monthly letters sent to approximately 750 consultants in child and adolescent psychiatry in the British Isles. Only five confirmed cases were reported, with the youngest child being 11 years old.
EDITOR’S NOTE: These data are of particular interest in relationship to earlier data indicating that childhood-onset bipolar disorder may be relatively rare in some European countries, including the British Isles, France, the Netherlands, and Germany, as well as in Australia, South Korea, and New Zealand.
In contrast, childhood-onset bipolar illness with an onset prior to age 13 appears to be prevalent in the US, with one-fifth to one-quarter of adult outpatients reporting onsets of either depression with dysfunction or mania prior to age 13. Another substantial group of patients report onsets in adolescence, indicating that some 50-66% of bipolar illness in the US begins in either childhood or adolescence.
Similarly higher amounts of childhood-onset bipolar illness are reported in Italy, Turkey, and Norway, indicating some heterogeneity of vulnerability factors and course of illness outcomes among different European countries.
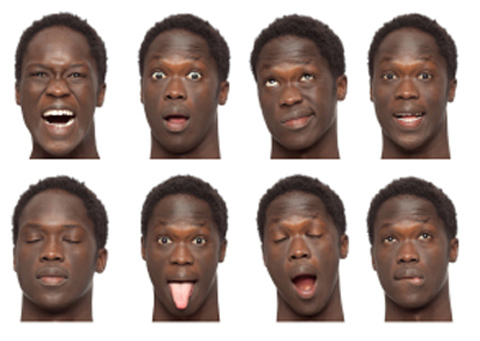
Consistent Deficits In Facial Emotion Recognition Found in Non-Ill Children of Parents with Bipolar Disorder
Children with bipolar parents may have difficulty identifying the emotions they see on another person’s face. Aditya Sharma of Newcastle University presented a poster at the Pediatric Bipolar Conference in Cambridge, Massachusetts in March, which indicated that children without bipolar disorder but at risk because a parent has the illness showed deficits in facial emotion recognition. Similar results were reported by Brotman et al. in the American Journal of Psychiatry in 2008. Since children of bipolar parents are at increased risk of developing the disease, this deficit in labeling facial emotion may be a marker of early bipolar disorder or a risk factor for its onset.
Editor’s Note: These types of deficits in facial emotion recognition have been consistently observed in adults and children diagnosed with bipolar disorder, so assessing whether children can successfully identify others’ facial emotions could become part of the assessment of risk for bipolar disorder. This deficit could also be targeted for psychosocial intervention and rehabilitative training to enhance emotion recognition skills. Such an approach could improve interpersonal communication and lessen hypersensitive responses to perceived emotional threats and negative emotional experiences.
Environmental Influences on Gene Structure May Be Transmitted to Offspring
It has been thought that one fundamental principle of genetics is that the impact of environment factors cannot be passed from one generation to the next via the genetic code. New data suggest this may not be true.
In an emerging field called epigenetics, researchers are finding that while the impact of environment and life experiences is not registered in DNA sequences, environmental factors can influence the structure of DNA or tightness of its packaging. Early life experiences, particularly psychosocial stress, can lead to the accumulation of methyl groups on DNA (a process called methylation), which generally constricts DNA’s ability to start transcription (turning on) of genes and the synthesis of the proteins the genes encode. DNA is tightly wound around proteins called histones, which can also be methylated or acetylated based on events in the environment. When histones are acetylated, meaning that acetyl groups are attached to them, DNA is wound around them more loosely, facilitating gene transcription (i.e. the reading out of the DNA code into messenger RNA, which then arranges amino acids in order to construct proteins). Conversely, histone methylation usually tightens the winding of DNA and represses transcription.
Inflammation in the Affective Disorders
Bipolar children exhibit more inflammation than healthy children, according to a paper presented by Pandey, Dwivedi, and Pavuluri from the University of Illinois at the American College of Neuropsychopharmacology in December 2009.
In “Pro-inflammatory cytokines in plasma of patients with pediatric bipolar disorder,” the researchers described their study in which 21 normal controls were compared with 22 children with pediatric bipolar disorder who were unmedicated for a period of at least two weeks. The level of the inflammatory cytokine interleukin-1b (IL-1b) was significantly higher in the pediatric bipolar patients compared with controls, and levels of TNF alpha, another inflammatory marker, were significantly higher as well. Not only is this evidence of increased inflammatory processes in pediatric bipolar disorder, but TNF alpha is associated with activation of transcription factors and the initiation of preprogrammed cell death, or apoptosis.