Sleep Disturbances in Pediatric Bipolar NOS is the Same as in BP I
Gianni Faedda reported in Frontiers in Psychiatry (2012) that decreased need for sleep is as prominent in BP NOS children as in those with BP I. So it appears that with the exception of only brief periods of mania in BP NOS, these children have similar characteristics to those with full blown BP I. Thus in addition to the briefer periods of mania, one should be on the look out for all the symptoms of bipolar disorder that are not typical of ADHD, including brief or extended periods of euphoria, decreased need for sleep, more extreme degrees of irritability and poor frustration tolerance, hallucination, delusions, suicidal and homicidal ideation, more severe depression, and increases in sexual interest and actions. When these are present, the bipolar mood instability should be treated first and only then small doses of psychomotor stimulants can be used to treat what ever residual ADHD remains. The typical symptoms of ADHD are very of present and comorbid in childhood onset bipolar disorder and cannot be used to discriminate the two diagnoses. The children with BP NOS are as dysfunctional as those with BP I and take longer to stabilize, so pharmacological treatment may need to be intensive, multimodal, and supplemented by Family Focused Therapy (FFT) or a related family therapy. It is most often not conceptualized as such, but BP NOS as well as BP I should be considered as a medical emergency and handled by a sophisticated pediatrician and/or referred for psychiatric consultation and therapy. The longer bipolar disorder is not treated, the worse the outcome is in adulthood.
Two different subtypes of early onset unspecified bipolar disorder (USBD)
The first subtype is classical BP NOS (Not Otherwise Specified) having all the characteristics of full-blown bipolar disorder except for only having brief durations of mania and responding to conventional treatment. The second is what is now called Temperature and Sleep Dysregulation Disorder (TSDD) and was formerly described by D. Papolos as the Fear of Harm (FOH) syndrome, and requires a different treatment approach.
Clinicians should be alert to unique symptoms in children who might have TSDD as such a diagnosis would lead to a unconventional treatment paradigm. We emphasize the importance of specifically asking parents about evidence of over heating (red face and red ears) and high tolerance for cold (going outside markedly under-dressed) and the presence of fear of sleep and horrific nightmares, as these may lead one to consider the diagnosis of TSDD.
If these two novel aspects (temperature and sleep dysregulation) occur in the presentation of a highly fearful and behaviorally dysregulated child with bipolar-like symptoms, these may lead to the consideration of an unconventional treatment paradigm. It utilizes 1) high dose lithium; 2) clonidine and other practical approaches to achieve cooling and relieve over heating; and 3) ascending doses of intranasal ketamine (as described by Papolos et al 2013; 2018). This may be of considerable clinical importance as a large group of children with this unique presentation respond very poorly to conventional treatments for bipolar disorder and remain highly impaired and dysfunction throughout their childhood and adolescence.
If these children instead are treated with: lithium (to achieve blood levels of 1.0 meq/L or higher); clonidine (0.1- 0.3mg IR and 0.1mg ER at noon and HS) and other practical ways to achieve cooling; followed by ascending intranasal doses of ketamine (starting at 20mg and increasing toward 80-260mg/day, repeated every 2-3 days), marked improvement can be achieved. This occurs in conjunction with ketamine’s positive effects on fear and aggressive behaviors in association with its ability to reduce core body temperature.
We highlight this potential alternative treatment approach as long term positive effects have been achieved with it in open case series (Papolos et al 2013; 2018 ). The efficacy of this treatment approach has not been validated in controlled clinical trials, but we believe wider recognition of the two subtypes of USBD– BPNOS and TSDD,– will lead to more systematic research on treatment. Actively looking for the unique features of TSDD and pursuing its unconventional treatment may lead to long term positive effects in a child previously viewed as having an intractable psychiatric illness.
Potential of Environmental Enrichment to Prevent Transgenerational Effects of Paternal Trauma
Gapp, K. et al. wrote about the “Potential of Environmental Enrichment to Prevent Transgenerational Effects of Paternal Trauma” in Neuropsychopharmacol 41, 2749–2758 (2016).
They “used a mouse model of unpredictable maternal separation combined with unpredictable maternal stress (MSUS) to examine the consequences of traumatic stress on coping behaviors in adulthood and across generations, and the potential contribution of (glucocorticoid receptors) GR. We show that MSUS affects avoidance behaviors and learning in aversive environments in exposed fathers and their male offspring. This is associated with an increase in GR expression in the hippocampus, and with decreased DNA methylation of GR promoter in the hippocampus and in germ cells. We show that transmission of the effects of paternal trauma can be prevented by paternal (environmental enrichment) EE, suggesting a reversibility of these effects.”
Editors Note: Dad’s early environmental adversity alter his response to traumatic stress as an adult, and this can be passed to the next generation via epigenetic changes in DNA methylation, histone and microRNA chemical changes persisting in sperm. If the dad with early life adversity is housed in an enriched environment, he does not have the altered response to stress or the changes in GR, and his offspring do not have the transgenerational alterations in stress responsively. This could probably happen in people if we could only figure out to super good environmental enrichment in those having early life adversity. Having lots of stress as a neonate and then being adopted out to wonderful foster family could be the basis for a naturalistic study of this sort of result.
Lurasidone Effective Long-Term in Pediatric Bipolar Depression

At the 2020 meeting of the American Society of Clinical Psychopharmacology, researcher Manpreet Singh presented data showing that children aged 10–17 with bipolar depression had an excellent long-term response to the antipsychotic medication lurasidone (trade name Latuda).
Lurasidone has been approved by the US Food and Drug Administration as a monotherapy treatment of bipolar depression in children and adolescents since 2018. Following a six-week double-blind study comparing lurasidone with placebo in 305 children and adolescents, Singh and colleagues carried out an open-label extension study in which all of the young participants, including those in the placebo group, had the option of taking lurasidone for up to two more years.
Of those, 195 children completed one year of treatment, and 93 completed two years of treatment. Rates of response were 51.0% after the six-week preliminary study; 88.4% at one year; and 91.1% at two years. Rates of remission were 24.3% after the six-week study; 61.3% at one year, and 75.6% at two years, while rates of recovery were 17.7% after the preliminary study; 53.8% at one year; and 73.8% at two years.
This improvement in depression had a strong correlation with improvement in functioning, as measured by the Children’s Global Assessment score (CGAS). The results show progressive increases in rates of response, remission, and recovery with duration of treatment that are associated with improvement in functioning.
Early Precursors of Mood Disorders in Young Children of Parents with Bipolar or Unipolar Disorder

At the 2020 meeting of the International Society for Bipolar Disorders, researcher Caroline Vandeleur presented findings from a 13-year study of children in Switzerland who have a parent with bipolar disorder or major depressive disorder. In contrast to findings from the US presented by Danella Hafeman, Vandeleur and colleagues found no evidence of psychopathology in 4 year-olds. They did find that in 7-year-olds, children of a parent with major depressive disorder were four times more likely to have a separation anxiety disorder. In an overall sample of 449 children with a mean age of 10 who were followed up for 13 years, major depression tended to be preceded by anxiety disorders. Participants who went on to be diagnosed with bipolar disorder had earlier symptoms of depression, subthreshold hypomania, conduct disorders, and drug abuse. These were especially common in those who had a parent with bipolar disorder.
Editor’s Note: These data indirectly confirm other observations in which children at high risk for mood disorders in the US showed earlier signs of psychopathology than those in other countries including the Netherlands and Canada.
Predicting Onset of Bipolar Disorder in Children at High Risk: Part I
 At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported.
At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported.
Symptom Progression
In offspring of parents with bipolar disorder, researcher Anne Cecilia Duffy found that symptoms in the children tended to progress in a typical sequence. Childhood sleep and anxiety disorders were first to appear, then depressive symptoms, then bipolar disorder.
Different Types of Illness May Respond Best to Different Medications
Duffy’s research also suggested links between illness features and a good response to specific medications. Those offspring who developed a psychotic spectrum disorder responded best to atypical antipsychotic medication. Those with classical episodic bipolar I disorder responded well to lithium, especially if there was a family history of lithium responsiveness. Those offspring with bipolar II (and anxiety and substance abuse) responded well to anticonvulsant medications.
If parents with bipolar disorder had experienced early onset of their illness, their children were more likely to receive a diagnosis of bipolar disorder.
The offspring of lithium-responsive parents tended to be gifted students, while those from lithium non-responders tended to be poorer students.
Comparing Risk Factors for Bipolar Disorder and Unipolar Depression
Researcher Martin Preisig and colleagues also showed that parental early onset of bipolar disorder (before age 21) was a risk factor for the offspring receiving a diagnosis of bipolar disorder. Parental oppositional defiant disorder (ODD) was also a risk factor for bipolar disorder in the offspring. The emergence of depression, conduct disorder, drug use, and sub-syndromal hypomanic symptoms also predicted the onset of mania during childhood.
Conversely, sexual abuse and witnessing violence were strong risk factors associated with a diagnosis of major (unipolar) depressive disorder. Being female and experiencing separation anxiety were also factors that predicted unipolar depression.
Predicting Conversion to Mania
Researcher Danella M. Hafeman reported that mood swings (referred to in the literature as “affective lability”), depression/anxiety, and having a parent who had an early onset of bipolar disorder were linked to later diagnoses of mania. Immediate risk factors that predicted an imminent onset of mania included affective lability, substance abuse, and the presence of sub-threshold manic symptoms.
Positive Effects of a Brief Session of Aerobic Exercise for Sedentary Children
At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Benjamin I. Goldstein reported that a single 20-minute session of aerobic exercise (achieving 70% of maximal heart rate) was associated with improvement in cognition and in abnormalities seen on brain imaging in young people. Goldstein urged clinicians to do motivational interviews with sedentary children in their care, emphasizing the positive cardiovascular and cognitive effects of exercise. He indicated this would be more effective than a focus only on weight loss, which is much more difficult to achieve.
Quetiapine Reduced Childhood Mania, Especially in Those with Thicker Frontal Temporal Regions
 In a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Melissa P. Delbello reported that six weeks of treatment with either lithium or quetiapine was effective in childhood mania, but quetiapine had a higher response rate of 71% versus 46% for lithium. Delbello found two types of structural changes on functional magnetic resonance imaging (fMRI). Some children had thicker frontal temporal regions, while others had thinning in these areas. The first group of patients had a 100% response to quetiapine, but only 53% of the second group responded to quetiapine.
In a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Melissa P. Delbello reported that six weeks of treatment with either lithium or quetiapine was effective in childhood mania, but quetiapine had a higher response rate of 71% versus 46% for lithium. Delbello found two types of structural changes on functional magnetic resonance imaging (fMRI). Some children had thicker frontal temporal regions, while others had thinning in these areas. The first group of patients had a 100% response to quetiapine, but only 53% of the second group responded to quetiapine.
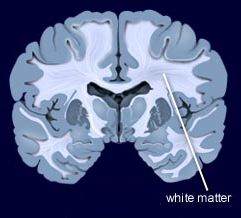
In contrast, other researchers have found lithium superior to quetiapine. Vivian Kafantaris showed that patients who respond well to lithium show improvements in white matter abnormalities. Michael Berk and colleagues found that a year on lithium was superior to quetiapine on all measures including cognition and brain imaging in patients having their first episode of mania.
7-Year-Olds At Risk for Schizophrenia, But Not Bipolar Disorder, Show Specific Types of Cognitive Dysfunction
 A large Danish study investigated whether children at risk for schizophrenia and bipolar disorder would show signs of cognitive problems. The study by researcher Nicoline Hemager and colleagues was published in the journal JAMA Psychiatry in 2018.
A large Danish study investigated whether children at risk for schizophrenia and bipolar disorder would show signs of cognitive problems. The study by researcher Nicoline Hemager and colleagues was published in the journal JAMA Psychiatry in 2018.
The researchers identified 7-year-olds,197 who had family members with schizophrenia, 118 who had family members with bipolar disorder, and 199 control 7-year-olds with no family history of these illnesses. Those children at risk for schizophrenia had significantly more cognitive deficits and behavioral disorders than the controls, while those children at risk for bipolar disorder did not differ significantly from the controls. The deficits among the children at risk for schizophrenia were in the areas of processing speed and working memory, executive and visuospatial functions, and declarative memory and attention.
The researchers indicated that the neurocognitive profile seen in the children at risk for schizophrenia could help clinicians identify these children for early intervention.
Lithium Effective for Maintenance Treatment of Childhood-Onset Bipolar Disorder
Evidence has been accumulating that lithium is effective in the treatment of young people with bipolar disorder. In a study by Robert Findling and colleagues published in the Journal of the American Academy of Child and Adolescent Psychiatry in 2018, participants aged 7–17 who responded well to lithium during a 24-week study were then randomized to receive either lithium continuation (17 participants) or placebo (14 participants) for 28 more weeks.
Those who continued lithium treatment were more likely to stay in the study. Participants who discontinued the study mostly reported that they did so due to re-emergence of their mood symptoms (mostly in the placebo group).
Lithium was well-tolerated and was not associated with any more weight gain than placebo. This study adds to the growing literature on the effectiveness and tolerability of lithium both acutely and in maintenance treatment in childhood bipolar disorder.



