Inflammation Linked to Poor Sleep Quality and Worse Executive Functioning
At a recent scientific meeting, researcher Ellen E. Lee and colleagues reported that compared to healthy volunteers, people with bipolar disorder or schizophrenia had elevated levels of inflammatory markers, which were associated with poor sleep.
According to self-reports, people in the schizophrenia and bipolar disorder group had worse sleep quality than the control group. Those with schizophrenia or bipolar disorder also had significantly higher levels of the inflammatory markers CRP, IL-6, and TNF alpha compared to the healthy volunteers. Among people with bipolar disorder, executive functioning and sleep quality had a strong inverse association to levels of IL-6, such that lower sleep quality and worse executive functioning were associated with higher levels of IL-6. These findings suggest that sleep disturbance and inflammation may have negative consequences for cognitive functioning.
White Matter Abnormalities in Obesity
Researcher Ramiro Reckziegel and colleagues reported at a recent scientific meeting that white matter is abnormal in obese adults with bipolar disorder. In a 2018 article in the journal Schizophrenia Bulletin, Reckziegel reported that body mass index (BMI) was associated with reduced fractional anisotropy, a measure of brain fiber integrity, in the cingulate gyrus in patients with bipolar disorder. This finding implies that obesity may play a role in white matter microstructure damage in the limbic system.
White Matter Abnormalities Linked to Irritability in Both Bipolar Disorder and DMDD
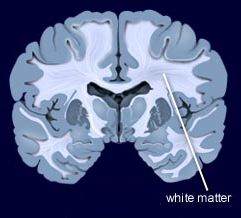 At a 2018 scientific meeting, researcher Julia Linke of the National Institute of Mental Health reported that there were white matter tract abnormalities in young people who had irritability associated with either bipolar disorder or disruptive mood dysregulation disorder (DMDD). Thus, while these two disorders differ in terms of diagnosis, presentation, and family history, they seem to have this neurobiological abnormality in common.
At a 2018 scientific meeting, researcher Julia Linke of the National Institute of Mental Health reported that there were white matter tract abnormalities in young people who had irritability associated with either bipolar disorder or disruptive mood dysregulation disorder (DMDD). Thus, while these two disorders differ in terms of diagnosis, presentation, and family history, they seem to have this neurobiological abnormality in common.
Scientific Mechanisms of Rapid-Acting Antidepressants
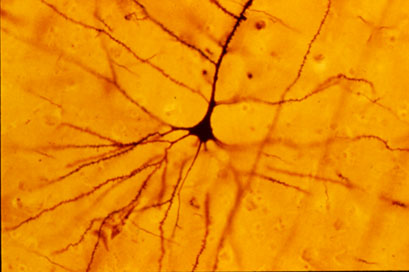
A pyramidal cell (Photo by Bob Jacobs, Laboratory of Quantitative Neuromorphology Department of Psychology Colorado College)
At a recent symposium, researcher Francis McMahon provided electrophysiological evidence that several different types of rapid-acting antidepressants—low-dose ketamine, scopolamine, and rapastinel (a partial agonist of the neurotransmitter NMDA)—act by decreasing the inhibitory effects of GABAergic interneurons on excitatory neurons called pyramidal cells, thus increasing synaptic firing.
Researcher Ronald Duman further dissected these effects, showing that ketamine and its active metabolite norketamine reduce the steady firing rate of GABA interneurons by blocking NMDA receptors, while the partial agonist rapastinel acts on the glutamate neurons directly, and both increase the effects of a type of glutamate receptors known as AMPA. These effects were demonstrated using a virus to selectively knock out GluN2B glutamate receptor subunits in either GABA interneurons or glutamate neurons.
Increasing AMPA activity increases synapse number and function and also increases network connectivity, which can reverse the effects of stress. Duman and colleagues further showed that when light is used to modulate pyramidal cells (a process called optogenetic stimulation) in the medial prefrontal cortex, different effects could be produced. Stimulating medial prefrontal cortex cells that contained dopamine D1 receptors, but not D2 receptors, produced rapid and sustained antidepressant effects. Conversely, inhibiting these neurons blocked the antidepressant effects of ketamine. Stimulating the terminals of these D1-containing neurons in the basolateral nucleus of the amygdala was sufficient to reproduce the antidepressant effects. These data suggest that stimulation of glutamate D1 pyramidal neurons from the medial prefrontal cortex to the basolateral nucleus of the amygdala is both necessary and sufficient to produce the antidepressant effects seen with ketamine treatment.
Researcher Hailan Hu reported that NMDA glutamate receptors drive the burst firing of lateral habenula (LHb) neurons, which make up the depressogenic or “anti-reward center” of the brain and appear to mediate anhedonic behavior (loss of interest or enjoyment) in animal models of depression. Ketamine blocks the burst firing of the LHb neurons, which disinhibits monoamine reward centers, enabling ketamine’s rapid-onset antidepressant effects. This may occur because inhibitory metabotropic glutamate receptors (mGluR-2) are activated, decreasing the release of glutamate.
MGluR-2 may also help explain the antidepressant effects of acetyl-L-carnitine supplements. L-carnitine is an amino acid that is low in the blood of depressed patients. The supplement acetyl-L-carnitine (ACL) activates the DNA promoter for mGluR-2, increasing its production and thus decreasing excess glutamate release. The acetyl group of the ACL binds to the DNA promoter for mGluR-2, thus this process seems to be epigenetic. Epigenetic mechanisms affect the structure of DNA and can be passed on to offspring even though they are not encoded in the DNA’s genetic sequence.
Risk of Suicide in People with Bipolar Disorder: Lowest with Lithium, Highest with Antidepressants
Researcher Markku Lähteenvuo and colleagues reported in the journal JAMA Psychiatry in early 2018 that long-acting injectable antipsychotics and lithium were best at preventing re-hospitalization in 18,018 bipolar patients in Finland who received an average of more than 7 years of follow up. Lähteenvuo and colleagues have now gone on to analyze suicide data from the same cohort of patients with bipolar disorder, and report that those taking lithium had the lowest rate of suicide, while those taking valproate had the next lowest suicide rate. Those patients with bipolar disorder who were treated with antidepressants had the greatest suicide rate. The suicide rate was particularly high for those once-hospitalized patients taking the MAO inhibitor antidepressant meclobemide, which is not approved for use in the US. Increased rates of suicide were also seen with use of sedatives and benzodiazepines.
Editor’s Note: Evidence continues to mount that lithium should be the definitive first line therapy in bipolar disorder for a multitude of reasons (as this editor Robert M. Post reviewed in an open-access article in the journal Neuropsychopharmacology in 2017). Still, lithium is not often prescribed for people with bipolar disorder in the US, and this does not seem to be in these patients’ best interests.
Use of antidepressants in bipolar disorder has remained controversial, but it is common in clinical practice despite a lack of evidence that it is effective, and the presence of some evidence that it is actually harmful. Antidepressant use in a person with bipolar disorder may cause switching into mania, cycle acceleration, dysphoria induction, and even suicide.
Clinicians should take these data seriously and overcome the impulse (leftover from treating unipolar depression) to use unimodal antidepressants as first line or adjunctive therapy for bipolar depression. Antidepressants are only effective in the long term in about 15% of patients with bipolar depression, and now it appears antidepressant use also carries an additional risk of suicide.
High Baseline Levels Of C-Reactive Protein Predict Better Response To Lurasidone in Bipolar Depression
In a study presented at the 2017 meeting of the International Society for Affective Disorders, Charlies L. Raison and colleagues examined whether baseline levels of the inflammatory marker C-reactive protein (CRP) affected antidepressant response to the antipsychotic drug lurasidone in bipolar depression. The participants were divided into three double-blind groups: one received 20–60mg/day of lurasidone, another received 80–120 mg/day of lurasidone, and the third received placebo over a period of six weeks. The effect was dramatic—in people with CRP levels above 5 mg/L at the beginning of the study, lurasidone (at either dosage level) had a very large effect size (d=0.85), while in people with baseline CRP levels below 5 mg/L the effect size was smaller (d=0.35).
Interestingly, 118 of the participants (24.5%) had CRP levels above 5mg/L at baseline, indicating a substantial amount of inflammation was present in a quarter of the bipolar depressed patients. Higher levels of CRP at baseline were correlated with better improvement on specific items on the Montgomery–Åsberg Depression Rating Scale (MADRS): “lassitude” (or lack of energy), “apparent sadness,” “reported sadness,” and “pessimistic thoughts.” Raison and colleagues concluded: “These findings suggest that the efficacy of lurasidone in patients with bipolar depression may in part be linked to the inflammatory status of patients prior to treatment. If confirmed in prospective investigations, [the results of a wide-range CRP assay] may prove useful as a predictive biomarker that could help optimize the use of lurasidone for the treatment of patients with bipolar depression.”
Editor’s Note: In many instances, high levels of CRP predict a poor response to treatment (such as to selective serotonin reuptake inhibitor antidepressants (SSRIs) in unipolar depression), so these findings are of considerable interest. They also suggest the untested possibility that lurasidone has anti-inflammatory effects, as those with high levels of inflammation at baseline often respond better to drugs with direct anti-inflammatory effects such as celecoxib (Celebrex) or the antioxidant N-acetylcysteine (NAC).
Vitamin D3 Improves Depression in Older Adults
Researcher Negin Masoudi Alavi and colleagues reported in the journal Clinical Nutrition in 2018 that compared to placebo, 50,000 IU of vitamin D3 taken weekly for eight weeks improved depression in depressed patients over the age of 60.
Although the literature about vitamin D3’s effects on depression are mixed, a 2014 meta-analysis by Simon Spedding in the journal Nutrients found that in studies of vitamin D-deficient depressed participants whose vitamin D levels were restored to normal levels by the end of the study, vitamin D significantly improved depression. (Spedding attributed earlier mixed results to studies that did not clearly correct a vitamin D deficiency.) A 2013 study by Nayereh Khoraminya and colleagues in the Australian and New Zealand Journal of Psychiatry suggested that a 1500 IU dose of vitamin D3 combined with the selective serotonin reuptake inhibitor (SSRI) antidepressant fluoxetine improved depression more than fluoxetine plus placebo in depressed patients who were not necessarily deficient in vitamin D. Another study by Jacqueline A. Pettersen in the journal Experimental Gerontology found that in healthy adults, 4,000 IU of vitamin D3 improved cognitive functioning (namely visual memory) more than 400 IU.
Editor’s Note: Given these promising studies, the safety of D3, and fact that psychiatric patients are often deficient in vitamin D3, taking vitamin D3 supplements to improve depression might be worth trying.
American Academy of Pediatrics Recommends Parents Avoid Spanking and Verbal Abuse
The American Academy of Pediatrics (AAP) has issued a policy statement calling for an end to corporal punishment, including spanking. These forms of punishment are tied to negative outcomes in every developmental area.
Children spanked regularly at age 3 had increased aggression risk by age 5. They also had more negative behaviors and lower vocabulary scores at age 9. Abusive behavior raises stress hormones and is associated with mental health struggles.
Verbal abuse should also be avoided. Verbal abuse includes punishment that shames, humiliates, threatens, frightens, or ridicules a child. Use of time outs, removal of privileges, and other forms of quiet discipline are recommended alternatives.
Editor’s Note: In our research network, the Bipolar Collaborative Network, we found that verbal abuse by itself (without the physical or sexual abuse that often accompany it) is associated with an earlier age of onset of bipolar disorder and a more difficult course of illness.
Family focused therapy (FFT) and other forms of family therapy are highly recommended for children of a parent with bipolar illness. These children are at high risk for a variety of psychiatric diagnoses, and those already experiencing depression, cyclothymia (mood swings between high and low) or a diagnosis of bipolar disorder not otherwise specified (BP-NOS) are much improved with FFT compared to treatment as usual. FFT teaches family members to recognize symptoms of illness for what they are rather than interpreting them as deliberate hostility, increases family communication and problem solving, and leads to good long-term outcomes.
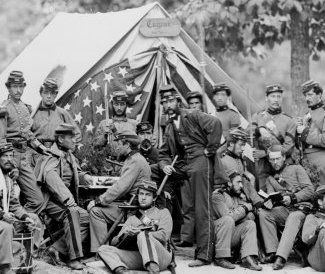
Civil War Data Shows Father’s Trauma Can Affect Son’s Lifespan
An economist at the University of California Los Angeles (UCLA) has used Civil War data to determine that trauma experienced by a father can affect the lifespan of his son, but that a mother’s healthy diet during pregnancy can neutralize this risk.
Researcher Dora Costa used records from the National Archive to identify Union soldiers who were held as prisoners of war (POWs) by the Confederacy. She compared records of their children’s lifespans to the children of Union soldiers who were never held as POWs, finding that the sons of POWs were more likely to have died at any given age. (The study included only children who lived to be at least 45 years old.) Detailed records were kept because families of soldiers and POWs were eligible for generous pensions.
When looking at the data, Costa expected to find that socioeconomic status was the factor that explained discrepancies in lifespans among children of Civil War veterans. However, she noticed that the difference in lifespan only appeared in sons, and only to sons born after the war.
This pointed to an epigenetic explanation. Epigenetics is the idea that some aspects of a parent’s experiences (such as deprivation, drug use, etc.) can be passed on to their children during the gene transcription process. While a parent’s inherited genetic sequence doesn’t change, the structure of their DNA can be wound tightly or loosely depending on life experiences, and this affects how easily their genes are transcribed when passed on to their children.
The sons of POWs in the worst camp environments (typically during the later years of the war when prisoner exchanges were less frequent and overcrowding and malnutrition were common in camps) had even shorter lifespans than the sons of POWs who were imprisoned in less dire circumstances.
The research also looked at birth months to determine whether mothers would have had access to good nutrition while pregnant. Sons born to POW fathers in the later months of the year (whose mothers were likely to have had access to good nutrition) had lifespans comparable to the sons of non-POWs, while sons of POWs born earlier in the year fared worse.
The research was published in the journal Proceedings of National Academy of Sciences in 2018.
Editor’s Note: This is another example in humans of findings that have been clear-cut in animal studies. A father’s experiences, such as stressors or substance abuse, can influence the next generation even if the parent has no contact with the offspring. Epigenetic marks on DNA, histones (the structures around which DNA is wound), or microRNA of the sperm appear to carry these unexpected transgenerational effects.
Inflammation is Associated with Antidepressant Treatment Resistance
Researcher Ebrahim Haroon and colleagues report in a 2018 issue of Psychoneuroendocrinology that people whose depression failed to respond to at least three different antidepressants in their current episode of depression had higher levels of inflammation than those who had fewer than three failed antidepressant trials.
The researchers found that patients who had not responded to antidepressants had higher levels of the inflammatory markers TNF-alpha, TNF-alpha receptor 2, and Il-6. The inflammatory marker CRP was also significantly elevated in these patients when statistical analyses that excluded body mass index (BMI) were used.
Haroon and colleagues reported that a third of all patients with major depressive disorder fail to respond to currently available antidepressant treatments, and that inflammation may be to blame because it interferes with the neurotransmitter systems that antidepressants target.
Editor’s Note: These data indirectly support the use of anti-inflammatory drugs to augment the effects of antidepressants in patients with treatment resistant depression. A caution that may be very important is to assess evidence of inflammation at baseline, as some data suggest that people with low CRP may, for example, do more poorly with a blocker of TNF-alpha, while people with high CRP at baseline (over 3 pg/ml) show good improvement.