Bipolar Disorder Worse in US than Europe
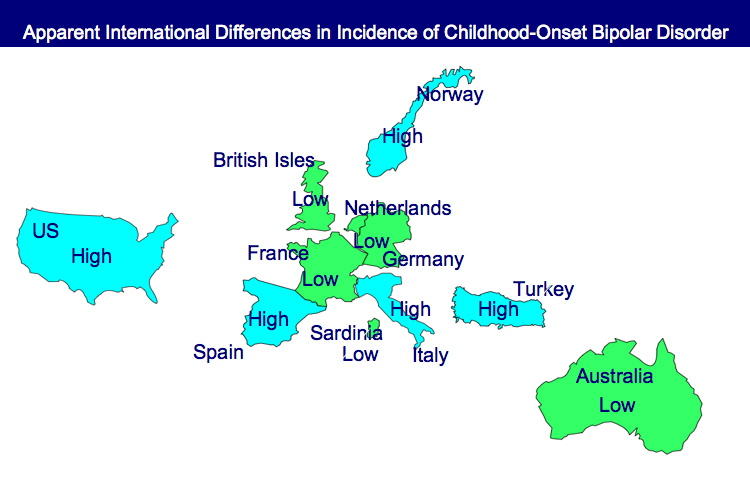
New research shows that there are more early onsets of illness and more difficult courses of bipolar illness in the US than in the Netherlands or Germany.
This editor was invited to give a plenary presentation at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. The talk, titled “A greater incidence of early onset bipolar illness and poor prognosis factors in patients in the US compared with those in The Netherlands and Germany,” was based on studies in our Bipolar Collaborative Network.
We found that patients who were studied and treated at four sites in the US (Los Angeles, Dallas, Cincinnati, and Bethesda) had more poor-prognosis factors and indices of difficult courses of bipolar illness compared with patients studied in the same fashion at three sites in Utrecht, the Netherlands and Freiberg and Munich, Germany. We presented some of these data in a preliminary report in the British Journal of Psychiatry in 2008 and further analyzed these data for an article published last year in the Journal of Clinical Psychiatry. Read more
Treatment Guidelines for Two Hypothetical Cases in Children
There are no FDA-approved treatments for children under age 10 with bipolar disorder. For an article in Psychiatric Annals, this editor and Janet Wozniak asked experts how they would sequence treatment of a hypothetical case of a 6-year-old with extreme mood instability consistent with a diagnosis of BP -NOS (see Table I). We also asked how the experts would treat a different case of a 9-year-old with a full-blown psychotic BP-I mania (see Table II).
The results are presented and discussed in detail in the article, and are presented here to reinforce several points. The recommendations for children under 10 and for BP NOS are highly similar to consensus guidelines for older BP I children compiled by Kowatch et al.
Treatments in the face of non-response to option A or others are sequenced differently by different experts, but almost always involve an atypical antipsychotic (AA) or a mood stabilizer (MS) such as lithium, valproate, carbamazepine/oxcarbazepine, or rarely, lamotrigine. Revisions of atypical antipsychotics and mood stabilizers and use of combinations are the common next strategies.
Faster, Better Response to Risperidone than Valproate in Adolescents with Bipolar Disorder
An article by Pavuluri et al. published in Bipolar Disorders in September reported that both divalproex sodium (valproate, or Depakote) and risperidone (Risperdol) were effective in youth with bipolar disorder, but improvements appeared more quickly with risperidone. Risperidone also produced higher response rates, higher remission rates, and fewer dropouts from side effects.
A presentation by the research group at an earlier conference suggested that it was particularly among those with comorbid disruptive behavioral disorders (DBD), which include attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), and conduct disorder (CD), that risperidone worked faster and produced greater early results than divalproex.
 In the study, 66 children with type I bipolar disorder and a mean age of 11 years were assessed. Treatment with risperidone was initiated at 0.5 mg/day and titrated to 2 mg, while divalproex was initiated at 60 micrograms/mL and titrated up to 120 micrograms.
In the study, 66 children with type I bipolar disorder and a mean age of 11 years were assessed. Treatment with risperidone was initiated at 0.5 mg/day and titrated to 2 mg, while divalproex was initiated at 60 micrograms/mL and titrated up to 120 micrograms.
Editor’s Note: The possibility that children with different comorbid disorders respond differently to different antimanic agents suggests that more studies are needed to determine which subgroups of patients are most responsive to typical treatments.
Inflammation and Oxidative Stress in Bipolar Disorder
A number of studies presented at the 4th Biennial Conference of the International Society for Bipolar Disorders conference in Sao Paulo, Brazil in March reported new data relevant to inflammation and oxidative stress. Both inflammation and oxidative stress increase risk of cardiovascular disorders, and patients with inadequately treated mood disorders lose 10 or more years of life expectancy from cardiovascular disorders compared to the general population. Inflammation and oxidative stress may also contribute to the symptoms, evolution, and progression of the mood disorders themselves.
It is possible that these two processes could become new targets for therapeutic intervention in addition to more traditional psychopharmacological drugs that primarily target the neurotransmitters dopamine, norepinephrine, serotonin, and the neurotrophic factor BDNF. Read more
Thyroid Augmentation Helps Depression (And Bipolar Disorder in Women)
Low dose thyroid replacement treatment with T3 (Cytomel) (25-37.5 µg) is typically recommended for acute antidepressant augmentation in unipolar and bipolar depression. This approach has few side effects and works even in those with normal thyroid function at baseline.
Some data also supports the use of relatively high (supraphysiological) doses of T4 (Synthroid) late in the treatment of highly treatment-resistant patients with unipolar and bipolar disorder. These supra-physiological doses of T4 typically ranged from 300-500 µg/day, producing a free thyroxine index of 150% of normal. This is usually moderately well tolerated, although minor degrees of sweating, tachycardia (fast heartbeat), and other signs of hyperthyroidism can accompany this regimen. If this approach is employed, it is particularly important to increase the dose of T4 (Synthroid) very slowly because of its relatively long half-life—about 12 days. (That is, if a patient takes a high dose of T4 and then stops their medication completely, 12 days later blood levels will only have decreased to half of what they originally were.)
Findings about high-dose T4 for women with treatment-resistant bipolar illness after the jump. Read more
Smoking Multiplies Risks for Bipolar Patients
Smoking is associated with a less successful outcome in the naturalistic treatment of bipolar patients, reported Seetal Dodd and colleagues at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. Nicotine dependence has also been found to be a risk factor for depressive symptoms, as reported in a recent article in the British Journal of Psychiatry.
In addition to these direct effects on mental health, smoking is also a major risk factor for cardiovascular disease when combined with the presence of any three of the five primary risk factors that constitute the metabolic syndrome. (These five factors are: increased waist circumference, high blood pressure, increased cholesterol, increased triglycerides, and insulin resistance or elevated fasting blood glucose.) Cardiovascular disease co-occurs with bipolar disorder at a high rate and is one of the major causes of decreased life expectancy in those with inadequately treated illness.
Because smoking is a powerful risk factor for comorbid illnesses such as heart attack and stroke and is itself associated with a poor clinical outcome in the treatment of bipolar disorder, every effort should be made to help patients with smoking cessation. Suggestions after the jump. Read more
Carbamazepine Extended Release Has Mixed Effects in Bipolar Children
In a poster presentation at the Pediatric Bipolar Conference in Cambridge, Massachusetts in March, Gagin Joshi from Massachusetts General Hospital (MGH) presented positive data from a study on the use of carbamazepine extended release (Equetro) in 27 children ages 6 to 12 with childhood-onset bipolar illness. These data were published this year in the Journal of Child and Adolescent Psychopharmacology.
Joshi found substantial overall improvement using an average dose of 788 mg/day, achieving blood levels averaging 6.6 mcg/l. Surprisingly, antidepressant effects were as robust as antimanic effects.
Major side effects included headache in 23% of participants, gastrointestinal upset in 18%, sedation in 15%, and dizziness in 8%. However, eleven children dropped out of the study prematurely (two for rash, three for mania, three for lack of efficacy, and three who did not participate in follow up). Joshi felt that carbamazepine extended release was a useful backup strategy, but he was not overly impressed with its overall profile in children, in part because of the high dropout rate.
Treatments Studies for Childhood Onset Bipolar Illness Are Inadequately Funded
It was remarkable that at the Pediatric Bipolar Conference hosted by Massachusetts General Hospital (MGH) and the Ryan Licht Sang Bipolar Foundation this past March in Cambridge, Massachusetts, none of the plenary talks, although they were excellent and given by leaders in the field of child psychiatry, dealt directly with the topic of the conference–childhood-onset bipolar disorder. There were also no reports of systematic placebo-controlled clinical trials evaluating treatment approaches in any of the subsequent presentations or posters. A number of open and uncontrolled studies examined new treatment possibilities.
It is notable that the National Institute of Mental Health (NIMH) no longer sponsors this conference, as it did for many years. Moreover, STEP-BD, an NIMH-sponsored research program on the course and treatment of adult-onset bipolar disorder, is now defunct, and the head of STEP-BD and one of the most productive researchers in bipolar illness, Andrew Nierenberg from the MGH, has been forced to search for other funding opportunities.
These developments highlight the ongoing deficient funding and study of both childhood-onset and adult-onset bipolar disorder despite the enormous public health impact, extraordinary morbidity, and early mortality from suicide and medical illnesses like cardiovascular disease that are associated with these disorders.
Help the Child and Adolescent Bipolar Foundation win $250,000!
The Child and Adolescent Bipolar Foundation (CABF) has launched a campaign for votes to win the Pepsi Refresh Project and a $250,000 grant to aid families and children living with bipolar disorder and depression. CABF has been chosen to compete for the top grant during the month of November. Winners are decided by total votes cast via Internet and text messages throughout the month.
If selected by popular vote, CABF will use an innovative
social media awareness effort to:
- Elevate awareness about bipolar disorder & depression in children;
- Educate parents & the public about the symptoms;
- Explain the best treatment options & ways to reduce teen suicide;
- Expand the number of children receiving treatment;
- Eliminate the stigma associated with mental illness;
- Extend hope to families struggling with mental illnesses.
Supporters can vote for CABF 3 times a day, once from
each of the following sources:
1. Pepsi Refresh website
2. Facebook
3. Texting – Text 104174 to PEPSI (73774) (Normal text
rates apply).
Psychotherapy Necessary for Bipolar Disorder and Severe Mood Dysregulation in Children
 Dr. Janet Wozniak of Massachusetts General Hospital initiated a survey, both at MGH and in the field, to ascertain practitioners’ experience with individual and family psychotherapeutic and educational approaches to childhood-onset bipolar illness. These types of approaches appear fundamental to treating children or families in which there is bipolar illness.
Dr. Janet Wozniak of Massachusetts General Hospital initiated a survey, both at MGH and in the field, to ascertain practitioners’ experience with individual and family psychotherapeutic and educational approaches to childhood-onset bipolar illness. These types of approaches appear fundamental to treating children or families in which there is bipolar illness.
It was the view of Wozniak, her survey, and many other investigators in attendance at the Pediatric Bipolar Conference in Cambridge, Massachusetts in March that such psychotherapeutic approaches are needed, and often recommended, but the availability of effective treatment and of therapists skilled in administering any of these psychotherapies in children is often lacking.