Dopamine D2 and D3 Agonist Pramipexole May Enhance Cognitive Function in Bipolar I Disorder
Anil Malhotra from the Zucker Hillside Hospital found that pramipexole (Mirapex), a dopamine D2 and D3 agonist used in the treatment of Parkinson’s disease, improved measures of processing speed and working memory in euthymic bipolar patients (whose average age was 42) when compared with placebo in an adjunctive clinical trial.
Editor’s Note: Bipolar patients in a euthymic phase have consistently been shown to have some degree of cognitive dysfunction that is typically correlated with the number of prior depressive and/or manic episodes they have experienced. This is one of the first studies to directly target this cognitive dysfunction with a pharmacotherapeutic agent.
Pramipexole may be of additional value among depressed patients, because in two small, placebo-controlled studies, one led by Carlos Zarate at the National Institute of Mental Health and one led by Joseph F. Goldberg in New York, pramipexole has been shown to exert acute antidepressant effects in bipolar patients in the depressive phase of the illness. The new data from Malhotra raise the possibility that there could be a two-for-one benefit when pramipexole is used in the depressive phase of bipolar illness—improvement in both depression and cognition.
Other approaches to improving cognition in patients with bipolar disorder
Inflammation and Oxidative Stress in Bipolar Disorder
A number of studies presented at the 4th Biennial Conference of the International Society for Bipolar Disorders conference in Sao Paulo, Brazil in March reported new data relevant to inflammation and oxidative stress. Both inflammation and oxidative stress increase risk of cardiovascular disorders, and patients with inadequately treated mood disorders lose 10 or more years of life expectancy from cardiovascular disorders compared to the general population. Inflammation and oxidative stress may also contribute to the symptoms, evolution, and progression of the mood disorders themselves.
It is possible that these two processes could become new targets for therapeutic intervention in addition to more traditional psychopharmacological drugs that primarily target the neurotransmitters dopamine, norepinephrine, serotonin, and the neurotrophic factor BDNF. Read more
Environmental Influences on Gene Structure May Be Transmitted to Offspring
It has been thought that one fundamental principle of genetics is that the impact of environment factors cannot be passed from one generation to the next via the genetic code. New data suggest this may not be true.
In an emerging field called epigenetics, researchers are finding that while the impact of environment and life experiences is not registered in DNA sequences, environmental factors can influence the structure of DNA or tightness of its packaging. Early life experiences, particularly psychosocial stress, can lead to the accumulation of methyl groups on DNA (a process called methylation), which generally constricts DNA’s ability to start transcription (turning on) of genes and the synthesis of the proteins the genes encode. DNA is tightly wound around proteins called histones, which can also be methylated or acetylated based on events in the environment. When histones are acetylated, meaning that acetyl groups are attached to them, DNA is wound around them more loosely, facilitating gene transcription (i.e. the reading out of the DNA code into messenger RNA, which then arranges amino acids in order to construct proteins). Conversely, histone methylation usually tightens the winding of DNA and represses transcription.
Episodic vs. Continuous Social Stress Result in Different Rates of Cocaine Use
In a study of rodents exposed to stress (by being forced to enter another rodent’s territory) and given the opportunity to self-administer cocaine, those exposed to a few brief episodes of stress increased their cocaine use and engaged in binge-like episodes, while those exposed to stress chronically showed suppressed cocaine use.
At the American College of Neuropsychopharmacology meeting in December 2009, Klaus Miczek and colleagues from Tufts University in Boston presented a fascinating study indicating that the temporal aspects of the experience of social stress may have dramatic impact not only on defeat stress behaviors and the associated biochemistry, but also on the likelihood that an animal adopts cocaine self-administration. These investigators compared episodic versus chronic defeat stress in rodents.
Episodic social defeat stress consisted of four brief confrontations between an intruding animal and an aggressive resident rat over the course of a period of ten days. In contrast, chronic subordination stress involved the continuous exposure of the intruder rat to an aggressive resident over five weeks, during which time the intruder lived in a protective cage within the resident’s home cage.
The episodically defeated intruder rats showed increases in intravenous cocaine self-administration and prolonged binge-like episodes, along with increases in brain-derived neurotropic factor (BDNF), which is necessary for long-term learning and memory, in the midbrain ventral-tegmental area (VTA) and increased dopamine release in the nucleus accumbens, the reward area of the brain. In contrast, the continuously subordinate rats showed the opposite pattern of suppressed cocaine intake, suppression of dopamine release in the n. accumbens, and reduced BDNF in the VTA.
Quetiapine is Effective Across a Spectrum of Illnesses
The atypical antipsychotic quetiapine (Seroquel or Seroquel XR) has a range of efficacy in a number of illnesses, depending on the size of the dose given. Read about some of its uses below, including as an adjunct to antidepressants in unipolar depression; as a treatment for generalized anxiety disorder (GAD) and post-traumatic stress disorder (PTSD); and, at higher doses, as a treatment for mania and depression. Some of its potential mechanisms of action are described as well.
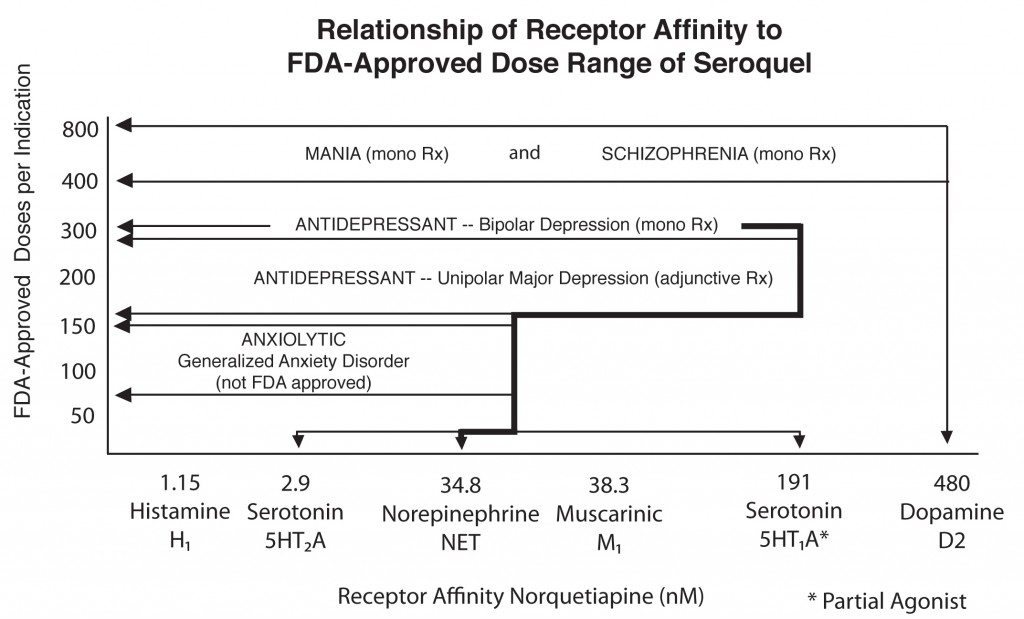
Quetiapine's actions on various receptors in the brain (bottom axis) are responsible for its effects in different illnesses
Quetiapine as an adjunct to antidepressants in unipolar depression
Posters at the American Psychiatric Association meeting in San Francisco in May 2009 showed new data from a series of studies of quetiapine in unipolar depression that showed the drug in monotherapy (at 150mg & 300mg) was significantly more effective than placebo. Studies were also positive when quetiapine was used as an adjunct compared with placebo for patients showing inadequate or incomplete responses to antidepressants such as selective serotonin reuptake inhibitors (SSRIs).
Read more


