BDNF in Learning and Memory
Brain-derived neurotrophic factor (BDNF) is involved in various aspects of learning and memory. The DNA for BDNF contains nine different regulatory sites, each of which is involved in different aspects of learning. Researcher Keri Martinovich studied each site by selectively knocking each one out with a genetic manipulation. She found that blocking the e1 site increased acquisition of new learning and recall in mice, while e2 did the opposite. Blockade of e4 had no effect on these memory functions but markedly blocked the process of extinction, which involves a different kind of new learning.
A mouse that learned to associate a particular cue with a shock (a process known as conditioned fear) will stop reacting to the cue after it is presented many times without a shock. This learning that the cue is no longer associated with the shock is referred to as extinction. The animals with e4 blocked in their BDNF did not develop the new extinction learning, and continued to react to the cue as if it were still associated with the shock.
Editor’s Note: These data may have clinical relevance for humans. The anticonvulsant valproate (trade name Depakote), a histone deacetylase inhibitor, selectively increases the e4 promoter site of BDNF and facilitates extinction of conditioned fear, according to research by Tim Bredy et al. published in 2010.
Clinical trails should examine whether valproate could enhance fear extinction in patients with post-traumatic stress disorder (PTSD).
A Common Variant of BDNF Predicts Non-Response to IV Ketamine
Brain-derived neurotrophic factor (BDNF) is a protein in the brain that protects neurons and is necessary for long-term memory and learning. Different people have different genetic variations in BDNF depending on which amino acid the gene that codes for it inserts into the protein, valine or methionine. There are three possible combinations that vary in their efficiency. The Val66Val allele of BDNF is the most efficient for secreting and transporting BDNF within the cell body to synapses on dendrites, and is also a risk factor for early onset of bipolar disorder and rapid cycling. Twenty-five percent of the population has a Met variant (either Val66Met or Met66Met), which functions less efficiently. These people have mild decrements in some cognitive processing.
Increases in BDNF are necessary to the antidepressant effects of intravenous ketamine. In animals, ketamine also rapidly changes returns dendritic spines that had atrophied back to their healthy mushroom shape in association with its antidepressant effects. According to research published by Gonzalo Laje and colleagues in the journal Biological Psychiatry in 2012, depressed patients with the better functioning Val66Val allele of BDNF respond best to ketamine, while those with the intermediate functioning Val66Met allele respond less well.
Researcher Ronald S. Duman of Yale University recently found that increases in BDNF in the medial prefrontal cortex are necessary to the antidepressant effects of ketamine. If antibodies to BDNF (which block its effects) are administered to the prefrontal cortex, antidepressant response to ketamine is not observed.
Duman also found that calcium influx through voltage sensitive L-type calcium channels is necessary for ketamine’s antidepressant effects. A genetic variation in CACNA1C, a gene that codes for a subunit of the dihydropiridine L-type calcium channel, is a well-replicated risk factor for bipolar disorder. One might predict that those patients with the CACNA1C risk allele, which allows more calcium influx into cells, would respond well to ketamine.
BDNF Is Decreased in Depression and Mania
Brain-derived neurotrophic factor (BDNF), which protects neurons and is necessary for long-term memory, can be measured in blood. In a symposium on bipolar disorder at the 2012 meeting of the Society of Biological Psychiatry, researcher Flavio Kapsczinski reviewed evidence from several meta-analyses showing that low levels of BDNF in the blood correlate with severity of an episode of depression or mania. In addition to the findings that BDNF levels are low during a mood episode, there are other reliable biomarkers of illness, including increases in intracellular calcium, increases in cortisol and failure to suppress cortisol by dexamethasone, and a variety of indices of inflammation and oxidative stress.
There are several common variants of the gene responsible for the production of BDNF, depending on which types of amino acids appear in its coding—valine or methionine. The Val66Val allele of proBDNF is the most frequently occurring in the population, and is the best-functioning variant. Those with a methionine substitution (Val66Met or Met66Met) have less efficient forms of BDNF. Researcher Jair Soares reported that the Met allele was associated with deficits in declarative memory in patients with bipolar disorder, and was also associated with smaller volume of the anterior cingulate gyrus.
Researcher Ghanshyam N. Pandey reported that patients with pediatric or adult bipolar disorder had decreased BDNF protein and mRNA levels in platelets and lymphocytes compared to controls. Treatment significantly increased these BDNF levels in the pediatric, but not in the adult bipolar subjects. These measurements in blood are consistent with findings that there are decreases in BDNF in the hippocampus and prefrontal cortex of patients who died while depressed or who committed suicide compared to controls.
Inflammatory Markers May Predict Antidepressant Response
There appears to be a link between inflammation and depression. In the journal Neuropsychopharmacology, Cattanes et al. reported in 2013 that compared to controls, depressed patients had significantly higher baseline levels of inflammatory cytokines, less glucocorticoid receptor function, less neuroplasticity, and fewer neuroprotective factors. Certain variables predicted response to treatment, others were seen only in responders, and still others changed in everyone with antidepressant treatment.
Higher baseline levels of inflammatory markers interleukin IB, macrophage inhibitory factor (MIF), and tumor necrosis factor TNF? were each associated with nonresponse to antidepressant treatment, and the three combined accounted for 50% of the variance in response—that is, they were the major predictor of whether a patient responded to treatment.
Levels of other factors changed in only those patients who responded well to antidepressants. The biggest changes were the normalization in levels of the neurotrophic factors BDNF and VEGF.
Several other markers normalized with antidepressant treatment regardless of whether the patients responded to treatment, and these included decreases in cytokines interleukin-IB and MIF and improved glucocorticoid receptor function.
The three different kinds of findings about these biomarkers were observed regardless of what type of antidepressant was used—SSRI versus tricyclic nortriptyline (which blocks norepinephrine reuptake).
Editor’s Note: This study replicates other studies in depression where signs of inflammation have been observed, including increases in inflammatory cytokines, decreases in glucocorticoid receptor function (needed to suppress high levels of the stress hormone cortisol) and lower levels of neuroplasticity and neuroprotection markers. This, however, is one of the first studies to show that levels of these markers at baseline may predict response to antidepressant treatment.
Also novel are the findings that while some high interleukin levels at baseline predicted antidepressant non-response, other ones normalized only in responders, and still others changed with treatment independent of whether the patients’ depression improved. These exciting findings require replication, but suggest the future possibility of personalized medicine, that is, choosing medications based on an individual biochemical marker profile. Eventually direct use of anti-inflammatory agents may be necessary in those with the highest levels of cytokines (predicting non-response to conventional antidepressant treatment). The same types of studies are needed in bipolar depression to determine the relationship between these inflammatory markers and treatment response.
Ginkgo Biloba Improves Tardive Dyskinesia
 Tardive dyskinesia is a sometimes irreversible side effect of antipsychotic treatment, and is characterized by uncontrollable, subtle and spontaneous motor movements, usually of the tongue, mouth, or fingers.
Tardive dyskinesia is a sometimes irreversible side effect of antipsychotic treatment, and is characterized by uncontrollable, subtle and spontaneous motor movements, usually of the tongue, mouth, or fingers.
Extracts of the leaves of the gingko biloba tree contain potent antioxidants. In a study published by Zhang et al. in the journal Biological Psychiatry in 2012, treatment with ginkgo biloba (EGb-761) at 240mg/day for 12 weeks improved tardive dyskinesia more than placebo. Patients with tardive dyskinesia had low levels of brain-derived neurotrophic factor (BDNF) at baseline, and gingko biloba increased these levels. BDNF is important for the production and protection of neurons, and maintaining long-term memory.
The increase in BDNF was correlated with the degree of improvement achieved with gingko biloba in these patients. Different people have different variations in the gene for BDNF. As a result, some people’s BDNF is transported to dendrites and synapses more efficiently than others’. Improvement was greatest in those patients with the most common and best-functioning variant of BDNF, Val66Val, and worst in those patients with the rare and poorest-functioning variant, Met66Met.
Editor’s Note: These findings could be of great clinical importance. Tardive dyskinesia occurred in 20 to 40% of patients with bipolar disorder following treatment with the older “typical” antipsychotics. The incidence is much lower with the newer “atypical” antipsychotics, but having an effective and well-tolerated treatment for this disfiguring side effect is an extra bonus.
How Illness Progresses In The Recurrent Affective Disorders
This editor (RM Post) in collaboration with Jacqueline Fleming and Flavio Kapczinski published the article “Neurobiological mechanisms of illness progression in the recurrent affective disorders” in the Journal of Psychiatric Research this year. The article built on several themes about the progression of bipolar illness that had been explored in previous research.
These themes include:
- The likely acceleration of repeated episodes as a function of the number of prior episodes (episode sensitization)
- The increased responsivity of the illness to repeated stressors (stress sensitization)
- The increased behavioral reactivity to repeated use of psychomotor stimulants such as cocaine (stimulant-induced behavioral sensitization)
Not only are these observations well documented in the scientific literature, but recent observations also suggest that each type of sensitization can show cross-sensitization to the other two types. That is, individuals exposed to repeated stressors are more likely both to experience affective illness episodes and to adopt comorbid substance abuse. In a similar way, episodes of an affective disorder and stressors may also be associated with the relapse into drug administration in those who have been abstinent.
In addition to these mechanisms of illness progression in the recurrent affective disorders, the new article reviews the literature showing that the number of affective episodes or the duration of the illness appear to be associated with a variety of other clinical and neurobiological variables.
The number of affective episodes a patient experiences is associated with the degree of cognitive dysfunction present in their bipolar illness, and experiencing more than 4 episodes of unipolar or bipolar depression is a risk factor for dementia in late life. A relative lack of response to most treatments is also correlated with the number of prior episodes, and this holds true for response to naturalistic treatment in general. While most of these data are correlational and the direction of causality cannot be ascertained for certain, it is likely that the number of affective episodes and/or their duration could account for and drive difficulties with treatment and with cognitive function.
If this were the case, one would expect to see a variety of neurobiological correlates with the number of prior episodes or duration of illness, and in the article we summarize those that have been found in unipolar and bipolar disorder. Considerable data indicate that cortical volume and degrees of prefrontal cortical dysfunction can vary as a function of number of prior episodes. There is evidence that increased activity of the amygdala and the nucleus accumbens are also related to episodes or duration of illness. In those with unipolar depression, the volume of the hippocampus is decreased with longer duration of illness. Read more
Genetic Markers of Response to Lithium
 At the 5th Biennial Conference of the International Society for Bipolar Disorders and the 67th Annual Meeting of the Society of Biological Psychiatry, John Kelsoe presented his research on personalized pharmacotherapy for bipolar disorder, describing genetic predictors of response to lithium.
At the 5th Biennial Conference of the International Society for Bipolar Disorders and the 67th Annual Meeting of the Society of Biological Psychiatry, John Kelsoe presented his research on personalized pharmacotherapy for bipolar disorder, describing genetic predictors of response to lithium.
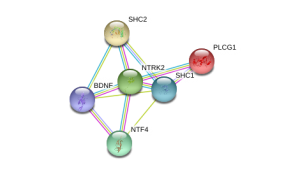
In his research Kelsoe found that a variant of the gene that codes for neurotrophic receptor type II (NTRK2), the receptor for brain-derived neurotrophic factor (BDNF), was associated with good response to lithium in patients with a family history of bipolar disorder or a history of euphoric mania. The “T” allele of rs1387923 was associated with better response to lithium retrospectively, and these results were replicated in a prospective study.
Editors Note: These data are among the first to indicate that genetic information could be used to make treatment decisions. Lithium increases BDNF and neurogenesis, thus it makes some sense that a variation in the BDNF receptor would affect clinical responsiveness to lithium.
In a similar vein, Janusz K. Rybakowski reported at the Society of Biological Psychiatry meeting on another possible predictor of long-term excellent response to lithium in bipolar disorder. Due to normal genetic variation, different people have different versions of BDNF. Rybakowski found that the patients with a version of BDNF known as Val66Val who had bipolar disorder performed significantly better on the Wisconsin Card Sorting Test, which evaluates abstract reasoning. However, he found that patients with a methionine amino acid in the place of one of the valine amino acids (resulting in a Val66Met allele, which is associated with minor cognitive difficulties) showed significantly better response to preventative treatment with lithium. It is noteworthy that these excellent lithium responders also performed better on a complex neuropsychological battery than those who were less good responders to lithium. The good responders’ performance on these tests was not different from healthy controls.
Editor’s Note: These data add to the possibility that prediction of lithium response is linked to common gene variations in neuroprotective factors or their receptors. It is interesting that the patients with the Val66Met allele, which works less efficiently, show the best long-term response to lithium. This is consistent with the view that lithium, which increases BDNF, is most effective in those who have a sluggish functioning of their BDNF due to having the Met allele. As we have written before, those with the Met allele have slight decrements in working memory, and in animal models, those with the Met allele show deficits in long-term potentiation (LTP), which suggest problems with long-term memory. Thus, using lithium to increase BDNF function in those with a “sluggish” variation in their BDNF makes sense and may ultimately be clinically useful.
Exercise and Brain Health: Some Good Points to Remember
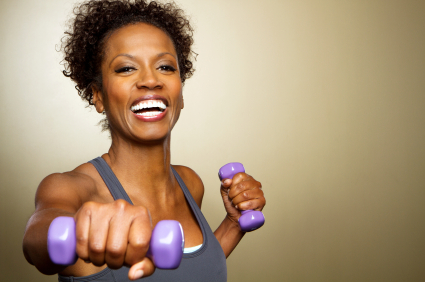
In a review article in the Neuroscientist published in February of this year, Kirk I. Erickson and collaborators wrote that “[m]ajor depressive disorder is considered a risk factor for Alzheimer’s dementia and memory impairment and is associated with less BDNF and greater hippocampal atrophy, possibly through a BDNF pathway. However, exercise and effective treatment for geriatric depression increases BDNF levels, increases serotonin fibers, is associated with greater hippocampal volumes, and reduces the risk for Alzheimer’s dementia.”
Editor’s note: Not a bad set of benefits from exercise! The researchers suggest that exercise is extremely important in reversing the decreases in brain-derived neurotrophic factor (BDNF) associated with depression, helping to improve depressed mood, increasing cardiovascular fitness, and maintaining healthy cognition.
Hippocampal volume and BDNF levels in blood both decrease with age. Yet exercise increases both BDNF and the formation of new neurons (neurogenesis) in animals. New data in humans suggest that aerobic fitness is associated with the size of the hippocampus, both in both children and adults. It is not clear yet whether this increase in hippocampal volume is directly driven by increases in BDNF and/or neurogenesis. However, since a smaller hippocampus is a risk factor both for depression and for mild cognitive impairment progressing to Alzheimer’s dementia, attempting to enhance hippocampal volume in any way possible is probably a good idea.
Methods of increasing hippocampal volume include treatment with antidepressants or with lithium. In the 2012 paper Erickson and collaborators also wrote, “Anaerobic exercise enhances executive and memory function and reduces hippocampal atrophy in late adulthood, and this may be partially mediated through a BDNF pathway.”
Erickson and collaborators conducted a longitudinal study published in 2010 that quantified the amount of physical activity subjects engaged in by calculating the total number of blocks walked per week. Individuals reporting greater amounts of physical activity at the beginning of the study had, upon examination nine years later, greater gray matter volume in several parts of the brain, including the hippocampus. This effect was “dose-dependent,” meaning that only those individuals who walked at least 72 blocks per week (roughly equivalent to 1 mile per day) had significant sparing of brain tissue nine years later. The study found increased gray matter volume in the prefrontal cortex and in the temporal lobe.
After a further follow-up of four more years, greater gray matter volume with physical activity was associated with a two-fold reduced risk of cognitive impairment. The researchers concluded that “physical activity patterns earlier in life were linked to brain volume and cognitive impairment later in life.”
There are a number of important points to remember about cognitive impairment. One is that increasing hippocampal volume and preventing its decrement with aging may help prevent age-related memory loss and potentially the rapidity at which mild cognitive impairment progresses. Read more
Common Genetic Variation Linked to Response to Antidepressants
 Brain-derived neurotrophic factor (BDNF) protects neurons and is important for long-term learning and memory. There are several genetic variations in BDNF depending on which amino acid—valine or methionine—falls at a particular position when the proBDNF protein is being made. Most people have the val-66-val allele, some have the val-66-met, and a few have the met-66-met allele.
Brain-derived neurotrophic factor (BDNF) protects neurons and is important for long-term learning and memory. There are several genetic variations in BDNF depending on which amino acid—valine or methionine—falls at a particular position when the proBDNF protein is being made. Most people have the val-66-val allele, some have the val-66-met, and a few have the met-66-met allele.
Researcher Jessica C. Levenson, working with David Kupfer and Ellen Frank at the University of Pittsburgh, reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 that patients with unipolar depression who have the val-66-val allele of proBDNF have better clinical responsiveness to antidepressants than those with the slightly less common variant, val-66-met.
Editor’s note: The val-66-val allele is more effective in enhancing synaptic plasticity and is more easily transported from the nucleus to the dendrites of neurons (where it is necessary for learning and memory) than the val-66-met allele or the least effective met-66-met variant.
These findings are intriguing because antidepressant treatments tend to increase BDNF, regardless of their mechanisms of action. Moreover, BDNF levels are low in patients with depression, usually in direct relationship to the severity of depression. Thus, the ability of antidepressants to increase BDNF may lead to a more effective treatment response in those with the better functioning val-66-val allele of BDNF. This remains to be further documented, but the study provides a preliminary example of how genotyping may eventually be able to help predict individual clinical response to a given treatment and thus foster the development of personalized medicine.
BDNF Related to Cognition and Fitness in Men with Coronary Artery Disease
 At the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011, Walter Swardfager and colleagues from Toronto, Ontario presented a study indicating that brain-derived neurotrophic factor (BDNF) concentrations in blood are associated with cognitive performance and cardiopulmonary fitness in people with coronary artery disease.
At the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011, Walter Swardfager and colleagues from Toronto, Ontario presented a study indicating that brain-derived neurotrophic factor (BDNF) concentrations in blood are associated with cognitive performance and cardiopulmonary fitness in people with coronary artery disease.
In 88 mostly male subjects with a mean age of 63 years, cardiopulmonary fitness was directly correlated with BDNF in blood as well as higher scores of cognition on two tests, the mini mental status exam and the digit symbol coding task. The investigators concluded that better fitness, psychomotor processing speed, and overall cognition were consistent with a hypothesis that BDNF protects midbrain dopaminergic neurons against inflammatory neurodegenerative processes.
Blood levels of interleukin 6, a measure of inflammatory cytokines, were associated with lower mini mental status scores in a multivariate analysis that controlled for BDNF levels.
Editor’s note: BDNF appears to be necessary for long-term learning and memory. Meta-analyses indicate that BDNF levels are low in depression and improve with euthymia. Many mood stabilizers including lithium, valproate, carbamazepine, and lamotrigine and most types of antidepressants are able to increase BDNF. The current findings linking BDNF with better cardiopulmonary fitness and cognition continue to emphasize the potential importance of BDNF beyond its role as a marker for depression.
In BNN Volume 12, Issue 3 from 2008, we reported on the data of Schmidt and Duman, which indicated that BDNF administered in a subcutaneous minipump is able to reverse many depressive-like behaviors in an animal model of depression, suggesting that even peripheral BDNF may have a role in the central nervous system.