Lamotrigine potentiates the antidepressant effects of quetiapine in bipolar depression
At the 2015 meeting of the International Society for Bipolar Disorders, researcher John Geddes presented an important study showing in inadequate responders to quetiapine that compared to adding placebo, adding the anticonvulsant lamotrigine to their treatment improved depression rapidly and lastingly. Some psychiatrists have been prescribing this combination to patients for some time, but this is the first formal clinical trial documenting its efficacy. The article was published online in December in the journal Lancet Psychiatry.
Researcher Guy Goodwin described details of the study, called CEQUEL, at the meeting. It included 202 patients with bipolar I or II disorder who required treatment for a depressive episode. Participants who did not respond completely to 14 days of treatment with quetiapine were prescribed either an additional dose of lamotrigine or a placebo. Lamotrigine was very slowly titrated up to maximum doses of 200mg/day. Its antidepressant effects were striking. They began early and persisted for 50 weeks. (The published article covers only the first 12 weeks.) Response rates for the combination of quetiapine and lamotrigine were 52%, compared to 22% for quetiapine alone. Remission rates were 35% for quetiapine and lamotrigine and 12% for quetiapine alone.
Folic acid interaction
Another part of the study assessed whether folic acid supplements could improve outcomes, but in fact they did the opposite, reversing the benefits of adding lamotrigine. Geddes did not have an explanation for why this might be the case. Lamotrigine can inhibit folate metabolism, and it had been thought that adding folate would be useful. Until further data are gathered on folate augmentation in patients taking the combination of lamotrigine and quetiapine, folate should be used cautiously if at all in these patients.
Possible combination with lithium
In Goodwin’s talk, he also noted lithium’s potential to lower suicide rates, premature mortality, and cognitive impairment, and to increase hippocampal and cortical volume.
Since lamotrigine was shown to potentiate the antidepressant effects of lithium in a study by Van der Loos and colleagues, and quetiapine is approved by the Food and Drug Administration for the prevention of depression as an adjunct to lithium (or valproate), there might be theoretical acute and long-term benefits to combining the three: lithium, quetiapine, and lamotrigine.
Reduced Cognitive Function and Other Abnormalities in Pediatric Bipolar Disorder
 At the 2015 meeting of the International Society for Bipolar Disorders, Ben Goldstein described a study of cognitive dysfunction in pediatric bipolar disorder. Children with bipolar disorder were three years behind in executive functioning (which covers abilities such as planning and problem-solving) and verbal memory.
At the 2015 meeting of the International Society for Bipolar Disorders, Ben Goldstein described a study of cognitive dysfunction in pediatric bipolar disorder. Children with bipolar disorder were three years behind in executive functioning (which covers abilities such as planning and problem-solving) and verbal memory.
There were other abnormalities. Youth with bipolar disorder had smaller amygdalas, and those with larger amygdalas recovered better. Perception of facial emotion was another area of weakness for children (and adults) with bipolar disorder. Studies show increased activity of the amygdala during facial emotion recognition tasks.
Goldstein reported that nine studies show that youth with bipolar disorder have reduced white matter integrity. This has also been observed in their relatives without bipolar disorder, suggesting that it is a sign of vulnerability to bipolar illness. This could identify children who could benefit from preemptive treatment because they are at high risk for developing bipolar disorder due to a family history of the illness.
There are some indications of increased inflammation in pediatric bipolar disorder. CRP, a protein that is a marker of inflammation, is elevated to a level equivalent to those in kids with juvenile rheumatoid arthritis before treatment (about 3 mg/L). CRP levels may be able to predict onset of depression or mania in those with minor symptoms, and is also associated with depression duration and severity. Goldstein reported that TNF-alpha, another inflammatory marker, may be elevated in children with psychosis.
Goldstein noted a study by Ghanshyam Pandey that showed that improvement in pediatric bipolar disorder was related to increases in BDNF, a protein that protects neurons. Cognitive flexibility interacted with CRP and BDNF—those with low BDNF had more cognitive impairment as their CRP increased than did those with high BDNF.
Offspring of Parents with Psychiatric Disorders At Increased Risk for Disorders of Their Own
At a symposium at the 2015 meeting of the International Society for Bipolar Disorder, researcher Rudolph Uher discussed FORBOW, his study of families at high risk for mood disorders. Offspring of parents with bipolar disorder and severe depression are at higher risk for a variety of illnesses than offspring of healthy parents.
Uher’s data came from a 2014 meta-analysis by Daniel Rasic and colleagues (including Uher) that was published in the journal Schizophrenia Bulletin. The article described the risks of developing mental illnesses for 3,863 offspring of parents with schizophrenia, bipolar disorder, or major depression compared to offspring of parents without such disorders.
Previous literature had indicated that offspring of parents with severe mental illness had a 1-in-10 likelihood of developing a severe mental illness of their own by adulthood. Rasic and colleagues suggested that the risk may actually be higher—1-in-3 for the risk of developing a psychotic or major mood disorder, and 1-in-2 for the risk of developing any mental disorder. An adult child may end up being diagnosed with a different illness than his or her parents.
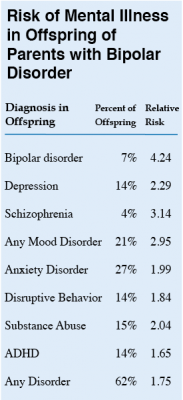 At the symposium, Uher focused on families in which a parent had bipolar disorder. These families made up 1,492 of the offspring in the Rasic study. The table at right shows the risk of an illness among the offspring of bipolar parents compared to that risk among offspring of healthy parents, otherwise known as relative risk. (For example, offspring of parents with bipolar disorder are 4.24 times more likely to be diagnosed with bipolar disorder themselves than are offspring of non-bipolar parents.) The table also shows the percentage of offspring of parents with bipolar disorder who have each type of disorder.
At the symposium, Uher focused on families in which a parent had bipolar disorder. These families made up 1,492 of the offspring in the Rasic study. The table at right shows the risk of an illness among the offspring of bipolar parents compared to that risk among offspring of healthy parents, otherwise known as relative risk. (For example, offspring of parents with bipolar disorder are 4.24 times more likely to be diagnosed with bipolar disorder themselves than are offspring of non-bipolar parents.) The table also shows the percentage of offspring of parents with bipolar disorder who have each type of disorder.
Editor’s Note: These data emphasize the importance of vigilance for problems in children who are at increased risk for mental disorders because they have a family history of mental disorders. One way for parents to better track mood and behavioral symptoms is to join our Child Network.



