An Inflammatory State Impedes Treatment for Bipolar Disorder
 A 2017 study by in the Journal of Clinical Psychiatry links inflammation to a poor antidepressant response in bipolar disorder. Many previous studies have found that elevated inflammatory markers are common in mood disorders, and that an inflammatory state seems to prevent response to certain therapies.
A 2017 study by in the Journal of Clinical Psychiatry links inflammation to a poor antidepressant response in bipolar disorder. Many previous studies have found that elevated inflammatory markers are common in mood disorders, and that an inflammatory state seems to prevent response to certain therapies.
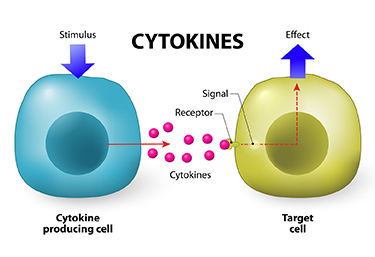
Researcher Francesco Benedetti and colleagues report that high levels of inflammatory cytokines (a type of small proteins) predicted a worse response to treatment with sleep deprivation and light therapy for bipolar depression. This treatment typically brings about a rapid antidepressant response.
Benedetti and colleagues measured 15 immune-regulating compounds in 37 patients who were experiencing an episode of bipolar depression and 24 healthy volunteers. Among those participants with bipolar disorder, 84% had a history of non-response to medication. Twenty-three of the 37 patients, or 62%, responded to the sleep deprivation/light therapy combination. Those who did not had higher levels of five cytokines: interleukin-8, monocyte chemoattractant protein-1, interferon-gamma, interleukin-6, and tumor necrosis factor-alpha.
Body mass index was correlated with cytokine levels and also reduced response to the treatment.
The finding supports a link between the immune system and mood disorders. Evaluating a patient’s level of inflammation may, in the future, allow doctors to predict the patient’s response to a given therapy. Patients with high levels of inflammation might benefit most from treatments that target their immune system.
Arthritis Drug Celecoxib May Improve Bipolar Depression When Paired with Escitalopram
A new study suggests that for people with bipolar depression, the anti-inflammatory drug celecoxib (Celebrex), typically used to treat arthritis, can boost the effectiveness of the antidepressant escitalopram (Lexapro).
In the 8-week study by researcher Angelos Halaris and colleagues, adults with bipolar depression were randomly assigned to one of two groups. The first group received the selective-serotonin reuptake inhibitor (SSRI) antidepressant escitalopram plus celecoxib to target inflammation. The second group received just the antidepressant escitalopram and a placebo.
By the end of the study, 78% of the group taking the anti-arthritis drug had seen major improvement in their depression, with 63% reporting that it had lifted completely. Meanwhile in the placebo group, only 45% reported major improvement, and 10% reported remission.
The group that received celecoxib with their escitalopram also began seeing improvement within one week of beginning treatment, instead of after four to six weeks, which is typical of antidepressant treatment.
Researchers think depression creates an immune response leading to chronic inflammation, which can upset the balance of neurotransmitters in the brain and make antidepressants less effective. Halaris suggests that reducing this inflammation with a drug like celecoxib can make antidepressants more effective.
The research was presented at the Fifth International Congress on Psychiatry and the Neurosciences and has not yet been published.
Vitamin D Supplementation May Not Be Effective in Bipolar Depression, But Is Still Worth Doing
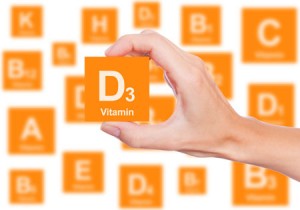 In some studies, vitamin D supplementation (1,500 IU/day) has been found to improve unipolar depression. Recently, researchers led by Wendy K. Marsh found that compared to placebo, 12 weeks of vitamin D3 supplementation (5,000 IU/day) did not produce greater improvement in depressive symptoms. The study, presented at the 2016 meeting of the Society of Biological Psychiatry, included 33 adult participants whose vitamin D levels remained deficient throughout the study.
In some studies, vitamin D supplementation (1,500 IU/day) has been found to improve unipolar depression. Recently, researchers led by Wendy K. Marsh found that compared to placebo, 12 weeks of vitamin D3 supplementation (5,000 IU/day) did not produce greater improvement in depressive symptoms. The study, presented at the 2016 meeting of the Society of Biological Psychiatry, included 33 adult participants whose vitamin D levels remained deficient throughout the study.
Editor’s Note: Caution is urged in interpreting this small study, especially because the participants did not achieve healthy levels of vitamin D.
Low levels of vitamin D are common in children and adults with bipolar disorder. Future research may explore whether raising vitamin D levels to healthy levels has a beneficial effect on mood. There are many other benefits to vitamin D supplementation. It can improve cognition, regulate calcium and phosphorus absorption, and maintain healthy bones and teeth. It may also protect against diseases such as cancer, type 1 diabetes, multiple sclerosis, rheumatoid arthritis, and Crohn’s disease. Improved cardiovascular health is also a possible benefit of vitamin D supplementation.
Treatment with Hormone EPO Improved Cognition in People with Unipolar and Bipolar Disorder
People with unipolar depression and bipolar disorder may experience cognitive difficulties, even when they’re not currently depressed. In a study published in the journal European Neuropsychopharmacology in 2016, researchers led by Caroline Vintergaard Ott determined that treatment with the hormone erythropoietin (EPO) may help. EPO is produced in the kidney and increases the production of hemoglobin and red cells.
Seventy-nine participants with unipolar or bipolar disorder were randomized to receive infusions of either EPO or a saline solution once a week for eight weeks. By the end of the study, those who received EPO showed significant improvements in the speed of their complex cognitive processing compared to those who received saline. EPO is known to induce the production of red blood cells. The improvements in processing speed lasted for at least another six weeks after red blood cell production would have normalized.
Those participants who received EPO not only had improved scores on tests of processing speed, they also reported fewer cognitive complaints. The EPO treatment was most likely to be effective in participants who had more impaired cognition at the beginning of the study.
In previous research by the same research group presented by Kamilla W. Miskowiak at the 2014 meeting of the International Society of Bipolar Disorders, EPO also improved sustained attention and recognition of happy faces.
Meta-Analysis Shows Anti-Inflammatory Treatments Improve Bipolar Depression
 It has been clear for some time that depression and inflammation are linked. This has led researchers to explore a variety of anti-inflammatory agents to treat depression. A meta-analysis of studies examining anti-inflammatory treatments for bipolar depression was published in the journal Bipolar Disorders in 2016.
It has been clear for some time that depression and inflammation are linked. This has led researchers to explore a variety of anti-inflammatory agents to treat depression. A meta-analysis of studies examining anti-inflammatory treatments for bipolar depression was published in the journal Bipolar Disorders in 2016.
Researcher Joshua D. Rosenblat and colleagues identified eight randomized controlled trials that met their criteria for anti-inflammatory treatments of bipolar disorder. These treatments included nonsteroidal anti-inflammatory drugs (NSAIDs such as ibuprofen and aspirin), omega-3 fatty acids, the antioxidant N-acetylcysteine, and pioglitazone (used to treat diabetes). Overall, the anti-inflammatory treatments had a moderate and statistically significant antidepressant effects. No serious side effects were reported, and the anti-inflammatory treatments did not cause a switch into mania in any of the participants.
The diversity of the anti-inflammatory treatments reviewed in this meta-analysis limit the extent to which it can be interpreted, but it is clear that more research on anti-inflammatory treatments for bipolar depression is needed. An open question is whether patients with particularly elevated levels of inflammatory markers in their blood would respond better to these anti-inflammatory treatments.
Methylene Blue May Help Bipolar Depression
 We have previously reported on the research by Martin Alda and colleagues that the chemical compound methylene blue had positive effects in patients with bipolar depression. The research was published in the British Journal of Psychiatry in 2016.
We have previously reported on the research by Martin Alda and colleagues that the chemical compound methylene blue had positive effects in patients with bipolar depression. The research was published in the British Journal of Psychiatry in 2016.
Now a new article by Ashley M. Feen and colleagues in the Journal of Neurotrauma reports that methylene blue has an antidepressant-like effect in mice with traumatic brain injury (TBI). Methylene blue reduced inflammation and microglia activation in the animals. Methylene blue reduced levels of the pro-inflammatory cytokine Il-1b and increased levels of the anti-inflammatory cytokine Il-10.
These findings are of particular interest as many patients with classical depression (and no brain injury) have abnormal levels of these inflammatory markers. It remains to be seen whether methylene blue is more helpful in those patients with elevated inflammatory markers and if levels of the markers can predict treatment response or not.
Methylene blue causes urine to turn blue, so low doses of the compound are used as a placebo. Alda and colleagues reported that the active dose 195mg reduced depression and anxiety significantly more than the placebo dose (15mg) in a 13-week crossover study. In that study, methylene blue was added to lamotrigine which had not had a complete enough effect.
In a 1986 study by G.J. Naylor and colleagues in the journal Biological Psychiatry, patients were treated with either 15mg/day or 300mg/day of methylene blue for one year and crossed over to the other dose in the second year. Participants had significantly less depression during the year of taking the active 300mg/day dose.
The FDA has issued a warning about the danger of a serotonin syndrome if methylene blue is combined with serotonin active agents (presumably because it inhibits MAO-A). Symptoms of the serotonin syndrome can include lethargy, confusion, delirium, agitation, aggression, decreased alertness, and coma. Neurological symptoms, such as jerky muscle contractions, loss of speech, muscle tension, and seizures; or autonomic symptoms, such as fever and elevated blood pressure, are also common. Patients should call their doctor if they are taking a serotonergic psychiatric medication and develop any of the above symptoms.
Anti-Inflammatory Treatments Look Promising for Bipolar Depression
Inflammation has been linked to both unipolar and bipolar depression. New research shows that anti-inflammatory treatments may reduce bipolar depression, for which few treatments exist.
Researchers led by Jonathan Savitz divided people with bipolar depression into four groups. One group received two placebos, another received minocycline (a drug with neuroprotective and immune-modulating properties) plus a placebo, the third received aspirin plus a placebo, and the final group received both minocycline and aspirin. Of the 64 participants, those who took both minocycline and aspirin were most likely to respond to treatment and to enter remission. In people with body mass indexes (BMIs) above the median of 30, a sign of greater inflammation, 100% of those who received both anti-inflammatory drugs responded to treatment, compared to 36% of those who received aspirin alone, 33% of those who received minocycline alone, and 25% of those who received two placebos.
Dosages of the drugs were 100mg twice a day for minocycline and 81mg twice a day for aspirin. Savitz and colleagues believe that aspirin and minocycline must work particularly well together, and are modifying their study to more directly compare use of the two anti-inflammatory drugs together to the absence of anti-inflammatory treatments.
Lurisadone is Effective in Mixed Unipolar Depression
Lurasidone (Latuda) has been approved by the US Food and Drug Administration (FDA) for the treatment of bipolar depression. A new study indicates that lurasidone is also effective in those with unipolar depression complicated by a few manic features, i.e. mixed depression, which is often more severe and less responsive to traditional antidepressants than traditional unipolar depression.
At a 2015 scientific meeting, Andrew Nierenberg and colleagues presented the results of a six-week study comparing 20–60 mg of lurasidone to placebo in about 200 depressed patients who had some manic symptoms. Lurasidone significantly improved unipolar depressive symptoms in addition to the mixed manic symptoms.
At baseline, the patients’ manic symptoms included: flight of ideas/racing thoughts in 66.8% of the participants, pressured speech in 61.1%, decreased need for sleep in 40.8%, increased energy or activity in 28.0%, elevated or expansive mood in 18.0%, increased or excessive involvement in pleasurable activities in 15.6%, and inflated self-esteem or grandiosity in 6.6%.
Tests of Generic Lamotrigine Successful
Studies published in 2015 and 2016 have established that generic versions of the anti-convulsant lamotrigine are bioequivalent to the name-brand drug (Lamictal) and to each other. Lamotrigine is used to treat epilepsy and is also prescribed for the prevention of bipolar depression.
An article by T.Y. Ting and colleagues in the journal Epilepsia in 2015 established that generic lamotrigine works similarly enough to the name brand drug that patients with epilepsy could be switched from one drug to the other without worsening seizures. More recently, M.D. Privitera and colleagues reported in the journal Lancet Neurology that different generic versions of lamotrigine were bioequivalent. No significant changes in seizure frequency or other negative outcomes were reported.
These studies show that generic versions of lamotrigine have the same anticonvulsant effectiveness as the original drug. The same should also be true for lamotrigine’s effectiveness in preventing bipolar depression.
Clarifying the Effects of a Diabetes Drug that Improves Bipolar Depression
Research continues on pioglitazone, a drug typically used to treat diabetes but with other positive effects on depression and stroke risk. Some researchers are working on determining whether the drug increases the risk of developing certain cancers, including bladder, prostate, and pancreatic cancers. A recent study by James D. Lewis and colleagues in the journal JAMA found no statistically significant increase in risk of bladder cancer among patients taking the drug, but the researchers said they also couldn’t rule out that the drug may increase this risk, as has been seen in previous studies. The study by Lewis did show an increase in pancreatic and prostate cancers in patients taking pioglitazone, but the researchers did not determine whether this was caused by the drug.
Another recent study by Walter N. Kernan and colleagues in the New England Journal of Medicine reported that pioglitazone reduced the incidence of stroke and heart attack in patients with a history of stroke or blocked blood vessels in the brain but without a diagnosis of diabetes. Patients who received pioglitazone also experienced side effects including weight gain, edema (an increase in fluids in the body’s tissues) and serious bone fractures.
Pioglitazone has had positive effects in bipolar depression and may one day be used as a treatment for bipolar disorder. For now, it may be worthy of consideration for the treatment of diabetes in patients who also have bipolar depression.