Lithium Safely Reduces Mania in Kids 7–17
The first large, randomized, double-blind study of lithium in children and teens has shown that as in adults, the drug can reduce mania with minimal side effects. The study by researcher Robert Findling was published in the journal Pediatrics in October. Lithium is the best available treatment for adults, but until now little research had been done on treatments for children and teens with bipolar disorder.
In the study, 81 participants between the ages of 7 and 17 with a diagnosis of bipolar I disorder and manic or mixed episodes were randomized to receive either lithium or placebo for a period of eight weeks. By the end of the study, those patients taking lithium showed greater reductions in manic symptoms than those taking placebo. Among those taking lithium, 47% scored “much improved” or “very much improved” on a scale of symptom severity, compared to 21% of those taking placebo.
Dosing began at 900mg/day for most participants. (Those weighing less than 65 lbs. were started at 600mg/day.) Dosing could be gradually increased. The mean dose for patients aged 7–11 was 1292mg/day, and for patients aged 12–17 it was 1716mg/day.
Side effects were minimal. There were no significant differences in weight gain between the two groups. Those taking lithium had significantly higher levels of thyrotropin, a peptide that regulates thyroid hormones, than those taking placebo. If thyroid function is affected in people taking lithium, the lithium dosage may be decreased, or patients may be prescribed thyroid hormone.
Lithium Has Minimal Effects On Renal Function: Results Of Two New Large Controlled Studies
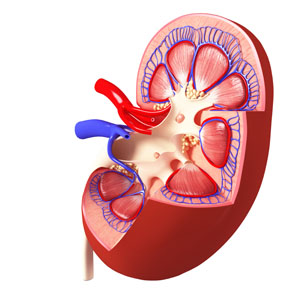 Earlier this year we described a 2015 study by Harald Aiff and colleagues that suggested that long-term lithium use was associated with a risk of kidney failure. That study, published in the Journal of Psychopharmacology, included 630 patients who had taken lithium for at least 10 years. One-third of these patients had evidence of kidney dysfunction, and in 5%, the impairment was severe. Two new studies provide some data that suggest these risks may not be lithium-specific and are comparable to risks that come with taking other medications.
Earlier this year we described a 2015 study by Harald Aiff and colleagues that suggested that long-term lithium use was associated with a risk of kidney failure. That study, published in the Journal of Psychopharmacology, included 630 patients who had taken lithium for at least 10 years. One-third of these patients had evidence of kidney dysfunction, and in 5%, the impairment was severe. Two new studies provide some data that suggest these risks may not be lithium-specific and are comparable to risks that come with taking other medications.
The first, by Stefan Clos et al. in The Lancet Psychiatry, included 1,120 patients followed for up to 12 years. On average, these patients had been exposed to lithium for a little over 4.5 years. Clos and colleagues determined patients’ estimated glomerular filtration rate (eGFR), a measure of how well the blood is filtered by the kidneys. The researchers concluded that there was “no effect of stable lithium maintenance therapy on the rate of change of eGFR over time” compared to other drugs such as quetiapine, olanzapine, or valproate.
The second new study, by Lars Vedel Kessing and colleagues in the journal JAMA Psychiatry, included 26,731 patients exposed to lithium and 420,959 exposed to anticonvulsants. Kessing and colleagues concluded that both exposure to lithium and exposure to an anticonvulsant were associated with an increased rate of chronic kidney disease, but lithium was not associated with end-stage kidney disease (the kind that requires dialysis or renal transplantation).
The three studies taken together suggest the following: Taking lithium for an average of 4–5 years does not affect kidney functioning, and longer exposure may not harm kidney function any more than other medications (such as anticonvulsants) would. However, kidney functioning (in terms of eGFR) does decline with age, and is also lower among those with higher baseline eGRF, those with other illnesses, those taking other drugs that affect the kidneys, and those who experience an episode of lithium toxicity. Read more
Saphris Reformulated for Kids with Bipolar I
The atypical antipsychotic asenapine has been reformulated for bipolar I disorder in children aged 10–17. The drug (trade name Saphris) was approved by the Food and Drug Administration (FDA) in 2009 for adults with schizophrenia and bipolar disorder. It is sometimes used as a treatment for mixed episodes (depression with some symptoms of mania).
The new formulation consists of 2.5mg tablets that are taken sublingually (under the tongue), and are available in a black cherry flavor. These can be prescribed as monotherapy for the acute treatment of manic or mixed episodes in children and teens.
RTMS for Depression Increases Volume of Specific Brain Regions
Repeated transcranial magnetic stimulation (rTMS) is a treatment for depression in which magnets placed near the skull stimulate electrical impulses in the brain. In a poster presented at the 2015 meeting of the Society of Biological Psychiatry, Martin Lan and colleagues presented results of the first study of structural changes in the brain following rTMS.
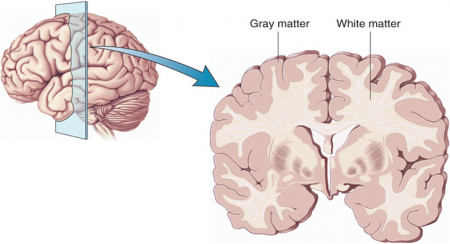
In the study, 27 patients in an episode of major depression underwent magnetic resonance brain scans before and after receiving rTMS treatment over their left prefrontal cortices. Lan and colleagues reported that several cortical regions related to cognitive appraisal, the subjective experience of emotion, and self-referential processing increased in volume following rTMS treatment: the anterior cingulate, the cingulate body, the precuneous, right insula, and gray matter in the medial frontal gyrus. The increases ranged from 5.3% to 15.7%, and no regions decreased in volume. More than 92% of the participants showed increased gray matter in all of these regions.
The brain changes were not correlated with antidepressant response to rTMS, but suggest a possible mechanism by which rTMS is effective in some people. Lan and colleagues concluded that rTMS likely had neuroplastic effects in areas of the brain that are important for emotion regulation.
N-acetylcysteine Reduces Self-Harm, Restores Amygdala Connectivity in Young Women
 N-acetylcysteine (NAC) is an anti-oxidant nutritional supplement that has been found to reduce a wide range of habitual behaviors, including drug and alcohol use, smoking, trichotillomania (compulsive hair-pulling), and gambling. It also improves depression, anxiety, and obsessive behaviors in adults, as well as irritability and repeated movements in children with autism. A new study suggests NAC may also be able to reduce non-suicidal self-injury, often thought of as “cutting,” in girls aged 13–21.
N-acetylcysteine (NAC) is an anti-oxidant nutritional supplement that has been found to reduce a wide range of habitual behaviors, including drug and alcohol use, smoking, trichotillomania (compulsive hair-pulling), and gambling. It also improves depression, anxiety, and obsessive behaviors in adults, as well as irritability and repeated movements in children with autism. A new study suggests NAC may also be able to reduce non-suicidal self-injury, often thought of as “cutting,” in girls aged 13–21.
The open study, presented in a poster by researcher Kathryn Cullen at the 2015 meeting of the Society for Biological Psychiatry, compared magnetic resonance imaging (MRI) scans of 15 healthy adolescent girls to scans of 22 girls who had been engaging in self-injury, both before and after this latter group received eight weeks of treatment with N-acetylcysteine. Doses were 1200 mg/day for the first two weeks, 2400mg/day for the next two weeks, and 3600mg/day for the final four weeks. The girls also reported their self-injury behaviors.
Treatment with NAC reduced the girls’ self-injury behaviors. The brain scans showed that NAC also increased resting-state functional connectivity between the amygdala and the insula. Connectivity in this region helps people regulate their emotional responses. At baseline, the girls who engaged in self-harm had had deficient connectivity between the amygdala, the prefrontal cortex, insula, and the posterior cingulate cortices compared to the healthy girls, and this improved with the NAC treatment.
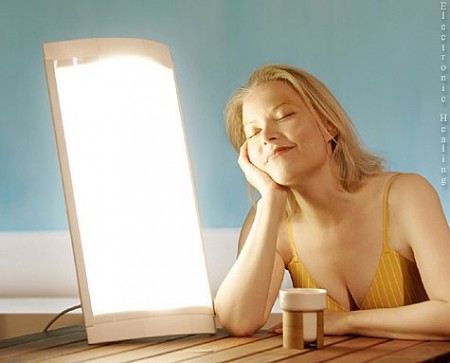
Midday Bright Light Therapy Effective in Bipolar Disorder
A recent study of 93 adults with bipolar disorder suggests that midday bright light therapy can be an effective adjunctive treatment for bipolar depression. The study by Dorothy Sit and colleagues was presented at the 2015 meeting of the Society for Biological Psychiatry. Participants had been diagnosed with bipolar I or II disorder, were in a current episode of depression, and were taking stable doses of mood stabilizing medication. They were randomized to receive either 7000-lux broad spectrum light for 45 to 60 minutes each day for six weeks or 50 lux dim red light. The comparison was dramatic: remission rates were 56.5% among those exposed to the 7000-lux light, and 14.3% among those who were exposed to the dim light. Those who received the bright light also reported better sleep quality and less suicidality.
Editor’s Note: These results are striking and raise the issue of whether midday bright light is more effective than early morning bright light, the usual recommendation for seasonal affective disorder (SAD) and other forms of depression. Until comparative studies are available, using midday light may be the way to go.
Ketamine: Equal Efficacy When Given With Lithium Or Valproate
Studies of rodents with depression-like behaviors revealed that the combination of low (sub-therapeutic) doses of lithium and infusions of ketamine produced antidepressant-like effects. Researchers believed this might mean that in humans, lithium might have a unique effect potentiating the effects of ketamine.
In a small study by Mark J. Niciu presented at the 2015 meeting of the Society for Biological Psychiatry, patients with bipolar depression taking lithium or valproate mood stabilizers were given ketamine infusions or control infusions. In the 23 patients taking lithium and the 13 taking valproate, ketamine’s antidepressant effects were significantly better than placebo, but there was no difference between lithium and valproate with regard to these antidepressant effects. These preliminary data in a small number of subjects do not support the proposition that lithium augments the effects of ketamine in depression.
Ketamine Temporarily Reduces Suicidal Thoughts
Intravenous ketamine can bring about rapid improvement in depressive symptoms among people with treatment-resistant depression. Because of its rapid effects, which can appear after only two hours, ketamine is being investigated as a treatment for people with suicidal thoughts.
At the 2015 meeting of the Society of Biological Psychiatry, Laili Soleimani and colleagues presented a poster about their recent double blind, randomized, controlled pilot study of ketamine inpatients and outpatients who scored highly on a measure of suicidal ideation. The 24 participants were randomized to receive either a single intravenous infusion of ketamine (0.5mg/kg) or a single infusion of midazolam (0.045 mg/kg), which shares ketamine’s anxiety-reducing effects but does not have antidepressant effects. They reported suicidal thoughts at 24 hours post-infusion, 48 hours, 72 hours, and 7 days. At 48 hours, those who received ketamine reported significantly reduced suicidal ideation compared to those who received midazolam, but this effect was no longer significant at the 72-hour mark.
The findings show that ketamine can briefly reduce suicidal ideation, and that the treatment is safe and tolerable for patients. This pilot study paves the way for further study of ketamine to reduce suicidal thinking in people who are at high risk for suicidal behavior.
Ketamine Improves Sleep and Reduces Suicidal Thoughts in Certain Patients
Intravenous ketamine is known for its fast-acting antidepressant effects, which can appear within two hours of an infusion. Researchers are now investigating its use for the reduction of suicidal thoughts. In a study presented in a poster at the 2015 meeting of the Society of Biological Psychiatry, Jennifer L. Vande Voort and colleagues compared the sleep of patients whose suicidal thoughts decreased after a single ketamine infusion (0.5 mg/kg over 40 minutes) to those whose suicidal thoughts remained.
Study participants whose suicidal thoughts diminished after one infusion of ketamine had better sleep quality the following night, with fewer disruptions in sleep than among those who did not have an anti-suicidal response to ketamine. The participants who responded well to ketamine had sleep quality similar to that of healthy controls.
Vande Voort and colleagues hope that these new findings about ketamine’s effect on sleep may provide clues to the biological mechanism behind ketamine’s effect on suicidal ideation.
Atypical Antipsychotics May Slow Loss of Gray Matter in Schizophrenia
Progressive losses in gray matter have been observed in the cortex of people with schizophrenia, and those at high risk for the illness. In the past, studies have shown that the amount of antipsychotics a patient is exposed to is correlated with the extent of their deficits in gray matter, suggesting that antipsychotic treatment could exacerbate gray matter loss.
A new meta-analysis by Antotonio Vita and colleagues in the journal Biological Psychiatry shows that first-generation antipsychotics were associated with greater losses in gray matter compared with atypical antipsychotics, which seemed to slow the loss of gray matter.
The meta-analysis analyzed data from 18 longitudinal studies comparing a total of 1155 patients with schizophrenia to 911 healthy control participants. Magnetic resonance imaging (MRI) scans showed that over time, patients with schizophrenia lost more cortical gray matter volume. The patients’ cumulative intake of any kind of antipsychotic between MRI scans was associated with gray matter losses. But when Vita and colleagues drilled down to find differences between patients taking first-generation antipsychotics and those taking second-generation atypical antipsychotics, they found that patients with higher average daily intake of first-generation antipsychotics had greater losses in gray matter, while patients with higher average daily intake of atypical antipsychotics had less progressive losses in gray matter.
This study is the first to compare the effects of first-generation antipsychotics, which were developed in the 1960s, with those of atypical antipsychotics, which came into frequent use in the late 1980s, on cortical gray matter loss in schizophrenia. While first-generation antipsychotics are associated with the side effect of tardive dyskinesia, involuntary movements of the face and jaw, atypical antipsychotics are most commonly associated with weight gain.
Three studies have randomly assigned patients with schizophrenia to receive either first-generation or atypical antipsychotics. In these studies as well, second-generation antipsychotics were associated with smaller losses in gray matter.
The authors speculate that either second-generation antipsychotics may have neuroprotective effects, or first-generation antipsychotics may have neurotoxic effects. They also suggest that first-generation antipsychotics may not have the capacity to interfere with the natural progression of schizophrenia in terms of gray matter losses.
Future studies may investigate differences between specific antipsychotic medications’ effects on gray matter volume. Vita and colleagues reported that in the analysis, the atypical antipsychotic clozapine was associated with the least loss of gray matter of any medication in the included studies.
Editor’s Note: This study is important because it adds to findings questioning the conclusions of a large National Institute of Mental Health–sponsored study known as CATIE and a meta-analysis by John Geddes published in the journal BMJ in 2000, in which he wrote that “There is no clear evidence that atypical antipsychotics are more effective or better tolerated than conventional (first generation) antipsychotics.” Read more