Over Half of Russian Women May Be Depressed
In a 2013 article in the journal European Psychiatry, in which researcher Valery V. Gafarov examined depression’s influence on cardiovascular health in Russia, an astonishing 55.2% of women aged 25–64 years in the study were diagnosed with depression. The study, in which 870 women in the city of Novosibirsk were surveyed over 16 years from 1995 to 2010, was part of a World Health Organization program called “MONICA-psychosocial.”
The researchers collected information on the incidence of myocardial infarction (heart attack), arterial hypertension, and stroke among the women. Over the 16 years of the study, 2.2% of the women had heart attacks and 5.1% had strokes. Women with depression were 2.53 times more likely to have a heart attack and 4.63 times more likely to have a stroke than women without depression.
Among women with average education levels, married women with depression were more likely to have heart attacks, hypertension, and strokes. Hypertension was more likely among women who worked as managers or light manual laborers.
N-acetylcysteine May Improve Prodromal Schizophrenia
 At the 2014 meeting of the International College of Neuropsychopharmacology, researcher N. Miyake described the effects of the nutritional supplement n-acetylcysteine (NAC) on clinical symptoms in subjects with subthreshold symptoms of psychosis.
At the 2014 meeting of the International College of Neuropsychopharmacology, researcher N. Miyake described the effects of the nutritional supplement n-acetylcysteine (NAC) on clinical symptoms in subjects with subthreshold symptoms of psychosis.
N-acetylcysteine, a glutathione precursor, has neuroprotective effects. In this case series, four patients with subthreshold psychosis were given 2000mg/day of NAC for 12 weeks. The patients’ symptoms improved to the point that three of the four were no longer considered at risk for psychosis.
Editor’s Note: These promising anecdotal observations deserve careful follow up using a control group. Omega-3 fatty acids have been show to slow conversion to full psychosis and performed better than placebo in a controlled study. Both n-acetylcysteine and omega-3 fatty acids should definitely be studied for those with emerging symptoms of bipolar disorder.
CRP, A Readily Available Marker of Inflammation, Predicts Response To Two Antidepressants
C-reactive protein, or CRP, is a protein found in blood plasma, the levels of which rise in response to inflammation. In a recent study, levels of CRP were able to predict which of two antidepressants a patient was more likely to respond to.
The 2014 article by Rudolph Uher et al. in the American Journal of Psychiatry reported that low levels of CRP (<1 mg/L) predicted a good response to the selective serotonin reuptake inhibitor (SSRI) escitalopram (Lexapro) while higher levels of CRP predicted a good response to the tricyclic antidepressant nortriptyline, a blocker of norepinephrine reuptake.
The research was part of the Genome-Based Therapeutic Drugs for Depression (GENDEP) study, a multicenter open-label randomized clinical trial. CRP was measured in the blood of 241 adult men and women with major depressive disorder. In the article the researchers say that CRP and its interaction with medication explained more than 10% of the individual variance in response to the two antidepressants.
If these findings can be replicated with these and similarly acting drugs, it would be a very large step in the direction of personalized medicine and the ability to predict individual response to medications.
Another promising open study of minocycline in bipolar depression
Joanna Soczynska in Roger McIntyre’s lab at the University of Toronto presented a poster at the 2014 meeting of the International College of Neuropsychopharmacology (CINP) on the anti-inflammatory and neuroprotective antibiotic minocycline.
Twenty-seven patients with a major depression received minocycline in addition to the medications they were already being prescribed. Dosage was 100mg twice a day. Treatment with adjunctive minocycline was associated with significant improvement on several scales that measure depression severity.
Editor’s Note: What was particularly interesting was that a subset of patients achieved complete remission, raising the question whether these patients might have markers of inflammation that would predict this excellent response. The authors concluded that the “results provide a rationale for testing minocycline’s efficacy in a larger randomized, placebo-controlled trial.”
Exactly this type of study was proposed a year ago by researcher Andy Nierenberg and given the best marks by a National Institute of Mental Health review committee but was turned down for funding because the National Institute of Mental Health has implemented a new initiative, Research Domain Criteria (RDoC), that lays out new criteria for research, limiting funding to those studies that focus on a molecular target that spans several diagnoses.)
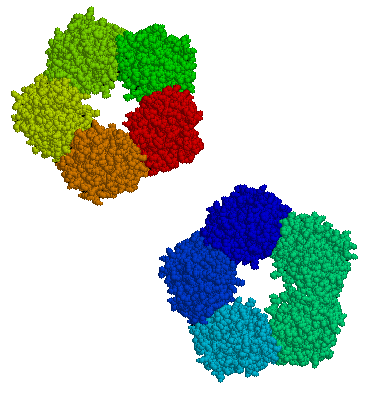
In Mice, Autism-Like Behavior Connected to Problems Pruning Dendritic Spines
Autism spectrum disorders are associated with developmental abnormalities at excitatory synapses. Dendrites, the branched projections of neurons where electrical signals are passed from one cell to the next, are covered in hundreds to thousands of spines that facilitate the synaptic connections with other neurons. These spines are created and also pruned as part of normal learning and development.
Post-mortem examination of the brains of patients with autism spectrum disorders shows increased density of dendritic spines and less pruning in certain neurons in the temporal lobe. These examinations also show impaired mTOR autophagy. MTOR is a protein that plays a role in cell growth and survival. Autophagy is the normal process by which some components of cells are broken down.
A 2014 study by Guomei Tang et al. in the journal Neuron showed that mice that are genetically altered to have overactive mTOR also have reduced dendritic spine pruning, blockade of autophagy, and increased autism-like behaviors. An immunosuppressant drug called rapamycin inhibits mTOR, and treating the mice with this drug corrected the problems with spine pruning and the autism-like behaviors. (This was not true for mice who had been altered to have another type of autophagy.) Normal spine formation was not affected by the restored pruning ability.
Tang et al. concluded that mTOR autophagy plays an important role in dendritic spine pruning, and that restoring neuronal autophagy can correct synaptic abnormalities and restore normative social behavior in mice with hyperactive mTOR.
Thalamus Implicated in Depression-Like Behavior and Resilience to It
At the 2014 meeting of the International College of Neuropsychopharmacology, researcher Scott Russo described characteristics of rodents who showed depression-like behavior after 10 days of exposure to a larger, more aggressive animal (a phenomenon known as defeat stress). These animals exhibited many behaviors that resembled human depression, including anxiety-like behaviors while navigating a maze; activation of the hypothalamic-pituitary-adrenal axis; circadian rhythm abnormalities; metabolic changes such as glucose intolerance; susceptibility to addiction; anhedonia, a lack of interest in sucrose, sex or intracranial self-stimulation; and profound and permanent social avoidance.
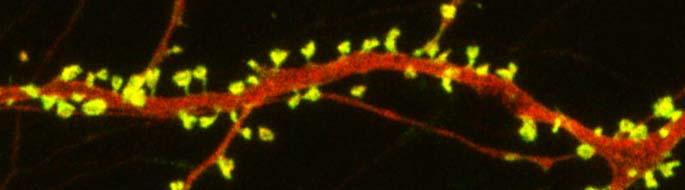
In susceptible animals, Russo found anatomical changes in the GABAergic neurons of the nucleus accumbens (also known as the ventral striatum), including increased numbers of synapses and a greater number of stubby spines on dendrites (the branched projections of neurons where electrical signals are passed from one cell to the next), as well as greater excitability of glutamatergic input, observed as excitatory post-synaptic potentials.
Russo’s attempt to identify these key neurons among the billions of neurons and the 100 to 500 trillion synapses in the brain was like the search for a needle in a haystack, but thinks he found it. The medium spiny neurons of the nucleus accumbens contain GABA and receive synapses from the prefrontal cortex, amygdala, and intralaminar nucleus of the thalamus (ILT), in addition to dopamine inputs from the VTA, and cholinergic, somatostatin, and orexin inputs. Russo found that it was the ILT inputs that conveyed susceptibility to defeat stress, and their presynaptic endings showed increased levels of glutamate transporters (VGLUT-2). Driving the ILT was sufficient to cause the rodents to display the depression-like behaviors, and silencing the ILT during defeat stress prevented the susceptible behaviors (like social avoidance) and promoted resilience.
Acute Steroid Injection May Ward Off PTSD
Low cortisol after a trauma is a risk factor for developing chronic post-traumatic stress disorder (PTSD). Researcher Joseph Zohar studied has been researching the effects of steroids on the development of PTSD and presented some findings at the 2014 meeting of the International College of Neuropsychopharmacology.
Twenty-five patients who experienced a traumatic event and showed acute stress symptoms were given either a single high-dose injection of hydrocortisone (100–140 mg) or a placebo within six hours of the trauma. Follow-up evaluation took place after two weeks, one month, and three months. Those who received this single high dose of hydrocortisone had lowered stress symptoms and less subsequent PTSD compared to those who received placebo.
Digestion of Wheat and Milk Releases Peptides that Might Cause Inflammation
Some people have found that gluten-free or casein-free diets have improved their intestinal, autoimmune, or neurological symptoms. (Casein is a protein found in mammals’ milk. Cow milk is high in casein while human milk proteins are 20–45% casein.) One explanation for the good effects of these diets is that peptides that are released during digestion of these foods can create epigenetic changes in gene expression, adding methyl groups to DNA strands that increase inflammation.
As infants transition from getting all of their nutrition from the placenta to using their gastrointestinal tract, their diet may lead to epigenetic modifications that affect their health later in life. Epigenetics refers to changes in genes that do not affect the inherited sequence of DNA, but affect how easily the DNA is transcribed to produce proteins. Methyl or acetyl groups can be added to DNA or the histones around which it is wound.
When a person digests casein (from either human or animal milk) or gliaden (a protein derived from wheat), peptides are released that activate opioid receptors, modulating the uptake of the amino acid cysteine in neurons and in the gastrointestinal tract. This decrease in cysteine uptake is associated with drop in the antioxidant glutathione and a methyl donor (a molecule with a reactive methyl group that can easily become part of another molecule) called S-Adenosyl methionine.
In addition to decreasing cysteine uptake, the peptides also increase DNA methylation and create epigenetic changes in genes involved in redox (changes in oxidation) and methylation homeostasis.
These processes are described in a 2014 article by Malav S.Trivedi et al. in the Journal of Nutritional Biology. Trivedi et al. conclude that milk and wheat can change antioxidant activity and gene expression. Differences in the peptides in human and cow milk may explain developmental differences between children who are breastfed and those who receive formula.
The decrease in antioxidants caused by peptides from wheat and milk can predispose people to inflammation and oxidation, explaining why wheat- or casein-free diets might be useful.