How Illness Progresses In The Recurrent Affective Disorders
This editor (RM Post) in collaboration with Jacqueline Fleming and Flavio Kapczinski published the article “Neurobiological mechanisms of illness progression in the recurrent affective disorders” in the Journal of Psychiatric Research this year. The article built on several themes about the progression of bipolar illness that had been explored in previous research.
These themes include:
- The likely acceleration of repeated episodes as a function of the number of prior episodes (episode sensitization)
- The increased responsivity of the illness to repeated stressors (stress sensitization)
- The increased behavioral reactivity to repeated use of psychomotor stimulants such as cocaine (stimulant-induced behavioral sensitization)
Not only are these observations well documented in the scientific literature, but recent observations also suggest that each type of sensitization can show cross-sensitization to the other two types. That is, individuals exposed to repeated stressors are more likely both to experience affective illness episodes and to adopt comorbid substance abuse. In a similar way, episodes of an affective disorder and stressors may also be associated with the relapse into drug administration in those who have been abstinent.
In addition to these mechanisms of illness progression in the recurrent affective disorders, the new article reviews the literature showing that the number of affective episodes or the duration of the illness appear to be associated with a variety of other clinical and neurobiological variables.
The number of affective episodes a patient experiences is associated with the degree of cognitive dysfunction present in their bipolar illness, and experiencing more than 4 episodes of unipolar or bipolar depression is a risk factor for dementia in late life. A relative lack of response to most treatments is also correlated with the number of prior episodes, and this holds true for response to naturalistic treatment in general. While most of these data are correlational and the direction of causality cannot be ascertained for certain, it is likely that the number of affective episodes and/or their duration could account for and drive difficulties with treatment and with cognitive function.
If this were the case, one would expect to see a variety of neurobiological correlates with the number of prior episodes or duration of illness, and in the article we summarize those that have been found in unipolar and bipolar disorder. Considerable data indicate that cortical volume and degrees of prefrontal cortical dysfunction can vary as a function of number of prior episodes. There is evidence that increased activity of the amygdala and the nucleus accumbens are also related to episodes or duration of illness. In those with unipolar depression, the volume of the hippocampus is decreased with longer duration of illness. Read more
Genetic Risk Factors for Onset of Bipolar Disorder
A Genetic Risk Factor For Bipolar Disorder: The CACNA1C Gene
In an abstract presented at the 5th Biennial Conference of the International Society for Bipolar Disorders, Sophia Frangou reported on the CACNA1C polymorphism, a genetic variation that has been associated with the risk of developing bipolar disorder in several genome-wide association studies that search for links between genes and illnesses. Frangou found that those people with the genetic variation had increased volume in some parts of the brain, including the right hypothalamus and the right amygdala, and decreased volume in others, including the putamen, as well as alterations in the functional connectivity of different cortical areas.
These data may be related to findings that calcium influx may play a role in bipolar disorder. In people with the genetic variation, the risk allele binds to a subunit of the voltage-dependent calcium channel, which modulates the influx of calcium from the outside to the inside the neuron.
Increased amounts of calcium are consistently found in the white cells and platelets of patients with bipolar disorder compared to controls. Moreover, the drug nimodipine, a dihydropyridine L-type calcium channel blocker, is effective in the prevention of manic and depressive episodes in a subgroup of patients, particularly those with cycling patterns that are ultra-rapid (4+ episodes per month) or ultradian (including a mood switch within a 24-hour period 4+ times per month). A large randomized study of patients with bipolar disorder presented by H.R. Chaudhry at the 2010 meeting of the Society of Biological Psychiatry also found that while lithium was associated with a 50% response rate, the combination of lithium and nimodipine was associated with a 73% response rate, again suggesting the additional efficacy of blocking L-type calcium channels.
Immune Abnormalities May Predict Onset of Bipolar Disorder in Children at High Risk
At the 5th Biennial Conference of the International Society for Bipolar Disorders E. Mesman discussed connections between immunity and bipolar disorder. Mesman and colleagues followed offspring of parents with confirmed bipolar disorder for 12 years and compared them to children in the general population. In the children of bipolar parents they found higher levels of immune markers called cytokines (PTX3 and sCD25) in circulating monocytes, a type of white blood cell. In the children of bipolar parents they also found a high inflammatory setpoint in the monocytes. T-effector and T-regulatory cells were also different in the offspring of bipolar parents.
While these findings were present in children who had already become ill with bipolar disorder, they were also present in those who had yet to experience a mood disorder, suggesting that these immune and inflammatory markers may ultimately be an important risk marker for the onset of bipolar disorder.
Editor’s Note: These are among the first studies suggesting that immune and inflammatory abnormalities may precede the onset of bipolar disorder. Many studies have shown that patients with active bipolar disorder show more inflammation, including increases in inflammatory markers interleukin 1 (IL-1), interleukin 6 (IL-6), C reactive protein (CRP), and tumor necrosis factor alpha (TNFa). The new data are of considerable importance not only because inflammation could serve as a marker of illness onset, but also because inflammation could become a potential target for therapeutics (i.e. using anti-inflammatory and immune-suppressing agents to treat bipolar disorder).
Inflammation and Mood Disorders
There is increasing evidence of a link between inflammation, brain function, and treatment resistance in the mood disorders. Obesity is also linked to inflammatory processes and thus may contribute to the development of treatment resistance in both unipolar and bipolar mood disorders.
Causes of Inflammation
 Obesity is one factor that can lead to increases in inflammation. When people gain weight, the size of fat cells can increase to the point that the cells are deprived of oxygen and disintegrate. Then macrophages and other cells come in to sweep up the remaining particles of the fat cells. These scavenger cells then become activated and produce more regulatory chemicals called cytokines. The cytokines produced in the periphery (in the body outside the brain) can then enter the brain and affect brain function in a process that may ultimately be linked to fatigue, depression, and other adverse mood and behavior states that contribute to treatment resistance. There is a two-way street: the brain can influence the body and what goes on in the body can influence the brain.
Obesity is one factor that can lead to increases in inflammation. When people gain weight, the size of fat cells can increase to the point that the cells are deprived of oxygen and disintegrate. Then macrophages and other cells come in to sweep up the remaining particles of the fat cells. These scavenger cells then become activated and produce more regulatory chemicals called cytokines. The cytokines produced in the periphery (in the body outside the brain) can then enter the brain and affect brain function in a process that may ultimately be linked to fatigue, depression, and other adverse mood and behavior states that contribute to treatment resistance. There is a two-way street: the brain can influence the body and what goes on in the body can influence the brain.
Other factors that can lead to increases in inflammation and eventually to treatment resistance in the unipolar and bipolar mood disorders include early life stress, medical illness, and anxiety and personality disorders.
Anti-Inflammatory Treatments
Given the close links between inflammation and depression (discussed in BNN Volume 15, Issue 1 from 2011), Andrew H. Miller of Emory University decided to test a specific anti-inflammatory agent called infliximab (a TNF monoclonal antibody that inhibits TNF alpha actions) as an antidepressant. One sign of inflammation is a C-reactive protein (CRP) level of 2mg/L or greater. The effect of infliximab on the population of treatment refractory depressed patients who participated in Miller’s study was not significant on the whole, but the drug did have significantly greater antidepressant effects than placebo in those patients with the highest levels of CRP. The investigators believe this demonstrates the principle that a drug that inhibits TNF alpha may be useful in patients with the greatest degree of inflammation.
Other approaches to anti-inflammatory mechanisms are also being pursued, including use of aspirin, COX-2 inhibitors, and the antibiotic minocycline. Minocycline has anti-inflammatory and neuroprotective effects and has been reported to have positive effects in cognition and negative symptoms of schizophrenia.
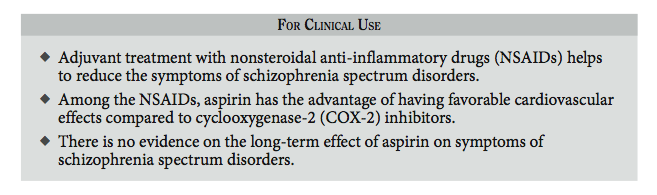
Aspirin May Help Reduce Schizophrenia Symptoms
An article by Laan et al. published in the Journal of Clinical Psychiatry in 2010 suggested that aspirin may reduce symptoms of schizophrenia spetrum disorders in patients being treated with antipsychotics.
Aspirin is an anti-inflammatory drug. We’ve written before about the possible use of aspirin in bipolar disorder and about the role of inflammation in mental illness.
BDNF Related to Cognition and Fitness in Men with Coronary Artery Disease
 At the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011, Walter Swardfager and colleagues from Toronto, Ontario presented a study indicating that brain-derived neurotrophic factor (BDNF) concentrations in blood are associated with cognitive performance and cardiopulmonary fitness in people with coronary artery disease.
At the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011, Walter Swardfager and colleagues from Toronto, Ontario presented a study indicating that brain-derived neurotrophic factor (BDNF) concentrations in blood are associated with cognitive performance and cardiopulmonary fitness in people with coronary artery disease.
In 88 mostly male subjects with a mean age of 63 years, cardiopulmonary fitness was directly correlated with BDNF in blood as well as higher scores of cognition on two tests, the mini mental status exam and the digit symbol coding task. The investigators concluded that better fitness, psychomotor processing speed, and overall cognition were consistent with a hypothesis that BDNF protects midbrain dopaminergic neurons against inflammatory neurodegenerative processes.
Blood levels of interleukin 6, a measure of inflammatory cytokines, were associated with lower mini mental status scores in a multivariate analysis that controlled for BDNF levels.
Editor’s note: BDNF appears to be necessary for long-term learning and memory. Meta-analyses indicate that BDNF levels are low in depression and improve with euthymia. Many mood stabilizers including lithium, valproate, carbamazepine, and lamotrigine and most types of antidepressants are able to increase BDNF. The current findings linking BDNF with better cardiopulmonary fitness and cognition continue to emphasize the potential importance of BDNF beyond its role as a marker for depression.
In BNN Volume 12, Issue 3 from 2008, we reported on the data of Schmidt and Duman, which indicated that BDNF administered in a subcutaneous minipump is able to reverse many depressive-like behaviors in an animal model of depression, suggesting that even peripheral BDNF may have a role in the central nervous system.
Diet, Depression, Inflammation and the Brain
We’ve been posting recently about diet and about treatments that are weight-neutral. There is evidence that diet, inflammation and depression are all linked. Epidemiological studies by Joe Hiblen have shown that in countries whose populations eat more fish and thus have high levels of omega-3 fatty acids in their diet, there is lower incidence of depression, suicide, and cardiovascular disease such as heart attacks and strokes. This may be because the major omega-3 fatty acids, EPA and DHA, are anti-inflammatory, and inflammation has been linked to depression. EPA inhibits the enzymes phospholipase A2 and cyclo-oxygenase-2 (COX-2), and their subsequent inflammatory effects on cytokines. DHA inhibits the pro-inflammatory cytokine IL6.
Researcher John Davis recently reviewed relevant literature and found that diets high in anti-inflammatory omega-3 fatty acids are associated with lower incidence of depression, cardiovascular disease, and markers of inflammatory processes. Conversely, diets high in fat and in inflammatory omega-6 fatty acids are associated with obesity, depression, and cardiovascular disease.
Various studies have shown the links between inflammation and depression. For example, when patients are given alpha-interferon to treat viral hepatitis, there is a subsequent increase in inflammatory cytokines IL-1 and IL-6, and depression often follows. Also, depressed patients have an increased ratio of pro-inflammatory to anti-inflammatory cytokines in their blood.
Another sign of a link between bipolar illness and inflammation can be seen in biochemical analysis of brain specimens obtained at autopsy. Researcher Rapaka Rao in the laboratory of Stanley Rapoport at the National Institute on Aging at the National Institutes of Health in Bethesda, Maryland, has reported that increased markers of neuronal inflammation and excitotoxicity were found in the brains of people who had had bipolar disorder. Phospholipase A2 and COX-2 were significantly elevated in the brains of those with bipolar illness and those with schizophrenia compared with controls. Pro-inflammatory interleukin I was also significantly increased in the brains of those who had had either illness. Read more
The Evolving Omega-3 Fatty Acid Story: The Icing on the Cake (And Why It Shouldn’t Be Eaten)
 Omega-3 fatty acids are important for brain development and function and are essential to the human diet since they cannot be synthesized by the body. Omega-3 fatty acids are derived from canola oil, walnuts, flax seed oil, leafy vegetables, and especially fish. The main omega-3 fatty acids include eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). They have anti-inflammatory effects, unlike omega-6 fatty acids, which are pro-inflammatory. The omega-6 fatty acids come from soy, peanuts, corn oil, and meats, and are associated with increases in obesity, myocardial infarction, and stroke.
Omega-3 fatty acids are important for brain development and function and are essential to the human diet since they cannot be synthesized by the body. Omega-3 fatty acids are derived from canola oil, walnuts, flax seed oil, leafy vegetables, and especially fish. The main omega-3 fatty acids include eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). They have anti-inflammatory effects, unlike omega-6 fatty acids, which are pro-inflammatory. The omega-6 fatty acids come from soy, peanuts, corn oil, and meats, and are associated with increases in obesity, myocardial infarction, and stroke.
In a recent review of the literature, John Davis and Joe Hiblen found that diets that include high levels of omega-3 fatty acids are associated with decreased incidence of depression, suicide, and cardiovascular disease. The researchers performed a meta-analysis of all the prospective depression treatment studies of omega-3 fatty acids compared to placebo. They found that EPA had antidepressant effects in humans, with moderate effect size and a high degree of statistical significance. DHA, however, did not appear to have an antidepressant effect, and pure DHA was even associated with some worsening of depression.
Editor’s note: This meta-analysis helps clarify some of the ambiguities in the literature about the antidepressant efficacy of the omega-3 fatty acids, clarifying that EPA alone is an effective antidepressant. The one study that did not find antidepressant effects with EPA was carried out by the Bipolar Collaborative Network, in which I am an investigator. Our study, published in an article by Keck et al., showed that 6g of EPA was not significantly more effective than placebo in bipolar depression or in rapid cyclers. However, there is some indication that 6g may be too high a dose of EPA, and most of the recommendations now suggest using 1-2g of either EPA or an EPA/DHA combination. Read more
Early Life Stressors Linked to Persistent Inflammation and Endocrine Abnormalities
Epigenetics is a relatively new area of study that examines changes in DNA regulation and structure that can come about as a result of environmental events, as opposed to the genetic inheritance (DNA sequence) people receive through their parents’ genes. Epigenetic effects occur when an environmental stressor or chemical causes methyl or acetyl groups to attach to DNA or to histones (around which DNA are wound). These epigenetic changes determine how difficult it is to turn on genes coded in the DNA (see here for more information about the way the environment produces these epigenetic effects).
After the jump: Several studies presented at the 65th Annual Scientific Convention of the Society of Biological Psychiatry earlier this year suggested a link between environmental stress and both inflammation and abnormalities in DNA.
 Read more
Read more
Inflammation and Oxidative Stress in Bipolar Disorder
A number of studies presented at the 4th Biennial Conference of the International Society for Bipolar Disorders conference in Sao Paulo, Brazil in March reported new data relevant to inflammation and oxidative stress. Both inflammation and oxidative stress increase risk of cardiovascular disorders, and patients with inadequately treated mood disorders lose 10 or more years of life expectancy from cardiovascular disorders compared to the general population. Inflammation and oxidative stress may also contribute to the symptoms, evolution, and progression of the mood disorders themselves.
It is possible that these two processes could become new targets for therapeutic intervention in addition to more traditional psychopharmacological drugs that primarily target the neurotransmitters dopamine, norepinephrine, serotonin, and the neurotrophic factor BDNF. Read more
Inflammation in the Affective Disorders
Bipolar children exhibit more inflammation than healthy children, according to a paper presented by Pandey, Dwivedi, and Pavuluri from the University of Illinois at the American College of Neuropsychopharmacology in December 2009.
In “Pro-inflammatory cytokines in plasma of patients with pediatric bipolar disorder,” the researchers described their study in which 21 normal controls were compared with 22 children with pediatric bipolar disorder who were unmedicated for a period of at least two weeks. The level of the inflammatory cytokine interleukin-1b (IL-1b) was significantly higher in the pediatric bipolar patients compared with controls, and levels of TNF alpha, another inflammatory marker, were significantly higher as well. Not only is this evidence of increased inflammatory processes in pediatric bipolar disorder, but TNF alpha is associated with activation of transcription factors and the initiation of preprogrammed cell death, or apoptosis.