Serotonin is Back
A review by Moncrieff et al in Molecular Psychiatry 2022 concluded that : “there is no convincing evidence that depression is associated with, or caused by, lower serotonin concentrations or activity.” This was widely reported in the news media.
A new analysis by 26 experts in the field finds many faults with this analysis (Jauhar et al 2023). Instead, they conclude “A more accurate, constructive conclusion would be that acute tryptophan depletion and decreased plasma tryptophan in depression indicate a role for 5-HT in those vulnerable to or suffering from depression, and that molecular imaging suggests the system is perturbed. The proven efficacy of SSRIs in a proportion of people with depression lends credibility to this position.” Long live serotonin’s role in depression.
Probiotic as an adjunct to an antidepressant
Viktoriya L. Nikolova, et al reported in JAMA Psychiatry (2023) that the probiotic Bio-Kult Advanced; ADM Protexin was more effective than placebo as an adjunct to antidepressants for depression and anxiety.
Risk of Attempted or Completed Suicide in Borderline Personality Disorder: Reduced with ADHD meds; Increased with Benzodiazepines
Johannes Lieslehto et al 2023 reported in JAMA New. Open on the comparative effectiveness in 22,601 individuals with BPD that “ADHD medication was the only pharmacological treatment associated with reduced risk of suicidal behavior among patients with BPD. Conversely, the findings suggest that benzodiazepines should be used with care among patients with BPD due to their association with increased risk of suicide.” Mood stabilizers had no effect while antipsychotics minimally and antidepressants moderately increased risk of suicide attempts or completed suicide.
Single-dose psilocybin-assisted therapy in major depressive disorder: a placebo-controlled, double-blind, randomized clinical trial
von Rotz et al reported in eClinical Medicine (the Lancet) that a single dose of psilocybin produced a huge AD (anti-depressant) effect compared to placebo. A dose of 0.215mg Kg (about 15mg for a 70kg person) had a rapid onset AD effect that persisted for at least 14 days. Music was played and in a living room like environment. Psychological support was provided on 3 visits pretreatment and on days 8 and 14 for a total of 14 hours
Abuse Histories Decrease Rate of Remission to Antidepressant Treatment
Harkness et al reported in The Canadian Journal of Psychiatry (2023) “Greater severity of emotional maltreatment perpetrated by the mother was a significant and direct predictor of lower odds of week 16 remission (odds ratio [OR]=1.68, P =0.02). In contrast, the relations of paternal-perpetrated emotional maltreatment and physical maltreatment to week 16 remission were indirect, mediated through greater severity of anhedonia at week 8.”
Editors note: Response to ADs is less good in those with a history of abuse in childhood. Therefore psychotherapy should be added to medications in such situations to attempt to enhance responsiveness.
U.S. FDA Approves VRAYLAR® (cariprazine) as an Adjunctive Treatment for Major Depressive Disorder
“A Phase 3 Study 3111-301-001 showed a clinically and statistically significant change from baseline to week six in the Montgomery-Åsberg Depression Rating Scale (MADRS) total score for patients treated with cariprazine at 1.5 mg/day + ADT compared with placebo + ADT. A second registration-enabling study, RGH-MD-75, showed a clinically and statistically significant change from baseline to week eight in the MADRS total score for patients treated with cariprazine at 2-4.5 mg/day (mean dose 2.6 mg) + ADT compared with placebo + ADT.
Cariprazine was generally well tolerated in 6- and 8-week studies. Mean weight change was < 2lbs and ? 3% of patients had a weight increase of ? 7%.
The starting dosage of VRAYLAR is 1.5 mg once daily. Depending upon clinical response and tolerability, the dosage can be increased to 3 mg once daily on Day 15. In clinical trials, dosage titration at intervals of less than 14 days resulted in a higher incidence of adverse reactions. The maximum recommended dosage is 3 mg once daily.
Most common adverse reactions observed in the adjunctive MDD studies (? 5% and at least twice the rate of placebo) were:
Akathisia, nausea, and insomnia at the recommended doses in 6-week, fixed-dose trials
Akathisia, restlessness, fatigue, constipation, nausea, increased appetite, dizziness, insomnia, and extrapyramidal symptoms in one 8-week flexible-dose trial at a titration of less than 14 days”
First and Only Oral NDMA Receptor Antagonist for MDD Can Now Be Prescribed
| October 28, 2022 |
| FEATURED NEWS: First and Only Oral NDMA Receptor Antagonist for MDD Can Now Be Prescribed Extended-release dextromethorphan HBr-bupropion HCl (Auvelity™), the only oral N-methyl D-aspartate (NMDA) receptor antagonist approved for the treatment of major depressive disorder (MDD), is now available by prescription in the United States, maker Axsome Therapeutics Inc. announced. The drug is supplied in 105-mg tablets in 30-count bottles.On August 18th, 2022, the US Food and Drug Administration (FDA) approved dextromethorphan HBr-bupropion HCl extended-release tablets 45mg/105mg |
Scientific Mechanisms of Rapid-Acting Antidepressants
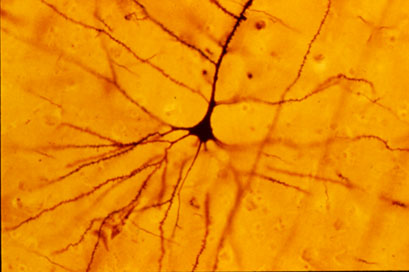
A pyramidal cell (Photo by Bob Jacobs, Laboratory of Quantitative Neuromorphology Department of Psychology Colorado College)
At a recent symposium, researcher Francis McMahon provided electrophysiological evidence that several different types of rapid-acting antidepressants—low-dose ketamine, scopolamine, and rapastinel (a partial agonist of the neurotransmitter NMDA)—act by decreasing the inhibitory effects of GABAergic interneurons on excitatory neurons called pyramidal cells, thus increasing synaptic firing.
Researcher Ronald Duman further dissected these effects, showing that ketamine and its active metabolite norketamine reduce the steady firing rate of GABA interneurons by blocking NMDA receptors, while the partial agonist rapastinel acts on the glutamate neurons directly, and both increase the effects of a type of glutamate receptors known as AMPA. These effects were demonstrated using a virus to selectively knock out GluN2B glutamate receptor subunits in either GABA interneurons or glutamate neurons.
Increasing AMPA activity increases synapse number and function and also increases network connectivity, which can reverse the effects of stress. Duman and colleagues further showed that when light is used to modulate pyramidal cells (a process called optogenetic stimulation) in the medial prefrontal cortex, different effects could be produced. Stimulating medial prefrontal cortex cells that contained dopamine D1 receptors, but not D2 receptors, produced rapid and sustained antidepressant effects. Conversely, inhibiting these neurons blocked the antidepressant effects of ketamine. Stimulating the terminals of these D1-containing neurons in the basolateral nucleus of the amygdala was sufficient to reproduce the antidepressant effects. These data suggest that stimulation of glutamate D1 pyramidal neurons from the medial prefrontal cortex to the basolateral nucleus of the amygdala is both necessary and sufficient to produce the antidepressant effects seen with ketamine treatment.
Researcher Hailan Hu reported that NMDA glutamate receptors drive the burst firing of lateral habenula (LHb) neurons, which make up the depressogenic or “anti-reward center” of the brain and appear to mediate anhedonic behavior (loss of interest or enjoyment) in animal models of depression. Ketamine blocks the burst firing of the LHb neurons, which disinhibits monoamine reward centers, enabling ketamine’s rapid-onset antidepressant effects. This may occur because inhibitory metabotropic glutamate receptors (mGluR-2) are activated, decreasing the release of glutamate.
MGluR-2 may also help explain the antidepressant effects of acetyl-L-carnitine supplements. L-carnitine is an amino acid that is low in the blood of depressed patients. The supplement acetyl-L-carnitine (ACL) activates the DNA promoter for mGluR-2, increasing its production and thus decreasing excess glutamate release. The acetyl group of the ACL binds to the DNA promoter for mGluR-2, thus this process seems to be epigenetic. Epigenetic mechanisms affect the structure of DNA and can be passed on to offspring even though they are not encoded in the DNA’s genetic sequence.
Risk of Suicide in People with Bipolar Disorder: Lowest with Lithium, Highest with Antidepressants
Researcher Markku Lähteenvuo and colleagues reported in the journal JAMA Psychiatry in early 2018 that long-acting injectable antipsychotics and lithium were best at preventing re-hospitalization in 18,018 bipolar patients in Finland who received an average of more than 7 years of follow up. Lähteenvuo and colleagues have now gone on to analyze suicide data from the same cohort of patients with bipolar disorder, and report that those taking lithium had the lowest rate of suicide, while those taking valproate had the next lowest suicide rate. Those patients with bipolar disorder who were treated with antidepressants had the greatest suicide rate. The suicide rate was particularly high for those once-hospitalized patients taking the MAO inhibitor antidepressant meclobemide, which is not approved for use in the US. Increased rates of suicide were also seen with use of sedatives and benzodiazepines.
Editor’s Note: Evidence continues to mount that lithium should be the definitive first line therapy in bipolar disorder for a multitude of reasons (as this editor Robert M. Post reviewed in an open-access article in the journal Neuropsychopharmacology in 2017). Still, lithium is not often prescribed for people with bipolar disorder in the US, and this does not seem to be in these patients’ best interests.
Use of antidepressants in bipolar disorder has remained controversial, but it is common in clinical practice despite a lack of evidence that it is effective, and the presence of some evidence that it is actually harmful. Antidepressant use in a person with bipolar disorder may cause switching into mania, cycle acceleration, dysphoria induction, and even suicide.
Clinicians should take these data seriously and overcome the impulse (leftover from treating unipolar depression) to use unimodal antidepressants as first line or adjunctive therapy for bipolar depression. Antidepressants are only effective in the long term in about 15% of patients with bipolar depression, and now it appears antidepressant use also carries an additional risk of suicide.
Inflammation is Associated with Antidepressant Treatment Resistance
Researcher Ebrahim Haroon and colleagues report in a 2018 issue of Psychoneuroendocrinology that people whose depression failed to respond to at least three different antidepressants in their current episode of depression had higher levels of inflammation than those who had fewer than three failed antidepressant trials.
The researchers found that patients who had not responded to antidepressants had higher levels of the inflammatory markers TNF-alpha, TNF-alpha receptor 2, and Il-6. The inflammatory marker CRP was also significantly elevated in these patients when statistical analyses that excluded body mass index (BMI) were used.
Haroon and colleagues reported that a third of all patients with major depressive disorder fail to respond to currently available antidepressant treatments, and that inflammation may be to blame because it interferes with the neurotransmitter systems that antidepressants target.
Editor’s Note: These data indirectly support the use of anti-inflammatory drugs to augment the effects of antidepressants in patients with treatment resistant depression. A caution that may be very important is to assess evidence of inflammation at baseline, as some data suggest that people with low CRP may, for example, do more poorly with a blocker of TNF-alpha, while people with high CRP at baseline (over 3 pg/ml) show good improvement.



